Glaucoma is a group of eye diseases that damage the optic nerve, the vital link between your eye and brain.
This damage is often caused by abnormally high pressure inside your eye and can lead to irreversible vision loss.
It’s a major public health concern, affecting an estimated 80 million people worldwide—a number projected to exceed 111 million by 2040, according to the BrightFocus Foundation.
Because it often develops without early warning signs, it has earned the ominous nickname “the silent thief of sight”.
Understanding this complex condition is the first step toward protecting your vision.
This comprehensive guide will walk you through what glaucoma is, its various types, symptoms, risk factors, and the most advanced diagnostic and treatment options available today.
Read on to empower yourself with the knowledge needed to safeguard your eye health.
In This Article
What is Glaucoma and How Does It Damage Your Vision?
At its core, glaucoma is a neurodegenerative disease affecting the optic nerve.
Think of your eye like a digital camera and the optic nerve as the cable that transmits images to your computer (your brain).
If this cable becomes damaged, the pictures can’t get through, resulting in blind spots in your vision.
Understanding the Optic Nerve: Your Eye’s Data Cable
The optic nerve is a bundle of more than a million tiny nerve fibers.
It’s responsible for carrying visual signals from the retina—the light-sensitive tissue at the back of the eye—to the brain, where they are interpreted as images.
In most types of glaucoma, the progressive death of these nerve fibers leads to a gradual loss of vision.
The Role of Intraocular Pressure (IOP)
Your eye is filled with a clear fluid called aqueous humor, which is constantly produced and drained.
This fluid helps maintain the eye’s shape and provides nutrients.
In a healthy eye, the amount of fluid produced is balanced by the amount that drains out through a spongy tissue called the trabecular meshwork.
When this drainage system becomes inefficient or blocked, the fluid builds up, increasing the pressure inside the eye.
This elevated intraocular pressure (IOP) is a primary risk factor for glaucoma because it exerts force on the delicate optic nerve, causing damage over time.
However, it’s crucial to note that not everyone with high IOP has glaucoma, and some people develop glaucoma with normal IOP.
How Vision Loss Occurs: The “Tunnel Vision” Effect
Glaucoma-related vision loss typically starts with the peripheral (side) vision.
Because our central vision remains sharp in the early stages, these changes often go unnoticed.
Patients may unconsciously turn their heads to compensate for the missing side vision.
As the disease progresses, the field of vision narrows, creating a “tunnel vision” effect.
In the final stages, central vision is also lost, leading to total blindness if left untreated.
What Are the Main Types of Glaucoma?
Glaucoma is not a single disease but a category of conditions.
The main types are distinguished by the state of the drainage angle between the iris and the cornea.
The National Eye Institute provides a clear classification of these types.
Primary Open-Angle Glaucoma (POAG): The Most Common Form
POAG is the most prevalent type of glaucoma, accounting for the vast majority of cases.
In this form, the drainage angle remains “open”, but the trabecular meshwork becomes less efficient at draining fluid over time.
This causes a slow, gradual increase in IOP.
Because it is painless and the vision loss is so gradual, many people are unaware they have it until significant, irreversible damage has occurred.
Acute Angle-Closure Glaucoma: A Medical Emergency
Also known as narrow-angle glaucoma, this type occurs when the drainage angle becomes blocked, preventing aqueous humor from draining at all.
This can happen suddenly when the iris bulges forward and seals off the angle.
The result is a rapid, severe spike in IOP.
Unlike POAG, acute angle-closure glaucoma is a medical emergency with dramatic symptoms, including severe eye pain, nausea, and blurred vision.
Immediate treatment is required to prevent permanent vision loss.
Normal-Tension Glaucoma: A Diagnostic Puzzle
In normal-tension glaucoma (NTG), the optic nerve is damaged even though the intraocular pressure is within the “normal” range.
The exact cause is not fully understood, but experts believe it may be due to an unusually sensitive optic nerve or reduced blood flow to the nerve.
This highlights that while IOP is a major factor, it’s not the only element in the development of glaucoma.
Congenital and Secondary Glaucomas
Secondary glaucoma results from another medical condition, injury or medication.
Causes can include eye injuries, inflammation, tumors, or long-term use of steroid medications.
Congenital glaucoma is a rare form that occurs in infants and young children, caused by incorrect development of the eye’s drainage system before birth.
It requires prompt surgical intervention to preserve vision.
Who is at Risk for Developing Glaucoma?
While anyone can develop glaucoma, certain factors significantly increase your risk.
Being aware of these risks is essential for early detection and prevention.
According to the Mayo Clinic, major risk factors include:
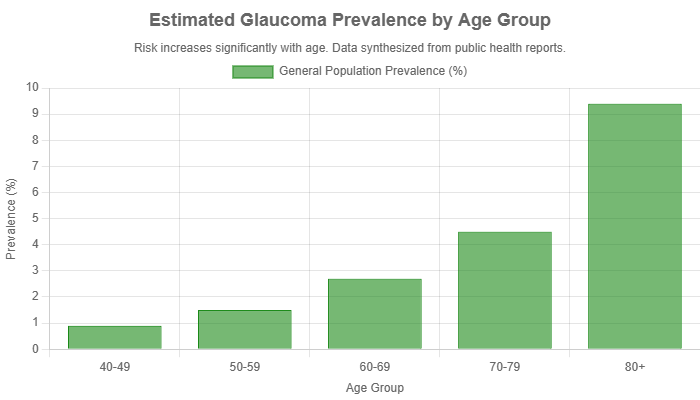
- Age: The risk increases significantly for those over 60.
- Family History: Having a close relative with glaucoma makes you 4 to 9 times more likely to develop it.
- Ethnicity: People of African, Hispanic, or Asian descent are at a higher risk for certain types of glaucoma.
- Medical Conditions: Diabetes, high blood pressure, heart disease, and sickle cell anemia are associated with an increased risk.
- High Intraocular Pressure (IOP): This is the single most important risk factor for developing glaucoma.
- Physical Eye Characteristics: Having thin corneas or optic nerve sensitivity.
- Long-term Steroid Use: Especially steroid eye drops.
- Severe Nearsightedness or Farsightedness.
What Are the Symptoms of Glaucoma?
The symptoms of glaucoma vary widely depending on the type and stage of the disease.
This is where the “silent” nature of the condition becomes most apparent.
Why It’s Called the “Silent Thief of Sight”
For primary open-angle glaucoma (POAG), there are typically no symptoms in the early stages.
No pain, no redness, and no noticeable vision changes.
The increase in eye pressure is slow and painless, and the initial loss of peripheral vision is often subtle enough to be missed.
This lack of warning signs is why regular, comprehensive eye exams are critically important, especially for those with risk factors.
Recognizing Late-Stage Symptoms
As POAG progresses, the following symptoms may become apparent:
- Gradual loss of peripheral (side) vision, often in both eyes.
- Patchy blind spots in your field of view.
- In advanced stages, difficulty with central vision and the development of “tunnel vision”.
Symptoms of Acute Angle-Closure Glaucoma
If you experience a sudden onset of the following symptoms, seek immediate medical attention from an ophthalmologist or go to an emergency room. This could be acute angle-closure glaucoma, which can cause blindness within days if not treated.
- Severe eye pain
- Intense headache
- Nausea and vomiting
- Blurred vision
- Seeing halos or colored rings around lights
- Redness of the eye
How is Glaucoma Diagnosed?
Because glaucoma is often asymptomatic, diagnosis relies on a comprehensive dilated eye exam.
A single test is not enough, an ophthalmologist will perform a series of evaluations to assess your risk and check for damage.
- Tonometry: This test measures your intraocular pressure (IOP). It’s a key part of any glaucoma screening, often performed with a puff of air or a gentle probe that touches the eye’s surface after numbing drops are applied.
- Ophthalmoscopy (Dilated Eye Exam): Your doctor uses drops to dilate your pupils, allowing for a clear view of the optic nerve’s shape and color. Signs of damage, such as cupping (enlargement of the central cup of the optic nerve), are a red flag for glaucoma.
- Perimetry (Visual Field Test): This test maps your complete field of vision to detect any blind spots. You’ll be asked to look straight ahead and indicate when you see a light appear in your peripheral vision.
- Gonioscopy: A special contact lens is placed on your eye to inspect the drainage angle. This helps determine whether you have open-angle or angle-closure glaucoma.
- Pachymetry: This test uses an ultrasonic wave to measure the thickness of your cornea. Corneal thickness can influence IOP readings, so this measurement helps your doctor interpret the results more accurately.
- Optical Coherence Tomography (OCT): This advanced imaging technique provides highly detailed, cross-sectional pictures of your retina and optic nerve, allowing for precise measurement of nerve fiber layer thickness. A recent study in Advances in Glaucoma Diagnosis and Treatment highlights how OCT has revolutionized early detection and monitoring.
What Are the Latest Glaucoma Treatment Options?
While there is no cure for glaucoma, and vision loss cannot be restored, early diagnosis and treatment can halt or slow the disease’s progression and save your remaining sight.
The primary goal of all glaucoma treatment is to lower intraocular pressure.
Prescription Eye Drops: The First Line of Defense
Medicated eye drops are the most common treatment for glaucoma.
They work by either reducing the amount of aqueous humor the eye produces or by improving its drainage.
It is essential to use them exactly as prescribed to keep eye pressure under control.
| Medication Class | Mechanism of Action | Common Examples | Potential Side Effects |
|---|---|---|---|
| Prostaglandin Analogs | Increase the outflow of aqueous humor. | Latanoprost (Xalatan), Travoprost (Travatan Z) | Eye redness, stinging, darkening of iris color, eyelash growth. |
| Beta-Blockers | Decrease the production of aqueous humor. | Timolol (Timoptic), Betaxolol (Betoptic) | Fatigue, shortness of breath, slow heart rate, depression. |
| Alpha-Adrenergic Agonists | Decrease production AND increase outflow of aqueous humor. | Brimonidine (Alphagan P) | Allergic reaction, eye redness, itching, dry mouth. |
| Carbonic Anhydrase Inhibitors | Decrease the production of aqueous humor. | Dorzolamide (Trusopt), Brinzolamide (Azopt) | Stinging or burning in the eye, metallic taste. |
| Rho Kinase Inhibitors | Increase outflow through the trabecular meshwork. | Netarsudil (Rhopressa) | Eye redness, corneal deposits, stinging. |
Laser Therapy: A Minimally Invasive Approach
For patients who cannot tolerate eye drops or for whom they are not effective enough, laser therapy is an excellent option.
These procedures are performed in an ophthalmologist’s office.
- Selective Laser Trabeculoplasty (SLT): This is the most common laser treatment for open-angle glaucoma. It uses a low-energy laser to stimulate the trabecular meshwork, improving its ability to drain fluid. The effects can last for several years.
- Laser Peripheral Iridotomy (LPI): This is the standard treatment for angle-closure glaucoma. The laser creates a tiny hole in the iris, allowing fluid to flow more freely and preventing the iris from blocking the drainage angle.
Surgical Interventions for Glaucoma
When medications and laser therapy are insufficient, surgery may be necessary to create a new drainage channel for the aqueous humor.
- Trabeculectomy: This is a traditional surgical procedure where the surgeon creates a small flap in the sclera (the white of the eye) and removes a piece of the trabecular meshwork, creating a new drainage pathway.
- Glaucoma Drainage Devices (Shunts): Also known as aqueous shunts or valves, these tiny tubes are implanted in the eye to divert aqueous humor to a collection area, from which it is absorbed into the bloodstream.
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS refers to a group of newer surgical procedures that use microscopic devices to reduce eye pressure. They are generally safer and have a faster recovery time than traditional surgery, but may not lower pressure as dramatically. The American Academy of Ophthalmology provides ongoing updates on these evolving techniques.
Living with Glaucoma: A Patient’s Guide
A diagnosis of glaucoma can be daunting, but it is a manageable condition.
Adopting a proactive approach to your health is key to preserving your vision and quality of life.
Managing Your Treatment and Medications
Consistency is everything. Adhering to your eye drop schedule is the most critical part of managing your glaucoma.
Use reminders, alarms, or charts to stay on track.
If you experience side effects, talk to your doctor, don’t just stop taking your medication.
There are often alternative treatments available.
Lifestyle, Diet, and Exercise Considerations
While lifestyle changes cannot replace medical treatment, they can support your overall eye health.
Regular, moderate exercise like walking or swimming can help lower IOP.
However, avoid exercises that involve inverted postures (like certain yoga poses) which can increase eye pressure.
A balanced diet rich in leafy greens and antioxidants is also beneficial for optic nerve health.
The Emotional Impact and Finding Support
Receiving a chronic diagnosis can be stressful.
Patients on forums like Reddit often express anxiety about future vision loss and the daily burden of treatment.
It’s important to acknowledge these feelings.
Joining a support group, either online or in person, can connect you with others who understand what you’re going through.
The Glaucoma Research Foundation offers excellent resources and community connections for patients and their families.
What Does the Future Hold for Glaucoma Research?
The field of glaucoma research is incredibly active, with promising developments on the horizon aimed at better diagnosis, treatment, and even nerve regeneration.
Advances in Early Detection and Monitoring
Researchers are developing AI algorithms that can analyze retinal scans (like OCT) to detect signs of glaucoma earlier and more accurately than the human eye.
Home-based tonometry devices are also becoming available, allowing patients to monitor their IOP throughout the day, providing doctors with more comprehensive data.
Neuroprotection: Protecting the Optic Nerve
Current treatments focus on lowering IOP, but they don’t directly protect the optic nerve from damage.
A major goal of future research is neuroprotection—developing drugs that can shield the optic nerve fibers from deteriorating, regardless of eye pressure.
As detailed in a 2024 study on new therapeutic approaches, this is a key area of investigation.
Novel Drug Delivery Systems
To overcome the challenge of daily eye drops, scientists are creating sustained-release drug delivery systems.
These include tiny implants injected into the eye that slowly release medication over several months, or even medicated contact lenses.
This would greatly improve treatment adherence and effectiveness.
Frequently Asked Questions (FAQ) about Glaucoma
1. Can glaucoma be cured?
No, there is currently no cure for glaucoma. Vision loss from the disease is irreversible. However, with early detection and treatment, the progression of the disease can be slowed or stopped, preventing further vision loss.
2. Will I go blind from glaucoma?
With modern treatments and regular monitoring, blindness from glaucoma is uncommon, especially when it’s caught early. The vast majority of patients are able to manage their condition and maintain useful vision throughout their lives.
3. Is glaucoma contagious?
No, glaucoma is not contagious. You cannot catch it from another person. It is a disease related to individual factors like genetics, age, and the physical structure of your eye.
4. Can I prevent glaucoma?
You cannot prevent glaucoma from occurring, but you can prevent significant vision loss from it. The best prevention is regular comprehensive eye exams to detect it early, especially if you have risk factors.
5. Does diet affect glaucoma?
While no specific diet can cure glaucoma, a healthy lifestyle with a diet rich in antioxidants (found in leafy greens and colorful fruits) may support optic nerve health. It’s also important to maintain a healthy weight and manage conditions like diabetes.
6. How often should I get my eyes checked for glaucoma?
The American Academy of Ophthalmology recommends a baseline exam at age 40. After that, your doctor will recommend a schedule based on your age and risk factors, typically every 1-4 years.
7. Are glaucoma eye drops safe?
Yes, glaucoma eye drops are generally safe and effective. Like any medication, they can have side effects. It’s important to discuss any issues with your doctor, who can often find an alternative that works for you.
8. Can children get glaucoma?
Yes, although it is rare. Congenital glaucoma occurs in infants, and juvenile glaucoma can affect children and young adults. It is often linked to genetic factors or other medical conditions.
Conclusion
Glaucoma is a serious and complex disease, but it is not a sentence to blindness.
Knowledge is your most powerful weapon against this “silent thief”.
Understanding the risks, recognizing the (often absent) symptoms, and committing to regular eye care are the cornerstones of preserving your sight.
Breakthroughs in diagnostics and treatments have transformed the outlook for patients, making it more manageable than ever before.
If you are over 40 or have any of the risk factors discussed, the single most important action you can take is to schedule a comprehensive dilated eye exam with an ophthalmologist.
Don’t wait for symptoms to appear. Take a proactive step today to protect your vision for a lifetime.

