Diabetes is a chronic health condition where the body either doesn’t produce enough insulin or can’t effectively use the insulin it produces, leading to high blood glucose (sugar) levels.
This metabolic disorder has reached epidemic proportions globally.
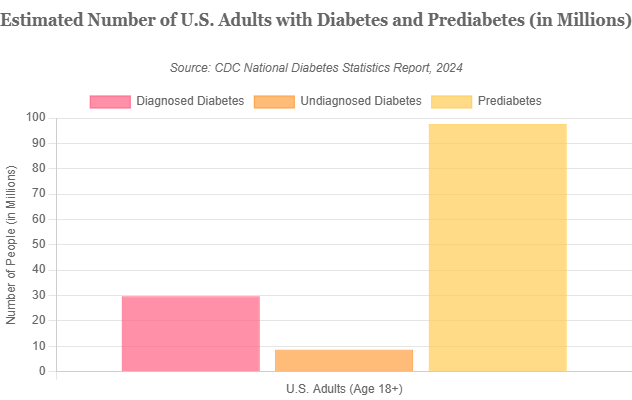
In the United States alone, the latest data reveals a staggering reality: over 38 million people have diabetes, and an additional 97 million adults—more than one in three—have prediabetes, placing them at high risk for developing the full-blown disease.
The economic burden is equally immense, with diagnosed diabetes costing the U.S. an estimated $413 billion in 2022.
Despite these numbers, a diagnosis of diabetes is not a final verdict. It is a starting point for taking control of your health.
This comprehensive guide will empower you with the knowledge to navigate this condition, whether for yourself or a loved one.
We will explore the fundamental differences between the types of diabetes, how to recognize both subtle and overt symptoms, the latest diagnostic and treatment approaches based on 2025 guidelines, and actionable steps for prevention and management.
In This Article
What is Diabetes? Understanding How Your Body Uses Energy
At its core, diabetes is a disease of energy metabolism.
To understand what goes wrong, we must first appreciate the elegant system our bodies use to convert food into fuel.
This process revolves around two key players: glucose and insulin.
The Role of Glucose: Your Body’s Premium Fuel
Think of your body as a high-performance engine. Like any engine, it needs fuel to run.
That fuel is glucose, a simple sugar. Glucose is the primary source of energy for every cell in your body, from the muscles that allow you to walk to the neurons that fire in your brain.
We get glucose primarily from the carbohydrates in the food we eat—things like bread, rice, fruits and vegetables.
When you eat, your digestive system breaks these foods down into glucose, which is then absorbed into your bloodstream.
The Role of Insulin: The Master Key
Once glucose enters the bloodstream, it needs a way to get out of the blood and into the cells where it can be used for energy.
This is where insulin comes in. Insulin is a hormone produced by specialized cells, called beta cells, located in the pancreas, a gland situated behind the stomach.
When your blood glucose levels rise after a meal, your pancreas releases insulin into the bloodstream.
Insulin acts like a key. It travels through the blood to your body’s cells and binds to receptors on the cell surface. This binding “unlocks” the cell, opening a channel that allows glucose to move from the bloodstream into the cell to be used for immediate energy or stored for later use.
This process keeps your blood glucose levels within a narrow, healthy range.
When the system works correctly, your cells get the fuel they need, and your blood sugar doesn’t get too high or too low.
What Goes Wrong in Diabetes?
Diabetes occurs when this finely tuned system breaks down.
The glucose can’t get into the cells efficiently, so it builds up in the bloodstream, a condition known as hyperglycemia (high blood sugar).
This breakdown happens for one of two fundamental reasons:
- Insufficient Insulin Production: The pancreas doesn’t produce enough—or any—insulin. This is like not having enough “keys” to unlock the body’s cells. The glucose is available, but it’s locked out. This is the primary problem in Type 1 diabetes.
- Insulin Resistance: The pancreas produces insulin, but the body’s cells don’t respond to it properly. The “locks” on the cells have become rusty or changed, so the insulin “key” no longer fits well. The pancreas tries to compensate by producing even more insulin, but eventually, it can’t keep up. This is the hallmark of Type 2 diabetes.
In both scenarios, the result is the same: glucose remains trapped in the blood, starving the cells of energy and, over time, causing damage to organs and tissues throughout the body.
Understanding this fundamental mechanism is the first step toward managing and preventing the consequences of diabetes.
What Are the Different Types of Diabetes?
While the common outcome is high blood sugar, the term “diabetes” encompasses several distinct conditions with different causes and demographic profiles.
Recognizing these differences is critical for appropriate diagnosis, treatment and management.
The most prevalent forms are Type 2, Type 1 and gestational diabetes, with prediabetes serving as a crucial warning sign.
Type 2 Diabetes: The Most Common Form
Type 2 diabetes is the most widespread form of the disease, accounting for approximately 90-95% of all diagnosed cases of diabetes.
It is primarily characterized by insulin resistance.
In the initial stages, the body’s cells do not respond effectively to insulin, forcing the pancreas to work overtime to produce more of the hormone to maintain normal blood glucose levels.
Over time, this constant overproduction can exhaust the insulin-producing beta cells in the pancreas, leading to a decline in insulin secretion.
The condition thus evolves from pure insulin resistance to a combination of resistance and relative insulin deficiency.
This process is often gradual, developing over many years, and its symptoms can be so subtle that they go unnoticed, leading to a high number of undiagnosed cases.
The development of Type 2 diabetes is strongly linked to a combination of genetic predisposition and lifestyle factors. Key risk factors include:
- Overweight or obesity
- Physical inactivity
- Family history of diabetes
- Age (risk increases after 45)
- Certain racial and ethnic groups (including African Americans, Hispanic/Latino Americans, American Indians, and some Asian Americans)
Type 1 Diabetes: An Autoimmune Condition
Type 1 diabetes is an autoimmune disease, meaning the body’s own immune system mistakenly attacks and destroys its healthy tissues.
In this case, the immune system targets and eliminates the insulin-producing beta cells in the pancreas.
As a result, the body produces very little or no insulin at all.
Unlike Type 2, Type 1 diabetes is not caused by lifestyle choices and is not preventable.
The exact trigger for this autoimmune attack is unknown but is believed to involve a combination of genetic susceptibility and environmental factors, such as a viral infection.
Once the beta cells are destroyed, they are gone for good, and the individual must take insulin for the rest of their life to survive.
Type 1 diabetes is most often diagnosed in children, adolescents, and young adults, which is why it was formerly known as “juvenile diabetes”.
However, it can develop at any age.
The onset of symptoms is typically abrupt and severe, often leading to a medical emergency if not diagnosed quickly.
Prediabetes: The Critical Warning Stage
Prediabetes is a serious health condition where blood sugar levels are higher than normal but not yet high enough to be diagnosed as Type 2 diabetes.
It is a critical fork in the road. As noted by the CDC, an estimated 97.6 million American adults have prediabetes, and alarmingly, more than 80% of them are unaware of their condition.
This condition indicates that the body is already struggling with insulin resistance or reduced insulin production.
Without intervention, prediabetes often progresses to full-blown Type 2 diabetes within five to ten years.
However, it also represents a crucial opportunity.
With lifestyle changes—such as weight loss, a healthy diet, and increased physical activity—many people with prediabetes can delay or even prevent the onset of Type 2 diabetes.
Gestational Diabetes: During Pregnancy
Gestational diabetes is a type of diabetes that develops during pregnancy in women who did not previously have the condition.
The hormones produced by the placenta to support the growing baby can block the action of the mother’s insulin, leading to insulin resistance and high blood sugar.
The condition is typically diagnosed during the second or third trimester of pregnancy.
While it usually resolves after the baby is born, having gestational diabetes poses risks for both mother and child.
The baby may have excessive growth, leading to complications during delivery, and is at a higher risk of developing obesity and Type 2 diabetes later in life.
The mother also has a significantly increased risk (up to a 50% chance) of developing Type 2 diabetes in the years following the pregnancy .
Other, Rarer Types of Diabetes
To provide a complete picture, it’s important to acknowledge less common forms of diabetes:
- Monogenic Diabetes: These are rare forms caused by mutations in a single gene. The most common types are Maturity-Onset Diabetes of the Young (MODY) and neonatal diabetes. They are often misdiagnosed as Type 1 or Type 2.
- Secondary Diabetes: This form of diabetes develops as a result of another medical condition or treatment. Examples include cystic fibrosis (which can damage the pancreas), pancreatitis, hormonal disorders like Cushing’s syndrome, or the use of certain medications like steroids.
Comparative Overview of Major Diabetes Types
This table provides a clear, at-a-glance comparison of the key features of the main types of diabetes, optimized for quick understanding.
| Feature | Type 1 Diabetes | Type 2 Diabetes | Gestational Diabetes |
|---|---|---|---|
| Primary Cause | Autoimmune destruction of beta cells | Insulin resistance & relative insulin deficiency | Hormonal changes during pregnancy causing insulin resistance |
| Typical Onset | Childhood/Young Adulthood (can be any age) | Adulthood (increasingly in youth) | 2nd or 3rd Trimester of pregnancy |
| Insulin Production | Little to none | Varies, often insufficient or ineffective | Temporarily impaired by hormones |
| Treatment | Insulin is mandatory for survival | Lifestyle changes, oral medications, sometimes injectable medications including insulin | Diet, exercise, sometimes medication (metformin or insulin) |
| Prevention | Not currently preventable | Often preventable or can be delayed with lifestyle changes | Risk may be reduced with a healthy pre-pregnancy lifestyle |
What Are the Early Symptoms and Warning Signs of Diabetes?
Recognizing the symptoms of diabetes is the first step toward diagnosis and management.
However, the signs can be subtle and are often mistaken for other conditions or simply the effects of aging.
The presentation of symptoms also varies significantly between Type 1 and Type 2 diabetes.
The most common early symptoms of diabetes include frequent urination, increased thirst, increased hunger and fatigue.
These signs arise directly from the body’s struggle to manage high blood sugar levels.
The “Classic” Symptoms of High Blood Sugar (Hyperglycemia)
These four symptoms are often referred to as the classic signs of diabetes.
They are a direct physiological response to excess glucose in the bloodstream.
- Frequent Urination (Polyuria): When there is too much glucose in the blood, the kidneys, which act as the body’s filters, work to remove it. To do this, they draw extra water from the body to dilute the glucose and flush it out in the urine. This leads to a noticeable increase in the frequency and volume of urination, especially at night (nocturia).
- Increased Thirst (Polydipsia): The frequent urination causes the body to lose a significant amount of fluid, leading to dehydration. The body’s natural response is to trigger a powerful thirst mechanism to encourage fluid replacement. This can feel like a constant, unquenchable thirst.
- Unexplained Weight Loss: This symptom is more common and pronounced in Type 1 diabetes. When cells cannot get glucose for energy due to a lack of insulin, the body begins to break down muscle tissue and fat stores for fuel. This metabolic shift results in weight loss despite normal or even increased food intake.
- Increased Hunger (Polyphagia): Even though there is plenty of glucose in the blood, it cannot enter the cells to be used for energy. The cells are effectively “starving”. This cellular starvation sends signals to the brain, triggering intense feelings of hunger that may persist even after eating.
Other Common Warning Signs
Beyond the classic symptoms, a range of other signs can indicate the presence of diabetes.
These often develop more gradually, particularly in Type 2 diabetes.
- Fatigue and Weakness: When your cells are deprived of their primary fuel source (glucose), you can feel persistently tired and lethargic, as your body lacks the energy to function optimally.
- Blurred Vision: High blood sugar levels can pull fluid from the lenses of your eyes, affecting their ability to focus. This can cause vision to become blurry. This condition is often temporary and can resolve once blood sugar levels are stabilized.
- Slow-Healing Sores or Frequent Infections: High blood sugar can impair the immune system and damage blood vessels, hindering the body’s natural healing processes. This can make cuts and sores take longer to heal and increase susceptibility to skin, gum and vaginal infections.
- Numbness or Tingling in Hands or Feet (Neuropathy): Over time, high blood sugar can damage nerves, a condition known as diabetic neuropathy. This often begins as a tingling or “pins and needles” sensation in the extremities and can progress to pain or numbness.
- Areas of Darkened Skin (Acanthosis Nigricans): This condition, characterized by dark, velvety patches of skin, typically in the armpits, neck or groin, is a strong indicator of insulin resistance and is commonly seen in individuals with Type 2 diabetes.
How Symptoms Differ Between Type 1 and Type 2
A critical distinction in recognizing diabetes is the speed and intensity of symptom onset.
In Type 1 Diabetes, symptoms tend to appear suddenly and dramatically, often over a period of just a few weeks. The autoimmune destruction of beta cells leads to a rapid and absolute deficiency of insulin, causing blood sugar to rise quickly. This can lead to a life-threatening condition called Diabetic Ketoacidosis (DKA) if not treated promptly.
In Type 2 Diabetes, symptoms develop gradually over several years. Because the body is still producing some insulin and the rise in blood sugar is slow, the signs can be very mild or even completely absent in the early stages. Many people attribute the fatigue or frequent urination to getting older. This insidious onset is why millions of people have Type 2 diabetes and don’t know it, underscoring the vital importance of regular health screenings, especially for those with risk factors.
How is Diabetes Diagnosed? Understanding the Key Tests and Numbers
If you experience symptoms of diabetes or have risk factors for the condition, a healthcare provider can perform simple blood tests to make a definitive diagnosis.
Understanding these tests and the numbers that define normal, prediabetes, and diabetes ranges can empower you to have more informed conversations with your doctor about your health.
The Main Diagnostic Tests for Diabetes
There are three primary tests used to diagnose diabetes. In many cases, a positive result will be confirmed by repeating the test on a different day.
- Hemoglobin A1C (HbA1c) Test: This is a powerful and convenient test that reflects your average blood glucose level over the past two to three months. It measures the percentage of hemoglobin (a protein in red blood cells that carries oxygen) that has become “glycated” or coated with sugar. The higher your blood sugar has been, the higher your A1C level will be. A major advantage of this test is that you do not need to fast beforehand.
- Fasting Plasma Glucose (FPG) Test: This test measures your blood glucose level at a single point in time after you have fasted (not eaten or drunk anything except water) for at least 8 hours, typically overnight. It provides a snapshot of your glucose level when it should be at its lowest.
- Oral Glucose Tolerance Test (OGTT): This test is more involved but can be more sensitive in detecting prediabetes. It measures how your body processes glucose. You will have your blood drawn after an overnight fast, and then you will drink a specially formulated sweet liquid containing a specific amount of glucose. Your blood will be drawn again, usually two hours later, to see how your body has handled the glucose load.
In some cases, such as when a person has symptoms of severe hyperglycemia, a Random Plasma Glucose Test may be used.
This test measures blood sugar without regard to when you last ate.
A level of 200 mg/dL or higher, along with symptoms of diabetes, can confirm a diagnosis.
Diagnostic Criteria for Prediabetes and Diabetes
The American Diabetes Association has established clear numerical criteria for diagnosing prediabetes and diabetes using these tests.
The following table summarizes these values, which are the universal standard in the United States.
| Test | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| A1C | Below 5.7% | 5.7% to 6.4% | 6.5% or higher |
| Fasting Plasma Glucose (FPG) | Below 100 mg/dL | 100 to 125 mg/dL | 126 mg/dL or higher |
| Oral Glucose Tolerance Test (OGTT) (2-hour value) | Below 140 mg/dL | 140 to 199 mg/dL | 200 mg/dL or higher |
Note: A diagnosis of diabetes is typically confirmed with a second test result on a different day, unless there are clear clinical symptoms of hyperglycemia. All diagnostic testing should be performed and interpreted by a qualified healthcare professional.
How is Diabetes Treated? From Lifestyle to Advanced Medicine
The management of diabetes has evolved dramatically over the past two decades.
Today, treatment is not just about lowering blood sugar, it’s about a holistic approach that includes protecting the heart and kidneys, leveraging technology and personalizing care.
The goal is to empower individuals to live long, healthy lives by keeping blood glucose levels in a target range and reducing the risk of complications.
The Foundation: Lifestyle Management
For all types of diabetes, lifestyle management remains the cornerstone of effective treatment. This includes diet, exercise and weight control.
- Healthy Eating: There is no single “diabetes diet”. Instead, the focus is on a balanced eating pattern. A popular and effective strategy is the Diabetes Plate Method, which encourages filling half your plate with non-starchy vegetables, one quarter with lean protein, and one quarter with carbohydrate foods (like whole grains, starchy vegetables, or fruit). For many, learning to count carbohydrates is also a key skill, especially for those on insulin. The emphasis is on whole, unprocessed foods and limiting added sugars and unhealthy fats.
- Physical Activity: Exercise is potent medicine for diabetes. It helps the body use insulin more effectively (improving insulin sensitivity) and helps control weight. The standard recommendation is at least 150 minutes per week of moderate-intensity aerobic activity (like brisk walking, cycling or swimming), spread over several days, plus two or more days of strength training.
- Weight Management: For individuals with Type 2 diabetes who are overweight, weight loss is one of the most impactful interventions. Research from the landmark Diabetes Prevention Program (DPP) showed that losing just 5-7% of body weight can dramatically improve blood sugar control and can even prevent or delay the onset of the disease.
Oral Medications for Type 2 Diabetes
When lifestyle changes alone are not enough to control blood sugar, medication is added.
The landscape of oral medications for Type 2 diabetes is broad and sophisticated.
- Metformin: This is almost always the first-line medication prescribed for Type 2 diabetes. It is safe, effective, and inexpensive. Metformin primarily works by reducing the amount of glucose produced by the liver and also helps to improve the body’s sensitivity to insulin.
- Modern Medication Classes: Beyond metformin, several newer classes of drugs offer significant benefits beyond glucose control. The 2025 treatment guidelines emphasize choosing medications based on a patient’s coexisting conditions, such as heart or kidney disease.
- SGLT-2 Inhibitors (e.g., empagliflozin, canagliflozin): These drugs work by causing the kidneys to excrete excess glucose in the urine. Importantly, they have been shown to provide powerful protection for the heart and kidneys, reducing the risk of heart failure hospitalization and slowing the progression of diabetic kidney disease.
- DPP-4 Inhibitors (e.g., sitagliptin, linagliptin): These medications help the body produce more insulin after meals. They are generally well-tolerated and have a low risk of causing low blood sugar (hypoglycemia).
Injectable Medications: Insulin and Beyond
For some, injectable medications are necessary to achieve target blood sugar levels.
- Insulin Therapy: Insulin is the essential, life-sustaining treatment for everyone with Type 1 diabetes. It is also used by many people with Type 2 diabetes when their pancreas can no longer produce enough insulin on its own. There are many types of insulin, categorized by how quickly they work and how long they last:
- Rapid-acting insulin: Taken just before meals to cover the rise in blood sugar from food.
- Long-acting (basal) insulin: Taken once or twice a day to provide a steady, background level of insulin.
- GLP-1 Receptor Agonists: This class of injectable (and now some oral) medications has revolutionized Type 2 diabetes treatment. Examples include semaglutide, liraglutide, and tirzepatide (which also targets another hormone, GIP). They work by mimicking a natural gut hormone, which stimulates insulin release, suppresses the release of glucagon (a hormone that raises blood sugar), slows digestion, and promotes a feeling of fullness. Recent clinical trials have shown these drugs not only provide excellent glucose control but also lead to significant weight loss and offer strong protection against heart attacks and strokes. A 2024 study highlighted that early, intensive therapy combining drugs like these can lead to more favorable cardiorenal outcomes..
Diabetes Technology: The Modern Toolkit
Technology has transformed daily life with diabetes, moving from reactive to proactive management.
- Blood Glucose Monitoring (BGM) vs. Continuous Glucose Monitoring (CGM): Traditional BGM involves pricking a finger to get a drop of blood for a glucose meter. While still used, it is being rapidly replaced by Continuous Glucose Monitors (CGMs). A CGM uses a tiny sensor inserted just under the skin to measure glucose levels in the interstitial fluid every few minutes, 24/7. This data is sent wirelessly to a smartphone or reader, providing real-time glucose values, trend arrows, and alerts for high or low blood sugar.
- Insulin Pumps and “Artificial Pancreas” Systems: An insulin pump is a small, wearable device that delivers a continuous drip of insulin (basal rate) and allows the user to deliver a bolus dose at mealtimes. The most advanced systems, known as hybrid closed-loop or “artificial pancreas” systems, integrate a CGM with an insulin pump. An algorithm uses the CGM data to automatically adjust the basal insulin delivery, reducing the burden of management and improving time spent in the target glucose range.
Part 6: What Are the Long-Term Complications of Uncontrolled Diabetes?
The primary reason for diligently managing diabetes is to prevent or delay its devastating long-term complications.
Persistent high blood sugar acts like a slow-acting poison, damaging blood vessels and nerves throughout the body.
These complications are broadly divided into two categories: microvascular (affecting small blood vessels) and macrovascular (affecting large blood vessels).
Microvascular Complications (Damage to Small Blood Vessels)
These complications affect the tiny, delicate blood vessels in the eyes, kidneys and nerves.
- Diabetic Retinopathy (Eye Damage): Diabetes is the leading cause of new cases of blindness among working-age adults in the United States. High blood sugar damages the small blood vessels in the retina, the light-sensitive tissue at the back of the eye. This can lead to leakage, swelling, and the growth of fragile new blood vessels, ultimately causing vision loss if not detected and treated early through regular eye exams.
- Diabetic Nephropathy (Kidney Damage): The kidneys are filled with millions of tiny blood vessel clusters (glomeruli) that filter waste from the blood. Diabetes is the number one cause of kidney failure. High blood sugar and high blood pressure overwork the kidneys, damaging this delicate filtering system. Over time, this can lead to chronic kidney disease (CKD) and eventually end-stage renal disease (ESRD), requiring dialysis or a kidney transplant.
- Diabetic Neuropathy (Nerve Damage): This is one of the most common complications of diabetes. High blood sugar injures nerve fibers, most often in the legs and feet (peripheral neuropathy). Symptoms can range from tingling, burning pain and extreme sensitivity to complete numbness. This loss of sensation is particularly dangerous, as it can allow injuries to the feet (cuts, blisters) to go unnoticed, leading to severe infections and, in the worst cases, amputations.
Macrovascular Complications (Damage to Large Blood Vessels)
High blood sugar accelerates atherosclerosis, the process where fatty plaques build up and harden the arteries.
This affects the large blood vessels that supply the heart, brain and limbs.
- Cardiovascular Disease (Heart Disease and Stroke): This is the leading cause of death for people with diabetes. The risk of having a heart attack or stroke is two to four times higher for adults with diabetes than for those without. Atherosclerosis can narrow the coronary arteries, leading to chest pain (angina) or a heart attack. It can also affect the arteries leading to the brain, increasing the risk of stroke.
- Peripheral Artery Disease (PAD): This refers to the narrowing of arteries that supply blood to the limbs, most commonly the legs. It can cause leg pain when walking (claudication) and, by reducing blood flow, further increases the risk of foot ulcers and amputations.
Other Health Concerns
The impact of diabetes extends beyond blood vessels and nerves. It can also increase the risk of:
- Skin Conditions: Including bacterial and fungal infections.
- Hearing Impairment: Hearing problems are more common in people with diabetes.
- Dementia: Type 2 diabetes may increase the risk of Alzheimer’s disease and other forms of dementia.
- Depression: The daily burden of managing a chronic illness makes depression a common co-occurring condition.
The good news is that these complications are not inevitable. Decades of research have proven that by managing blood glucose, blood pressure, and cholesterol levels, and by not smoking, individuals with diabetes can significantly reduce their risk of developing these serious health problems.
Can You Prevent or Reverse Diabetes?
This is one of the most frequently asked and hopeful questions surrounding diabetes.
The answer is nuanced and depends entirely on the type of diabetes.
While Type 1 is not preventable, the story for Type 2 is dramatically different, with powerful evidence supporting both prevention and the concept of remission.
Preventing Type 2 Diabetes: A Proven Strategy
The ability to prevent Type 2 diabetes is not a theoretical concept, it is a scientifically proven reality.
The landmark Diabetes Prevention Program (DPP), a major multicenter clinical research study, provided definitive evidence.
The study found that participants at high risk for diabetes who engaged in an intensive lifestyle change program—focused on healthy eating and physical activity—reduced their risk of developing Type 2 diabetes by 58% over three years.
This was even more effective than the medication metformin, which reduced risk by 31%.
The key actionable steps for preventing Type 2 diabetes are clear and accessible:
- Achieve and Maintain a Healthy Weight: Losing even a modest amount of weight (5-10% of your starting body weight) can make a huge difference. For a 200-pound person, this means losing just 10-20 pounds.
- Engage in Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity exercise per week, such as a 30-minute brisk walk five days a week. Exercise makes your body’s cells more sensitive to insulin.
- Adopt a Balanced, Whole-Foods-Based Diet: Focus on a diet rich in vegetables, fruits, whole grains and lean proteins. Minimize processed foods, sugary drinks, and unhealthy fats. The Mediterranean diet and DASH diet are excellent models.
- Manage Stress and Get Adequate Sleep: Chronic stress and poor sleep can affect hormones that regulate blood sugar and can lead to weight gain, increasing diabetes risk.
The Concept of “Remission” in Type 2 Diabetes
For individuals who have already been diagnosed with Type 2 diabetes, the concept of “remission” offers significant hope.
It is crucial to understand that remission is not a cure.
A cure would imply the underlying disease process is gone forever.
Remission means that blood glucose levels have returned to a normal, non-diabetic range (an A1C below 6.5%) without the need for any diabetes medications.
The primary driver of Type 2 diabetes remission is significant weight loss.
Research, such as the Diabetes Remission Clinical Trial (DiRECT) in the U.K., has shown that a structured, low-calorie weight management program can lead to remission in a substantial number of people.
In the DiRECT study, nearly half (46%) of participants who followed the program were in remission after one year.
The “Twin Cycle Hypothesis”, proposed by Professor Roy Taylor, suggests that Type 2 diabetes is caused by excess fat accumulation in the liver and pancreas, which impairs their function.
Substantial weight loss can remove this excess fat, allowing these organs to function normally again.
Remission is most achievable for those who have had diabetes for a shorter duration (e.g., less than 6 years) and who are able to achieve and sustain a significant weight loss (typically 22-33 pounds or more).
It is important to note that remission may not be permanent. If weight is regained, the diabetes will likely return.
Therefore, it requires a lifelong commitment to maintaining a healthy lifestyle.
The concept of remission does not apply to Type 1 diabetes, as the autoimmune destruction of beta cells is irreversible.
Frequently Asked Questions (FAQ) about Diabetes
Here are direct answers to some of the most common questions people have about diabetes.
1. What is a normal blood sugar level?
For someone without diabetes, a normal fasting blood sugar level (after not eating for at least 8 hours) is between 70 and 99 mg/dL. A normal level two hours after eating is typically below 140 mg/dL.
2. Is diabetes genetic?
Both major types have a genetic component. Type 1 diabetes has a weaker genetic link but requires a genetic predisposition. Type 2 diabetes has a much stronger genetic link, if you have a parent or sibling with Type 2, your risk is significantly higher. However, for Type 2, lifestyle factors play a crucial role in triggering the disease.
3. Can eating too much sugar cause diabetes?
Indirectly, yes for Type 2. A diet high in sugar and calories can lead to weight gain and obesity, which are major risk factors for developing insulin resistance and Type 2 diabetes. However, sugar consumption itself does not cause the autoimmune reaction of Type 1 diabetes.
4. Can you have diabetes and not know it?
Absolutely. This is very common with Type 2 diabetes, where symptoms can be mild or absent for many years. The CDC estimates that over 8.5 million adults in the U.S. have undiagnosed diabetes. This is why regular screening is so important for those at risk.
5. What is the difference between mg/dL and mmol/L?
These are two different units of measurement for blood glucose concentration. Milligrams per deciliter (mg/dL) is the standard unit used in the United States. Millimoles per liter (mmol/L) is the standard in the United Kingdom, Canada, and many other countries. To convert from mg/dL to mmol/L, you divide by 18.
6. Is there a special diet for diabetes?
There is no single “diabetes diet”. The focus is on a healthy, balanced eating plan that is rich in nutrients and low in unhealthy fats and added sugars. Key principles include portion control, carbohydrate awareness, and emphasizing non-starchy vegetables, lean protein, and whole grains.
7. Do I have to give up all my favorite foods?
No. A healthy eating plan for diabetes is about balance and moderation, not deprivation. With guidance from a registered dietitian or diabetes educator, you can learn how to incorporate your favorite foods into your meal plan in a way that doesn’t cause large spikes in blood sugar.
8. Is Type 2 diabetes worse than Type 1?
Neither type is “worse” than the other. Both are serious, chronic conditions that require diligent, lifelong management to prevent severe complications. They simply have different underlying causes and require different treatment strategies. Both can be managed effectively to allow for a long and healthy life.
Conclusion
Diabetes, in its various forms, represents one of the most significant public health challenges of our time.
It is a complex condition rooted in the body’s fundamental process of energy management.
From the autoimmune attack of Type 1 to the insidious onset of insulin resistance in Type 2, the result is a metabolic disruption that, if left unchecked, can have profound consequences on nearly every organ system.
However, a diagnosis of diabetes is far from a sentence to poor health.
The key message of this guide is one of empowerment through knowledge.
Understanding your specific type of diabetes, recognizing the early warning signs, and engaging with the diagnostic process are the first critical steps.
Modern medicine has provided an extraordinary toolkit for management—from foundational lifestyle interventions and effective oral medications to revolutionary injectable therapies and transformative technologies like CGMs and automated insulin delivery systems.
We now know that for the millions at risk, Type 2 diabetes is largely preventable.
For those already diagnosed, the concept of remission through dedicated lifestyle change is a tangible and achievable goal.
For everyone living with the condition, diligent management of blood glucose, blood pressure, and cholesterol can dramatically reduce the risk of complications, paving the way for a long, active, and fulfilling life.
If you have recognized any of the symptoms or risk factors discussed in this guide, the most important action you can take is to speak with a healthcare provider.
Early detection and proactive management are your most powerful allies.
We encourage you to share this information with friends, family, and anyone who might benefit from a deeper understanding of diabetes.
Knowledge is the first and most critical prescription.
References
- Centers for Disease Control and Prevention. (2024). National Diabetes Statistics Report. U.S. Department of Health and Human Services.
- American Diabetes Association. (2023). Statistics About Diabetes.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (2022). What Is Diabetes?.
- Mayo Clinic. (2024). Diabetes – Symptoms and causes.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The Diabetes Prevention Program (DPP).
- Moiz, A., et al. (2024). A Systematic Review and Meta-Analysis of Randomized Controlled Trials on Semaglutide for Weight Loss. PubMed.
- Anson, M., et al. (2024). Treating Type 2 Diabetes With Early, Intensive, Multimodal Pharmacotherapy: Real-World Evidence. Journal of Diabetes Research.
- American Heart Association. Cardiovascular Disease & Diabetes.
- Lean, M. E., et al. (2018). Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. The Lancet.
- Taylor, R. (2024). Understanding the cause of type 2 diabetes. The Lancet Diabetes & Endocrinology.

