Pelvic inflammatory disease (PID) is a serious infection of the female upper reproductive organs, including the uterus, fallopian tubes and ovaries.
It most often develops when sexually transmitted bacteria spread from the vagina upwards.
Affecting an estimated 2.5 million women aged 18-44 in the United States, PID can cause severe long-term consequences like infertility and chronic pain, yet its symptoms are often subtle or even absent, leading to delayed diagnosis and treatment.
This comprehensive guide will explore every facet of pelvic inflammatory disease, from its hidden symptoms and diverse causes—including both STI and non-STI related factors—to the latest diagnostic methods, advanced treatment options and crucial prevention strategies.
Understanding this condition is the first step toward protecting your reproductive health for years to come.
In This Article
What is Pelvic Inflammatory Disease (PID)?
A Simple Definition
Pelvic inflammatory disease, commonly known as PID, is not a single disease but rather a spectrum of inflammatory disorders affecting the upper female genital tract.
As defined by the Centers for Disease Control and Prevention (CDC), it represents an infection that has ascended from the lower genital tract (vagina and cervix) into the typically sterile environment of the upper reproductive organs.
Which Organs Are Affected?
PID can involve any combination of the following organs, leading to specific conditions:
- Uterus: Inflammation of the uterine lining is called endometritis.
- Fallopian Tubes: Inflammation of the fallopian tubes is called salpingitis. This is a hallmark of PID and a primary cause of its long-term complications.
- Ovaries: Inflammation of the ovaries is called oophoritis.
- Pelvic Peritoneum: The infection can also spread to the membrane lining the inside of the abdomen and pelvis, causing pelvic peritonitis.
In severe cases, the infection can lead to the formation of a tubo-ovarian abscess (TOA), which is a pocket of pus involving the fallopian tube and ovary.
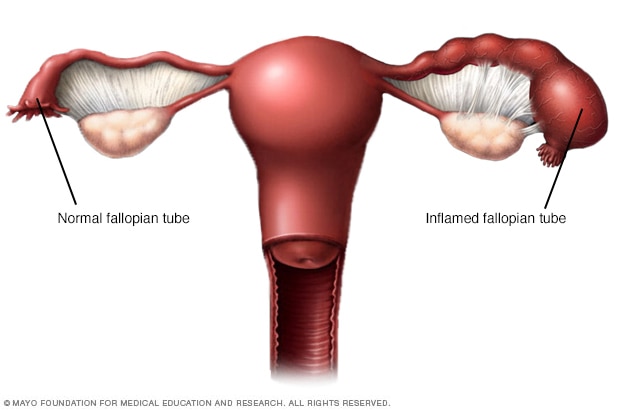
Pelvic inflammatory disease (PID) is an infection of the upper reproductive organs. Untreated, it can cause permanent damage.
How Does the Infection Spread?
The development of pelvic inflammatory disease is typically an ascending process.
The cervix normally acts as a barrier, preventing bacteria from the vagina from entering the upper genital tract.
However, certain infections, particularly STIs like chlamydia and gonorrhea, can disrupt this barrier.
This disruption, known as cervicitis, allows pathogenic microorganisms to travel upward.
This ascent is not random. Factors like menstruation (when the cervical mucus is thinner) and uterine contractions can facilitate the upward movement of bacteria.
Once in the uterus, the infection can spread through the fallopian tubes and to the ovaries and surrounding pelvic structures, causing widespread inflammation and damage.
The Alarming Statistics: How Common is PID?
While rates have been decreasing over the past decade, largely due to improved screening for STIs, PID remains a significant public health concern.
- According to the CDC, a 2013–2014 national survey found that 4.4% of sexually experienced women of reproductive age in the U.S. reported a lifetime diagnosis of PID. This equates to an estimated 2.5 million women with a history of the condition.
- Older data from the American College of Obstetricians and Gynecologists (ACOG) notes that PID is diagnosed in more than 1 million women in the United States each year.
- The condition is most common in sexually active women aged 15 to 25.
The true prevalence may be even higher, as many cases of PID are “silent” or subclinical, meaning they produce mild or no symptoms and go undiagnosed.
What Are the Symptoms of Pelvic Inflammatory Disease?
One of the greatest challenges in diagnosing and treating pelvic inflammatory disease is the wide variation in its presentation.
Symptoms can range from severe and debilitating to mild and easily dismissed, or they can be completely absent.
The Challenge of “Silent” or Mild PID
Many women with PID do not experience any noticeable signs or symptoms.
This is often referred to as subclinical PID.
This is particularly common with chlamydia-associated PID, which tends to be less symptomatic than PID caused by gonorrhea.
The danger of silent PID is that the infection can cause significant, permanent damage to the reproductive organs without the person ever knowing they are infected until they experience long-term complications, such as infertility or chronic pelvic pain.
Common and Recognizable PID Symptoms
When symptoms of pelvic inflammatory disease are present, they can be vague and mistaken for other conditions like menstrual cramps or a urinary tract infection.
According to sources like the Mayo Clinic and ACOG, the most common signs include:
- Pain in the lower abdomen and pelvis: This is the most frequent symptom. The pain can range from a mild, dull ache to severe, cramping pain. It is often bilateral (on both sides).
- Unusual or heavy vaginal discharge: The discharge may have an unpleasant or foul odor and can be yellow or green in color.
- Abnormal uterine bleeding: This can include bleeding between periods, bleeding after intercourse, or heavier-than-usual periods.
- Pain during sexual intercourse (Dyspareunia): This deep pelvic pain during or after sex is a common red flag.
- Fever and chills: A fever, sometimes low-grade, may be present, especially in more severe cases.
- Painful, frequent or difficult urination: These symptoms can mimic a bladder infection.
Less Common but Serious Symptoms
In some cases, the inflammation from PID can spread beyond the pelvic organs.
A notable example is Fitz-Hugh-Curtis syndrome, where the infection spreads to the tissue surrounding the liver.
This can cause sharp pain in the upper right abdomen, which may be mistaken for gallbladder or liver problems.
The pain can sometimes radiate to the right shoulder.
When Should You See a Doctor for PID Symptoms?
Given the potential for severe complications, it is crucial to seek medical attention if you suspect you have pelvic inflammatory disease.
Do not dismiss your symptoms, even if they are mild.
Urgent Medical Care: When to Go to the ER
Seek emergency medical care immediately if you experience any of the following severe symptoms, as they could indicate a serious infection or another medical emergency like an ectopic pregnancy or appendicitis:
- Severe pain low in your abdomen that makes it difficult to stand or walk.
- Nausea and vomiting, with an inability to keep food or fluids down.
- A high fever, typically over 101°F (38.3°C).
- Foul-smelling, copious vaginal discharge.
Scheduling a Doctor’s Visit for Milder Symptoms
Even if your symptoms are not severe, you should see your healthcare provider as soon as possible.
Symptoms like unusual discharge, painful urination, or bleeding between periods are not normal and warrant investigation.
These can be signs of an STI that, if treated promptly, can prevent the development of full-blown PID.
Expert Tip: When you see your provider, be prepared to discuss your symptoms, sexual history, and contraceptive methods openly. This information is vital for an accurate diagnosis.
The Importance of Not Delaying Treatment
Delaying treatment for pelvic inflammatory disease dramatically increases the risk of long-term complications.
Research published in the American Journal of Obstetrics and Gynecology found that women who delayed seeking care for PID were significantly more likely to experience infertility or ectopic pregnancy.
Prompt evaluation and treatment are your best defense against permanent damage.
What Causes Pelvic Inflammatory Disease?
While PID is a polymicrobial infection (meaning multiple types of bacteria can be involved), the initial trigger is often an infection that begins in the cervix.
These infections can be broadly categorized into sexually transmitted and non-sexually transmitted causes.
The Primary Culprits: Sexually Transmitted Infections (STIs)
The vast majority of PID cases are linked to untreated STIs.
These bacteria are highly effective at infecting the cervix and disrupting its natural defenses.
- Neisseria gonorrhoeae (Gonorrhea): Historically a major cause of PID, gonorrhea tends to produce more severe, acute symptoms. According to StatPearls, gonorrheal PID is often more clinically severe than PID from other pathogens.
- Chlamydia trachomatis (Chlamydia): Chlamydia is now the most common bacterial STI and a leading cause of PID. It is notoriously “silent”, often causing few or no initial symptoms, which allows it to progress to PID undetected. It’s estimated that 10% to 15% of women with untreated chlamydia will develop PID.
The Emerging Pathogen: Mycoplasma genitalium
In recent years, another STI, Mycoplasma genitalium (Mgen), has been increasingly recognized as a significant cause of PID.
A systematic review and meta-analysis confirmed that Mgen infection is associated with a 67% increased odds of PID and is found in about 1 in 10 PID cases.
Like chlamydia, Mgen often causes mild or asymptomatic infections, contributing to its spread and progression to upper genital tract disease.
A major concern with Mgen is its growing resistance to common antibiotics, making treatment more complex.
Beyond STIs: Other Causes of PID
While STIs are the main drivers, it’s a critical misconception that PID is exclusively an STI.
Research indicates that a significant portion of cases are not related to gonorrhea or chlamydia.
- Bacterial Vaginosis (BV): BV is a condition caused by an imbalance in the normal vaginal flora, leading to an overgrowth of anaerobic bacteria. While not an STI, having BV is strongly associated with an increased risk of developing PID. These BV-associated bacteria can ascend into the upper genital tract, either on their own or alongside an STI and contribute to the inflammatory process.
- Post-procedural Infections: Any procedure that disturbs the cervical barrier can introduce bacteria into the uterus. This can happen, though less commonly, after:
- Childbirth
- Miscarriage or therapeutic abortion
- Insertion of an intrauterine device (IUD)
- Other gynecologic procedures involving instrumentation of the uterus
- Other Bacteria: In some cases, respiratory or enteric (gut) bacteria like Haemophilus influenzae and Escherichia coli have been implicated in PID, though this is rare.
Who is Most at Risk for Developing PID?
Several factors can increase a woman’s risk of developing pelvic inflammatory disease.
These risks are closely tied to the risk of acquiring an STI.
Key Demographic and Behavioral Risk Factors
The following factors are consistently associated with a higher risk of PID:
- Age: Being sexually active and younger than 25 is a primary risk factor. The cervix of an adolescent or young woman is not fully matured, making it more susceptible to infections like chlamydia.
- Multiple Sexual Partners: Having more than one sexual partner, or having a partner who has other partners, significantly increases the likelihood of exposure to STIs.
- Inconsistent Condom Use: Having sex without a condom is a major risk factor. Condoms are highly effective at preventing the transmission of bacteria that cause PID.
- A History of PID or STIs: A previous episode of PID damages the reproductive tract and makes it more vulnerable to future infections. A history of any STI also indicates a higher risk.
The Douching Debate: Why It Increases Risk
Douching is the practice of washing or cleaning out the inside of the vagina with water or other fluids.
Health organizations like ACOG strongly advise against it.
Douching upsets the natural balance of bacteria in the vagina, which can:
- Allow harmful bacteria to overgrow.
- Physically push infection-causing bacteria from the vagina and cervix up into the uterus and fallopian tubes.
- Mask symptoms like unusual discharge, causing a delay in seeking medical care.
Intrauterine Devices (IUDs): Clarifying the Risk
There is a small, temporary increased risk of PID associated with IUD insertion.
However, this risk is primarily confined to the first three weeks after the device is inserted.
The risk is thought to be related to the introduction of bacteria into the uterus during the insertion procedure itself.
Beyond this initial period, IUDs do not increase the risk of PID.
In fact, hormonal IUDs may even offer some protection by thickening cervical mucus, making it harder for bacteria to ascend.
How is Pelvic Inflammatory Disease Diagnosed?
Diagnosing PID can be difficult because its symptoms are often nonspecific and can overlap with many other conditions.
There is no single, simple test to definitively diagnose PID.
Therefore, diagnosis is primarily clinical, based on a combination of your symptoms, a physical exam and supporting lab tests.
The Challenge of a Clinical Diagnosis
Because of the potential for serious complications, healthcare providers are encouraged to maintain a low threshold for diagnosing and treating PID.
This means they may start presumptive treatment based on clinical suspicion even before all test results are back.
The CDC notes that a clinical diagnosis of PID has a positive predictive value of 65%–90% compared to laparoscopy, meaning it’s correct most, but not all, of the time.
The Diagnostic Process: What to Expect at Your Appointment
If your provider suspects PID, the evaluation will typically include:
- Medical and Sexual History: Your provider will ask about your symptoms, sexual habits, number of partners, contraceptive use and any history of STIs.
- Pelvic Exam: This is a crucial part of the evaluation. Your provider will perform a bimanual exam to check for the hallmark signs of PID:
- Cervical motion tenderness: Pain when the cervix is moved.
- Uterine tenderness: Pain when the uterus is palpated.
- Adnexal tenderness: Pain or tenderness in the area of the fallopian tubes and ovaries.
- Lab Tests: Samples will be taken to look for signs of infection.
- Cervical Swabs: Samples from your cervix and vagina will be sent for Nucleic Acid Amplification Testing (NAAT) to detect Chlamydia trachomatis, Neisseria gonorrhoeae, and, if available, Mycoplasma genitalium.
- Microscopy: A sample of vaginal fluid (a “wet prep”) may be examined under a microscope for an abundance of white blood cells, which indicates inflammation, and to check for co-infections like bacterial vaginosis or trichomoniasis.
- Blood and Urine Tests: These can be used to check for pregnancy (to rule out ectopic pregnancy), test for other STIs like HIV and syphilis and measure inflammatory markers or white blood cell counts.
Advanced Diagnostic Tools
If the diagnosis is uncertain, or if you are severely ill, your provider may order more specific tests:
- Transvaginal Ultrasound: This imaging test uses sound waves to create pictures of your reproductive organs. While a normal ultrasound does not rule out PID, it can help identify complications. According to AAFP, findings suggestive of PID include thickened, fluid-filled fallopian tubes (hydrosalpinx) or a tubo-ovarian abscess.
- Endometrial Biopsy: A small sample of the uterine lining is removed and examined for signs of inflammation (endometritis). This is more invasive and not routinely done.
- Laparoscopy: This is a surgical procedure where a thin, lighted scope is inserted through a small incision in the abdomen to directly view the pelvic organs. It is considered the “gold standard” for diagnosing PID, as it allows the surgeon to see inflammation or scarring on the fallopian tubes. However, due to its cost and invasive nature, it is reserved for cases where the diagnosis is unclear or when other surgical emergencies cannot be ruled out.
What Are the Treatment Options for Pelvic Inflammatory Disease?
Prompt treatment for pelvic inflammatory disease is essential to eradicate the infection and, most importantly, to prevent or minimize long-term damage to the reproductive organs.
Treatment cannot reverse any scarring that has already occurred, which is why early intervention is so critical.
First-Line Treatment: Antibiotic Regimens
PID is treated with a combination of broad-spectrum antibiotics to cover all likely pathogens, including gonorrhea, chlamydia, and anaerobic bacteria often associated with BV.
Treatment should be started as soon as PID is suspected, without waiting for lab results.
The CDC provides specific guidelines for treatment, which may involve oral pills, intramuscular (IM) injections, or intravenous (IV) therapy.
It is absolutely crucial to take all of your medication as prescribed, even if you start to feel better.
Stopping treatment early can lead to treatment failure and an increased risk of complications.
| Setting | Primary Regimen | Notes |
|---|---|---|
| Outpatient (Mild-to-Moderate PID) | Ceftriaxone 500 mg IM in a single dosePLUS Doxycycline 100 mg orally twice a day for 14 daysWITH Metronidazole 500 mg orally twice a day for 14 days | This combination provides broad coverage for gonorrhea, chlamydia, and anaerobes. Metronidazole is now routinely recommended to improve outcomes. |
| Inpatient (Hospitalization) | One of the following:Ceftriaxone 1 g IV every 24 hours + Doxycycline 100 mg orally/IV every 12 hours + Metronidazole 500 mg orally/IV every 12 hoursCefotetan 2 g IV every 12 hours + Doxycycline 100 mg orally/IV every 12 hours | IV therapy is used for more severe cases. Patients can often transition to oral antibiotics after 24-48 hours of clinical improvement to complete a 14-day course. |
When is Hospitalization Necessary?
While many cases of PID can be treated on an outpatient basis, your provider may recommend a hospital stay if you:
- Are severely ill (e.g., high fever, nausea, vomiting).
- Are pregnant.
- Have a tubo-ovarian abscess (TOA).
- Cannot tolerate oral medications.
- Have not responded to outpatient treatment within 72 hours.
- Have a diagnosis that is uncertain, and surgical emergencies like appendicitis cannot be ruled out.
Treating Your Partner(s): A Critical Step for Prevention
This is a non-negotiable part of PID treatment.
Any person you have had sexual contact with in the 60 days preceding your symptoms must be evaluated and treated for STIs, regardless of whether they have symptoms.
If they are not treated, you are at high risk of being reinfected.
You should abstain from sexual intercourse until you and your partner(s) have completed the full course of treatment and your symptoms have resolved.
What Happens if Antibiotics Fail?
Treatment failure can occur, especially with the rise of antibiotic-resistant bacteria like M. genitalium. If your symptoms do not improve within 3 days of starting treatment, you must contact your healthcare provider.
This may require a change in antibiotics, further diagnostic testing or hospitalization for IV therapy.
For complications like a large or persistent tubo-ovarian abscess, drainage via a needle (guided by ultrasound or CT) or surgical intervention may be necessary.
What Are the Long-Term Complications of Untreated or Repeated PID?
The inflammation from pelvic inflammatory disease can cause scar tissue (adhesions) to form in the delicate structures of the upper genital tract.
This permanent damage is the root cause of PID’s most devastating long-term complications.
Infertility: The Risk of Tubal Scarring
PID is a leading cause of preventable infertility in women.
The infection can scar the inside of the fallopian tubes, creating blockages that prevent the egg from meeting the sperm or from traveling to the uterus.
- ACOG estimates that 1 in 10 women with PID will become infertile.
- The risk of infertility increases with each subsequent episode of PID. After one episode, the risk is around 10-15% after three or more episodes, the risk can jump to 50-75%.
- Delaying treatment also dramatically increases the risk of infertility.
Ectopic Pregnancy: A Life-Threatening Risk
Even if the fallopian tubes are only partially blocked or damaged by scarring, it can be enough to trap a fertilized egg.
Instead of implanting in the uterus, the egg implants and begins to grow inside the fallopian tube.
This is called a tubal or ectopic pregnancy.
An ectopic pregnancy is a medical emergency. As the embryo grows, it can cause the fallopian tube to rupture, leading to massive, life-threatening internal bleeding. The risk of ectopic pregnancy is increased 6 to 7 times in women who have had PID.
Chronic Pelvic Pain: A Debilitating Aftermath
For about 20% of women who have had PID, the pain doesn’t go away with treatment.
The adhesions and scar tissue can bind pelvic organs together, causing persistent pain that can last for months or years.
This chronic pelvic pain can be constant or may be triggered by activities like ovulation, menstruation or sexual intercourse.
Living with chronic pain can also have a significant psychological toll, leading to higher rates of depression and anxiety.
Tubo-Ovarian Abscess (TOA): A Serious Infection Pocket
In severe cases of PID, a collection of pus called an abscess can form in the fallopian tube and ovary.
A TOA is a serious complication that often requires hospitalization for aggressive IV antibiotic therapy. If the abscess is large or does not respond to antibiotics, it may need to be drained.
If a TOA ruptures, it can cause a life-threatening, body-wide infection (sepsis).
How Can You Prevent Pelvic Inflammatory Disease?
Since the most serious consequences of PID are often irreversible, prevention is paramount.
The strategies for preventing PID are centered on preventing STIs.
Practicing Safe Sex
- Use Condoms: Using male latex or polyurethane condoms correctly and consistently every time you have sex is one of the most effective ways to prevent the transmission of STIs that cause PID.
- Limit Your Number of Partners: Reducing your number of sexual partners decreases your potential exposure to STIs.
- Talk to Your Partner(s): Have open conversations about sexual history before beginning a new sexual relationship. Consider getting tested together.
The Role of Contraception
It’s important to understand that most forms of contraception, including birth control pills, patches, rings and hormonal IUDs, do not protect against STIs.
While they are effective for preventing pregnancy, you must still use a barrier method like a condom to protect against infection, especially with a new partner.
Regular STI Screening: The Best Defense
Since many STIs are asymptomatic, regular screening is the only way to know for sure if you are infected.
The CDC recommends annual screening for chlamydia and gonorrhea for:
- All sexually active women younger than 25.
- Older women with new or multiple sex partners, or a partner who has an STI.
Early detection and treatment of an STI is the single best way to prevent it from progressing to pelvic inflammatory disease.
Avoiding Douching
As mentioned earlier, do not douche. The vagina is self-cleaning, and douching disrupts its healthy ecosystem, increasing your risk of both vaginal infections and PID.
Frequently Asked Questions (FAQ) about PID
Can you get PID without having an STI?
Yes. While most cases are caused by STIs, PID can also result from an overgrowth of normal vaginal bacteria (like in bacterial vaginosis) or after medical procedures, childbirth, or miscarriage. These non-STI causes account for about 15% of cases.
Can PID go away on its own?
No. Pelvic inflammatory disease is a serious infection that requires antibiotic treatment. Without treatment, the infection can cause permanent damage to your reproductive organs, even if the initial symptoms seem to fade over time.
How long does it take to develop PID after an infection?
It can vary from a few days to a few weeks. After being infected with chlamydia or gonorrhea, if left untreated, the bacteria can ascend to the upper genital tract and cause PID within a relatively short timeframe.
Can men get PID?
No, PID is an infection of the female reproductive organs. However, men can carry and transmit the bacteria that cause PID (like chlamydia and gonorrhea) to their female partners, often without having any symptoms themselves.
Does PID always cause infertility?
Not always, but it is a major risk. About 1 in 10 women with PID become infertile. The risk increases significantly with repeated infections or delayed treatment. Prompt and complete antibiotic therapy is the best way to preserve fertility.
Can I get pregnant after having PID?
Yes, many women can still get pregnant after having PID, especially if it was a single episode that was treated quickly and effectively. However, your risk of infertility and ectopic pregnancy is higher than someone who has never had PID.
Will my partner know I have PID?
Your partner will not automatically know. You must inform any recent sexual partners (within the last 60 days) so they can be tested and treated. This is crucial to prevent them from developing complications and to prevent you from being reinfected.
Is PID contagious?
PID itself is not contagious. However, the underlying bacterial infections that cause it, such as chlamydia and gonorrhea, are highly contagious and are spread through sexual contact. This is why partner treatment is essential.
Conclusion
Pelvic inflammatory disease is a complex and serious condition with the potential for life-altering consequences.
It is far more than just a simple infection, it is an inflammatory cascade that can lead to infertility, ectopic pregnancy and chronic pain.
The key takeaways are clear: PID is often caused by untreated STIs, its symptoms can be deceptively mild or absent and the damage it causes can be permanent.
However, knowledge is power. By understanding the risks, recognizing the symptoms, practicing safe sex, and committing to regular STI screenings, you can significantly reduce your chances of developing PID.
Early diagnosis and prompt, complete treatment are your strongest allies in preventing long-term complications.
If you are experiencing any of the symptoms described in this guide, do not wait. Speak to a healthcare provider immediately. Your future reproductive health may depend on it.
Please share this article with friends and loved ones to help raise awareness about this critical women’s health issue.
Disclaimer
The information provided in this article is for educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read here.
Reference
[1] Pelvic Inflammatory Disease – StatPearls – NCBI Bookshelf
https://www.ncbi.nlm.nih.gov/books/NBK499959
[2] Pelvic inflammatory disease (PID) – Symptoms & causes – Mayo Clinic
[3] Pelvic Inflammatory Disease (PID) – ACOG
https://www.acog.org/womens-health/faqs/pelvic-inflammatory-disease
[4] Prevalence of Pelvic Inflammatory Disease in Sexually Experienced …
https://www.cdc.gov/mmwr/volumes/66/wr/mm6603a3.htm
[5] Pelvic Inflammatory Disease (PID) – STI Treatment Guidelines – CDC
https://www.cdc.gov/std/treatment-guidelines/pid.htm
[6] Not All PID is an STD: A Patient’s Perspective on Dismissal, Delay …

