Ringworm, known medically as dermatophytosis or tinea, is a very common skin infection caused by a fungus, not a worm as its name misleadingly suggests.
The name originates from the characteristic ring-shaped, red, and itchy rash that often forms on the skin.
This condition is far more prevalent than many realize.
In fact, fungal skin infections are a global health issue, with estimates from the U.S. Centers for Disease Control and Prevention (CDC) suggesting that up to 25% of the world’s population may contract a ringworm infection at some point in their lives.
While typically not life-threatening, ringworm can be intensely uncomfortable, persistent, and highly contagious.
This guide will provide a comprehensive overview of the different types of ringworm, how to accurately identify its symptoms, the most effective evidence-based treatments, how it spreads, and crucial prevention strategies to protect yourself and your family.
Dive into this complete guide to understand everything you need to know about identifying, treating, and preventing this common fungal infection.
In This Article
Part 1: Understanding the Basics of Ringworm (Dermatophytosis)
Before diving into treatments and prevention, it’s essential to build a solid foundation of what ringworm is, what causes it, and how it behaves.
This section demystifies the condition and answers the most fundamental questions.
What Exactly Is Ringworm? (And Why Isn’t It a Worm?)
At its core, ringworm is a superficial fungal infection.
It affects the top layers of your skin, hair, or nails.
The fungi responsible for this infection are a specialized group called dermatophytes.
These microscopic organisms thrive on keratin, the tough, waterproof protein that makes up our skin, hair, and nails.
The three main genera of dermatophytes that cause ringworm are Trichophyton, Microsporum, and Epidermophyton.
The term “ringworm”, is a classic misnomer, a relic from a time before the true cause was understood.
The name comes from two sources: the Latin word tinea, which means “gnawing worm”, and the distinct, circular or “ring-like” appearance of the rash.
Early observers mistakenly believed a worm was burrowing under the skin, creating the lesion.
We now know this is incorrect, but the common name has persisted for centuries.
Key Definition: Ringworm (tinea or dermatophytosis) is a contagious fungal infection of the skin, hair, or nails caused by dermatophyte fungi. It is characterized by an itchy, red, scaly patch that may be ring-shaped. Despite its name, no worm is involved.
What Does Ringworm Look Like? (Key Symptoms and Visual Clues)
While the “ring”, is its most famous feature, the appearance of a ringworm infection can vary depending on its location and severity.
However, there are several hallmark signs and symptoms to watch for.
The classic presentation, especially on the body (tinea corporis), is an annular (ring-shaped) lesion.
This rash typically starts as a small, red, scaly spot.
As it grows, the center of the lesion may begin to clear, leaving a ring with a raised, scaly, and actively spreading border.
This border is where the fungus is most active.
Common symptoms associated with a ringworm infection include:
- Intense itching (pruritus): This is often the most bothersome symptom.
- Red, scaly, or cracked skin: The texture of the affected skin changes noticeably.
- A circular or ring-shaped rash: The lesion typically expands outwards over days or weeks.
- Hair loss: In cases of scalp ringworm (tinea capitis) or beard ringworm (tinea barbae), the fungus can invade the hair follicles, causing hair to become brittle and break off, leading to bald patches.
- Nail changes: For fungal nail infections (tinea unguium), nails may become thick, brittle, crumbly, and discolored (often turning yellow or brownish).
It’s crucial to note that not all ringworm infections look like a perfect ring.
Sometimes, the lesions can be irregular in shape, multiple rings can merge, or they may appear as simple scaly patches without significant central clearing.
This variability is a common reason for misdiagnosis.
How Is Ringworm Transmitted? (Understanding How It Spreads)
Ringworm is highly contagious, and understanding its transmission routes is the first step toward prevention.
The dermatophyte fungi can spread through three primary pathways:
- Human-to-Human (Anthropophilic Transmission): This is the most common route, occurring through direct, skin-to-skin contact with an infected person. It’s frequently seen in environments with close physical contact, such as households, schools, and contact sports like wrestling. Sharing personal items also falls into this category.
- Animal-to-Human (Zoophilic Transmission): Many animals can carry dermatophytes and pass them to humans. Common culprits include kittens and puppies, but also guinea pigs, rabbits, and farm animals. According to a study in Mycoses, infections acquired from animals (e.g., caused by *Microsporum canis* from cats) can often cause a more intense inflammatory reaction in humans than those passed between people.
- Object-to-Human (Geophilic/Fomite Transmission): Fungal spores are hardy and can survive for long periods on surfaces and objects, known as fomites. You can contract ringworm by touching contaminated items. Common sources of transmission include:
- Towels, clothing, and bed linens
- Combs, hairbrushes, and hats
- Damp surfaces like locker room floors, public showers, and pool decks
- Shared sports equipment or gym mats
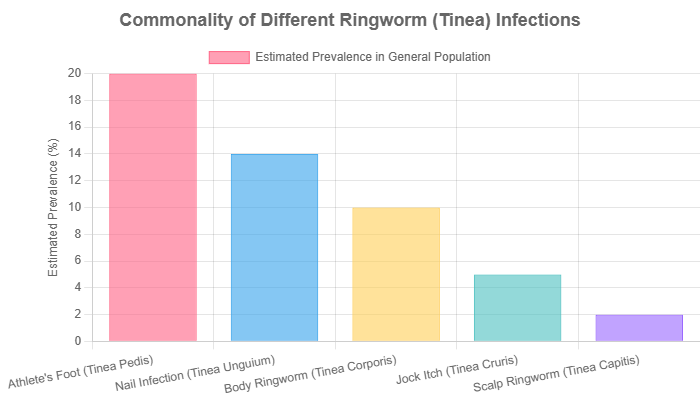
Part 2: The Many Faces of Tinea: Types of Ringworm by Body Location
One of the most important aspects of understanding ringworm is knowing that it’s not a single disease but a family of infections.
The medical name, tinea, is followed by a Latin term that specifies the affected body part.
While the underlying cause is the same group of fungi, the symptoms, appearance, and required treatment can differ significantly based on location.
Where Can You Get Ringworm? A Head-to-Toe Breakdown
Here is a detailed look at the most common types of tinea infections:
Tinea Corporis (Ringworm of the Body)
This is the “classic” ringworm that affects the smooth skin of the trunk, arms, and legs.
It presents with the typical ring-shaped, itchy, red rash with a clearing center.
It’s what most people picture when they hear the word “ringworm”.
Tinea Pedis (Athlete’s Foot)
As the name suggests, this is a ringworm infection of the feet.
It is extremely common, especially among people who wear tight-fitting shoes or frequent public showers and gyms.
Symptoms include itching, stinging, and burning between the toes or on the soles of the feet, along with peeling, cracking, and blistering skin.
Tinea Cruris (Jock Itch)
This infection affects the skin of the groin, inner thighs, and buttocks.
It is more common in men and adolescent boys.
Tinea cruris appears as a red-brown, itchy rash that often has a sharply defined, scaly border. It’s often associated with sweating and wearing tight clothing.
Tinea Capitis (Ringworm of the Scalp)
Primarily affecting children, tinea capitis is a serious infection that requires prompt medical attention.
It can cause itchy, scaly, gray or reddish patches on the scalp.
A key sign is hair loss, which can manifest as bald spots or “black dots” where the hair has broken off at the scalp’s surface.
This type of ringworm almost always requires treatment with oral antifungal medication.
Tinea Unguium (Onychomycosis or Fungal Nail Infection)
This is a fungal infection of the fingernails or, more commonly, the toenails. It affects an estimated 14% of the general population.
The infected nail can become thickened, brittle, crumbly, and distorted in shape.
It often turns a yellowish or brownish color.
Treatment can be long and challenging, often requiring months of oral medication.
Tinea Manuum (Ringworm of the Hands)
This infection affects one or both hands.
It often presents as dry, scaly skin on the palms.
A classic clinical pattern is the “one hand, two feet” syndrome, where a patient has tinea pedis on both feet and tinea manuum on only one hand (usually the dominant hand, from scratching the feet).
Tinea Barbae (Ringworm of the Beard)
This less common type affects the beard and mustache area of the face in adult men.
It can cause itchy, scaly, red patches and may lead to hair loss in the beard.
It can sometimes form deeper, pus-filled sores (kerion).
Informative Table: Comparing Types of Ringworm
| Medical Name | Common Name | Affected Area | Key Symptoms | Common Treatment Approach |
|---|---|---|---|---|
| Tinea Corporis | Body Ringworm | Trunk, arms, legs | Classic ring-shaped, itchy, red rash with central clearing. | Topical Antifungals |
| Tinea Pedis | Athlete’s Foot | Feet, especially between toes | Itching, burning, peeling, cracked skin. | Topical Antifungals |
| Tinea Cruris | Jock Itch | Groin, inner thighs, buttocks | Red-brown, itchy rash with a sharp, scaly border. | Topical Antifungals |
| Tinea Capitis | Scalp Ringworm | Scalp, hair shafts | Scaly patches, hair loss, “black dots”, inflammation. | Oral Antifungals (Required) |
| Tinea Unguium | Fungal Nail Infection | Fingernails and toenails | Thick, brittle, discolored (yellow/brown) nails. | Oral Antifungals (Often Required) |
| Tinea Manuum | Hand Ringworm | Palms, back of hands | Dryness, scaling, peeling, often on one hand only. | Topical or Oral Antifungals |
| Tinea Barbae | Beard Ringworm | Beard and mustache area | Red, scaly patches, pustules, hair loss. | Oral Antifungals (Often Required) |
Part 3: Diagnosis, Misdiagnosis, and When to Seek Medical Help
Getting the right diagnosis is the most critical step toward effective treatment.
Many people attempt to self-treat skin rashes, but what works for eczema or psoriasis can make a fungal infection worse.
This section covers how doctors confirm a ringworm diagnosis and when it’s time to stop guessing and see a professional.
How Is Ringworm Officially Diagnosed by a Doctor?
While an experienced dermatologist can often suspect ringworm based on a visual inspection, confirming the diagnosis with testing is best practice to ensure correct treatment.
The American Academy of Dermatology (AAD) outlines several methods:
- Clinical Examination: The process begins with a healthcare provider examining the rash and asking about your symptoms, potential exposures, and medical history.
- KOH Prep (Potassium Hydroxide Smear): This is the gold standard for rapid, in-office diagnosis. The doctor will gently scrape a small sample of scale from the active border of the rash. The sample is placed on a microscope slide with a drop of potassium hydroxide (KOH) solution, which dissolves skin cells but leaves the tough fungal elements intact. Viewing this under a microscope can reveal the characteristic branching, rod-shaped filaments (hyphae) of the fungus.
- Fungal Culture: If the KOH prep is inconclusive or if the infection is not responding to treatment, a sample of skin, hair, or nail can be sent to a laboratory. There, it is placed on a special medium (like Sabouraud dextrose agar) to see if fungus grows. This test is more definitive and can identify the exact species of dermatophyte, but results can take several weeks.
- Wood’s Lamp Examination: A Wood’s lamp emits ultraviolet (UV) light. Certain species of dermatophytes, particularly from the *Microsporum* genus, will fluoresce a bright yellow-green color under this light. It’s a quick, painless test but is only useful for specific types of scalp ringworm.
Ringworm vs. Other Skin Rashes: How to Tell the Difference?
One of the biggest challenges with ringworm is that it can look like several other common skin conditions.
Using the wrong treatment, especially a steroid cream, can suppress the inflammation and make the rash look better temporarily, but it allows the fungus to spread unchecked—a condition known as tinea incognito.
Expert Warning: Never apply a potent steroid cream (like hydrocortisone) to a rash unless you are certain it is not a fungal infection. Steroids weaken the skin’s local immune response, which can cause the ringworm to worsen and spread.
Here’s how ringworm compares to common look-alikes:
- vs. Nummular Eczema: This condition also causes coin-shaped or round patches of irritated skin. However, nummular eczema typically lacks the central clearing seen in classic ringworm. The entire patch is usually uniformly red and scaly or weepy.
- vs. Psoriasis: Psoriasis can cause red, raised plaques with scaling. The key difference is the scale: psoriatic scales are typically much thicker, silvery-white, and more well-demarcated than the fine scale of ringworm.
- vs. Pityriasis Rosea: This viral rash often starts with a single, large oval patch called a “herald patch”, which can be mistaken for ringworm. However, this is usually followed by a widespread eruption of smaller, oval-shaped pink patches, often in a “Christmas tree” pattern on the back.
- vs. Granuloma Annulare: This condition also forms ring-shaped lesions, but they are typically smooth, skin-colored or reddish bumps and lack the scaling characteristic of ringworm.
When Should You See a Doctor for a Ringworm Infection?
While simple cases of body ringworm can often be managed with over-the-counter products, it’s crucial to seek professional medical advice in certain situations. You should see a doctor if:
- The infection is on the scalp or in the beard. Tinea capitis and tinea barbae require oral prescription medications to penetrate the hair follicle and eradicate the infection. Topical creams are not sufficient.
- Over-the-counter (OTC) treatments have not improved the rash after two weeks of consistent use. This could indicate a more resistant fungus or an incorrect diagnosis.
- The rash is widespread, covering a large area of your body, or spreading rapidly.
- You have a weakened immune system. Individuals with conditions like diabetes, HIV/AIDS, or those undergoing chemotherapy are more susceptible to severe or widespread infections and require medical supervision.
- The area shows signs of a secondary bacterial infection. Look for increased pain, swelling, warmth, the formation of pus, or a fever.
- You are simply unsure of the diagnosis. Getting a definitive diagnosis from a healthcare provider is the fastest way to get the right treatment and avoid making the problem worse.
Part 4: The Definitive Guide to Treating Ringworm
Treating ringworm effectively requires the right medication, proper application, and—most importantly—patience and adherence.
This section breaks down the evidence-based treatment options, from store-bought creams to prescription pills, and addresses the growing concern of drug resistance.
How Do You Treat Ringworm Effectively? (Medical Treatments)
Treatment for ringworm is based on the location and severity of the infection.
The goal is to kill the fungus and prevent it from spreading.
Over-the-Counter (OTC) Antifungal Options
For uncomplicated cases of ringworm on the body (tinea corporis), athlete’s foot (tinea pedis), and jock itch (tinea cruris), OTC topical antifungals are the first line of defense.
These come as creams, lotions, powders, or sprays. Look for products containing these active ingredients:
- Clotrimazole (e.g., Lotrimin AF)
- Miconazole (e.g., Micatin)
- Terbinafine (e.g., Lamisil AT)
- Tolnaftate (e.g., Tinactin)
Expert Application Tip: When applying a topical antifungal, don’t just cover the rash.
Apply the cream to the visible lesion and also to a border of about two inches of normal-looking skin around it.
This targets the fungus that may be spreading invisibly.
Crucially, continue using the treatment for at least one to two weeks after the rash has completely disappeared to kill any lingering spores and prevent recurrence.
Prescription-Strength Medications
If OTC treatments fail or if the infection is severe or located in a hard-to-treat area, a doctor will prescribe stronger medications.
- Prescription Topicals: These include stronger versions of OTC drugs or different agents like Ketoconazole, Econazole, or Ciclopirox. They are more potent and may be needed for more stubborn skin infections.
- Oral Antifungals: These pills are essential for treating ringworm of the scalp (tinea capitis) and nails (tinea unguium), as topical creams cannot effectively penetrate these areas. They are also used for widespread or inflammatory skin infections. Common oral antifungals include:
- Terbinafine: Often a first-choice for many dermatophyte infections due to its high efficacy.
- Itraconazole: Another powerful broad-spectrum antifungal.
- Griseofulvin: A classic treatment, especially for scalp ringworm in children.
- Fluconazole: Used for certain types of fungal infections.
Treatment with oral medications can last from a few weeks for skin infections to several months for nail infections.
It is vital to complete the entire prescribed course.
The Critical Importance of Treatment Adherence
One of the most common reasons for treatment failure and recurrence is stopping the medication too soon.
The rash may look better and stop itching long before the fungus is completely eradicated.
Stopping treatment early allows the surviving fungi to regrow, often leading to a relapse that can be harder to treat the second time around.
This is a major theme in user forums like Reddit, where people express frustration over “ringworm that won’t go away”.
What About Drug-Resistant Ringworm? (An Emerging Global Concern)
This is a topic of growing importance that sets this guide apart from more basic resources.
In recent years, health authorities have noted the emergence of antifungal-resistant strains of ringworm.
The CDC has issued alerts about strains like Trichophyton indotineae, which often show resistance to terbinafine, a standard first-line treatment.
This emerging threat has significant implications:
- Treatment Failure: Standard therapies may not work, leading to chronic, widespread, and highly inflammatory infections.
- Need for Specialized Care: Diagnosis may require fungal culture with susceptibility testing to determine which drugs will be effective.
- Alternative Treatments: Patients may need longer courses of different, and often more expensive, antifungal drugs like itraconazole. Research published in journals like the Journal of Fungi highlights the urgent need for better diagnostics and new treatment strategies.
If your ringworm is not responding to standard treatment, it is essential to see a dermatologist who is aware of these emerging resistant strains.
Are There Any Home Remedies for Ringworm That Actually Work?
A quick search online reveals dozens of supposed home remedies for ringworm, from tea tree oil to apple cider vinegar.
It’s important to approach these with a scientific and cautious perspective.
- Tea Tree Oil: Some laboratory studies suggest tea tree oil has antifungal properties. However, clinical evidence in humans is limited, and it can cause significant skin irritation or allergic reactions in some people.
- Apple Cider Vinegar: Proponents claim its acidity creates an inhospitable environment for fungus. There is no strong scientific evidence to support its use for ringworm, and applying it directly to skin can cause chemical burns.
- Coconut Oil: Contains fatty acids that have shown some mild antifungal activity in lab settings, but it’s unlikely to be potent enough to cure an established infection.
The Verdict: While some natural substances may have mild antifungal effects, they are not a reliable or proven substitute for medical treatment.
They have not undergone the rigorous testing for safety and efficacy that FDA-approved antifungal medications have.
At best, they might be used as a complementary measure *after* consulting a doctor, but they should never be the primary treatment for a confirmed ringworm infection.
Part 5: Prevention: Your Best Defense Against Ringworm
Given how easily ringworm spreads, prevention is just as important as treatment.
Following good hygiene and environmental practices can significantly reduce your risk of contracting an infection or spreading it to others.
How Can You Prevent Ringworm from Spreading or Recurring?
A multi-pronged approach focusing on personal hygiene, environmental control, and managing active infections is most effective.
Personal Hygiene Best Practices
- Keep Your Skin Clean and Dry: Fungus thrives in warm, moist environments. Dry your skin thoroughly after bathing, paying special attention to skin folds, the groin area, and between your toes.
- Change Socks and Underwear Daily: Or more often if you sweat heavily.
- Do Not Share Personal Items: This is one of the most critical rules. Avoid sharing towels, clothing, combs, hairbrushes, hats, or any other item that comes into direct contact with skin or hair.
- Wash Hands Thoroughly: Wash your hands with soap and water after touching an infected area on your own body, after applying medication, or after touching a pet that may be infected.
Managing Your Environment
- Wear Protective Footwear: Always wear sandals, flip-flops, or shower shoes in public locker rooms, gym showers, and around swimming pools.
- Wash Contaminated Items: Wash any bedding, towels, and clothing used by an infected person in hot water with detergent.
- Disinfect Surfaces: Clean and disinfect surfaces that may have come into contact with the fungus, such as gym equipment, bathroom floors, and counters.
- Choose Breathable Fabrics: Wear loose-fitting clothing made of cotton or other breathable materials to reduce moisture buildup.
What to Do If a Pet or Family Member Is Infected
- Treat Everyone at Once: If one person in a household has ringworm, it’s possible others do too, even without symptoms yet. For scalp ringworm, all household members may be advised to use an antifungal shampoo to prevent a cycle of reinfection.
- Get Pets Checked by a Vet: If you suspect your pet is the source (common signs include patches of missing fur), take them to a veterinarian for diagnosis and treatment. While treating your pet, limit contact and vacuum frequently to remove contaminated hair and skin cells from the environment.
Part 6: Frequently Asked Questions (FAQ)
Here are quick, direct answers to some of the most common questions about ringworm.
1. How long is ringworm contagious?
Ringworm is contagious as long as live fungus is present on the skin. You are generally considered contagious until you have been using an effective antifungal treatment for at least 24-48 hours. However, it’s best to take precautions until the rash is gone.
2. Can you get ringworm even if you are very clean?
Yes. Ringworm is caused by exposure to a fungus, not by poor hygiene. While keeping skin clean and dry helps prevent it, anyone can get ringworm through contact with an infected person, animal, or surface, regardless of their personal cleanliness.
3. Does ringworm leave scars?
Typically, superficial ringworm infections do not leave scars if treated properly. However, severe, deep, or inflammatory infections (like a kerion on the scalp) or those with a secondary bacterial infection can potentially lead to scarring or permanent hair loss.
4. Can stress cause a ringworm outbreak?
Stress does not directly cause ringworm, as the infection requires exposure to the fungus. However, severe stress can weaken the immune system, potentially making you more susceptible to contracting an infection if you are exposed, or making an existing infection harder to fight off.
5. What is the fastest way to get rid of ringworm?
The fastest and most effective way is to get an accurate diagnosis from a doctor and use the prescribed or recommended antifungal medication consistently for the full duration. There are no safe “overnight” cures, proper medical treatment is key.
6. Can I go to work/school with ringworm?
Generally, yes, provided the infected area can be covered with clothing or a bandage. Most schools and workplaces allow attendance once treatment has begun. For contact sports, athletes should be withheld from competition until cleared by a healthcare provider.
7. Does bleach kill ringworm on the skin?
Absolutely not. You should never apply bleach or other harsh household disinfectants to your skin. This is dangerous and can cause severe chemical burns and skin damage, making the situation much worse. Use only medically approved antifungal treatments.
8. Why does my ringworm keep coming back?
Recurrence is often due to stopping treatment too early, reinfection from a contaminated environment (bedding, towels) or an untreated family member/pet, or potentially a drug-resistant strain. Ensure you complete the full treatment course and decontaminate your environment.
Conclusion
Ringworm, or tinea, is a widespread and treatable fungal infection, but its misleading name and resemblance to other rashes can cause confusion and treatment delays.
The most critical takeaways from this guide are that correct diagnosis is paramount, different types of ringworm require different treatment approaches, and strict adherence to the full course of medication is essential for a complete cure.
While common, ringworm should be taken seriously to prevent its spread, avoid uncomfortable symptoms, and mitigate the risk of complications or chronic infection, especially in light of emerging drug-resistant strains.
By understanding how it spreads and practicing good preventive hygiene, you can significantly reduce your risk.
If you are struggling with a persistent rash, an infection on your scalp or nails, or are simply unsure what you’re dealing with, do not hesitate to consult a dermatologist or another qualified healthcare provider.
Professional medical advice is your best tool for achieving an accurate diagnosis and a personalized treatment plan that will resolve the infection effectively and safely.
References
- U.S. Centers for Disease Control and Prevention (CDC). (2024). Clinical Overview of Ringworm and Fungal Nail Infections. https://www.cdc.gov/ringworm/hcp/clinical-overview/index.html
- American Academy of Dermatology (AAD). (n.d.). Ringworm: Diagnosis and treatment. https://www.aad.org/public/diseases/a-z/ringworm-treatment
- Yee, G., & Al Aboud, A. M. (2025). Tinea Corporis. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK544360/
- Mayo Clinic. (n.d.). Ringworm (body) – Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/ringworm-body/symptoms-causes/syc-20353780
- U.S. Centers for Disease Control and Prevention (CDC). (2024). Antifungal-resistant Ringworm. https://www.cdc.gov/fungal/diseases/ringworm/antifungal-resistant.html
- Leung, A. K., Lam, J. M., Leong, K. F., & Hon, K. L. (2020). Tinea corporis: an updated review. Mycoses, 63(7), 697–706. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7375854/
- Gupta, A. K., & Cooper, E. A. (2024). Current and emerging issues in dermatophyte infections. Journal of Fungi, 10(6), 465. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11175395/

