Carpal tunnel syndrome is a common condition that causes numbness, tingling and weakness in the hand and arm.
It occurs when the median nerve, one of the major nerves to the hand, is squeezed or compressed as it travels through the wrist.
This condition is surprisingly widespread, with a 2024 systematic review estimating that it affects approximately 14.4% of the global population, making it one of the most prevalent nerve entrapment disorders worldwide.
This guide will provide a definitive overview of carpal tunnel syndrome, from its underlying anatomy and symptoms to the most effective diagnostic methods, treatments and prevention strategies.
By understanding the complete picture, you can take informed steps toward managing your symptoms and protecting your hand health for the long term.
In This Article
What Exactly Is Carpal Tunnel Syndrome?
A Squeeze on a Critical Nerve
At its core, carpal tunnel syndrome (CTS) is a compressive neuropathy.
This means it’s a condition caused by direct pressure on a nerve. In this case, the affected nerve is the median nerve.
This nerve is a vital communication highway, running from your forearm into your hand. It provides sensation (feeling) to your thumb, index finger, middle finger and half of your ring finger.
It also controls the muscles around the base of your thumb (the thenar muscles), which are crucial for pinching and gripping.
When the space within the wrist’s carpal tunnel narrows for any reason, pressure builds on the median nerve. This pressure disrupts the nerve’s function, leading to the classic symptoms of numbness, tingling, and eventually, weakness.
Think of it like a garden hose being kinked—the flow of water (nerve signals) is interrupted, affecting everything downstream.
Understanding the Anatomy: The Carpal Tunnel
To understand what is carpal tunnel syndrome, you must first understand the carpal tunnel itself.
It’s not a disease but a physical structure—a narrow, rigid passageway in your wrist.
The floor and sides of this tunnel are formed by the small wrist bones, known as carpal bones.
The roof is a strong, fibrous band of connective tissue called the transverse carpal ligament.
This tunnel is a crowded space. Packed inside are nine tendons that flex your fingers and thumb, along with the median nerve.
Because the tunnel’s boundaries are so rigid (bone and a tough ligament), there is very little room for expansion.
According to the American Society for Surgery of the Hand (ASSH), any swelling of the tendons or thickening of the ligament can reduce the available space and compress the median nerve, triggering the symptoms of CTS.
Who Is at Risk for Carpal Tunnel?
Prevalence and Demographics
While anyone can develop carpal tunnel syndrome, it is far from random. Certain populations are significantly more susceptible.
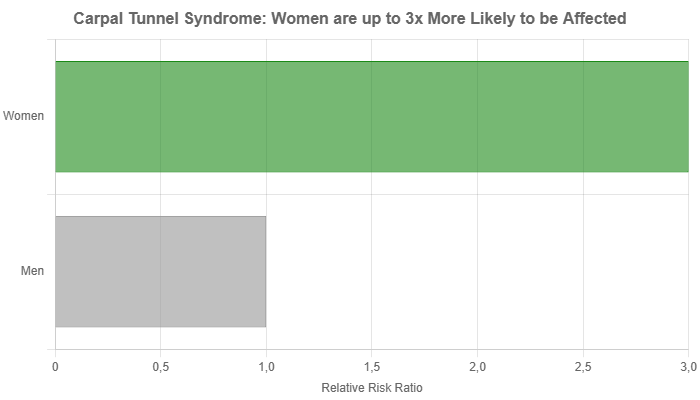
The condition is most common in adults, with symptoms often beginning between the ages of 40 and 60. One of the most striking demographic factors is gender.
Women are up to three times more likely than men to develop carpal tunnel syndrome.
The Mayo Clinic suggests this may be because the carpal tunnel itself is often smaller in women.
Hormonal fluctuations related to pregnancy and menopause, which can cause fluid retention, are also believed to be contributing factors.
Key Risk Factors You Should Know
Carpal tunnel syndrome is often the result of a combination of factors rather than a single cause.
These risk factors increase pressure on the median nerve. They can be broadly categorized as follows:
- Anatomical Factors: A wrist fracture or dislocation can alter the bone structure and narrow the tunnel. Additionally, some people are simply born with smaller carpal tunnels, predisposing them to the condition.
- Medical Conditions: Certain health issues are strongly linked to CTS. These include:
- Inflammatory Conditions: Rheumatoid arthritis and other inflammatory diseases can cause swelling in the wrist.
- Diabetes: This condition can cause generalized nerve damage, making the median nerve more vulnerable to compression.
- Thyroid Disorders: An underactive thyroid (hypothyroidism) is a known risk factor.
- Obesity: Higher body weight is associated with an increased risk of CTS.
- Fluid Retention: Conditions like pregnancy, menopause, or kidney failure can increase fluid in the body, raising pressure within the carpal tunnel.
- Lifestyle and Occupational Factors: While the link between specific jobs and CTS is complex, certain activities are known to aggravate the condition. These include:
- Repetitive Wrist Flexion: Assembly line work or any task requiring prolonged or repeated bending of the wrist.
- Use of Vibrating Tools: Operating jackhammers, sanders or other high-vibration machinery.
- Prolonged Awkward Postures: Holding a phone, book, or steering wheel for long periods can trigger symptoms. The connection to computer use is debated, but poor ergonomics can certainly contribute to wrist strain.
What Are the Symptoms of Carpal Tunnel Syndrome?
The symptoms of carpal tunnel typically start gradually and can fluctuate.
They often affect the thumb, index, middle, and the thumb-side of the ring finger.
The little finger is usually spared, as it is supplied by a different nerve (the ulnar nerve).
Recognizing the progression of symptoms is key to seeking timely treatment.
Early Warning Signs
“Symptoms often first appear in one or both hands at night… You might wake up and feel you need to ‘shake out’ your hand or wrist.” – National Institute of Neurological Disorders and Stroke (NINDS)
The initial signs are often subtle and intermittent:
- Nocturnal Numbness and Tingling: Waking up at night with a “pins and needles” sensation in your hand is a hallmark early symptom. This happens because people often sleep with their wrists bent, which increases pressure in the carpal tunnel.
- The “Shake Out” Maneuver: Many people instinctively shake their hands to try and restore normal feeling upon waking.
- Daytime Symptoms with Specific Activities: You might notice tingling or numbness while driving, holding a phone or reading.
Progressive Symptoms
As the nerve compression worsens, symptoms become more persistent and noticeable during the day.
- Increased Frequency: The episodes of numbness and tingling become more frequent and last longer.
- Radiating Sensations: The tingling or a dull ache may travel from the wrist up into the forearm.
- Clumsiness and Weakness: You may find yourself dropping objects more often. This can be due to the numbness or a developing weakness in the thumb’s pinching muscles. Difficulty with fine motor tasks like buttoning a shirt or handling small coins becomes apparent.
Severe and Chronic Symptoms
If left untreated, carpal tunnel syndrome can lead to permanent nerve damage. The signs of severe CTS are a clear signal that medical intervention is urgently needed.
- Constant Numbness: The intermittent tingling gives way to a constant loss of sensation in the fingers.
- Muscle Atrophy: The thenar muscles at the base of the thumb may visibly shrink and waste away (thenar atrophy). This is a late-stage sign and indicates significant muscle damage.
- Loss of Temperature Sensation: You may lose the ability to distinguish between hot and cold in the affected fingers.
How Is Carpal Tunnel Syndrome Diagnosed?
The Diagnostic Process: What to Expect
A correct diagnosis is crucial because many other conditions can mimic the symptoms of CTS.
A healthcare provider will typically use a combination of patient history, physical examination and specialized tests.
Patient History and Physical Examination
Your doctor will start by asking detailed questions about your symptoms, daily activities and medical history.
They will then perform a physical exam of your hands, arms, shoulders and neck to rule out other causes. This includes:
- Checking for Sensation: Testing the feeling in your fingers and hand.
- Assessing Muscle Strength: Looking for any weakness or atrophy in the thumb muscles.
- Provocative Tests: These maneuvers are designed to temporarily increase pressure on the median nerve to see if they reproduce your symptoms. Common tests include:
- Tinel’s Sign: The doctor gently taps over the median nerve at your wrist. A tingling or shock-like sensation in the fingers suggests CTS.
- Phalen’s Test (Wrist Flexion): You’ll be asked to press the backs of your hands together with your wrists fully flexed for about 60 seconds. If this triggers numbness or tingling, the test is positive.
- Durkan’s Test (Carpal Compression): The examiner applies firm pressure directly over the carpal tunnel for up to 30 seconds to see if symptoms appear.
Confirmatory Tests: EMG and Nerve Conduction Studies
While a physical exam is often highly suggestive, the gold standard for confirming a carpal tunnel diagnosis and assessing its severity is electrodiagnostic testing.
These tests measure how well your median nerve is functioning.
- Nerve Conduction Study (NCS): This is the primary test. Small electrodes are placed on your hand and wrist. The test measures the speed and strength of electrical signals as they travel down the median nerve. A slowing of the signal as it crosses the carpal tunnel is a definitive sign of compression.
- Electromyography (EMG): This test is often done alongside an NCS. A fine needle electrode is inserted into a muscle (usually at the base of the thumb) to measure its electrical activity. An EMG can detect muscle damage resulting from severe nerve compression and helps rule out nerve problems originating in the neck or arm.
What Are the Treatment Options for Carpal Tunnel?
The goal of carpal tunnel treatment is to relieve pressure on the median nerve.
The best approach depends on the severity and duration of your symptoms.
Treatment typically starts with conservative, non-surgical methods.
Non-Surgical Treatments: The First Line of Defense
For mild to moderate cases, non-surgical options are often very effective at managing symptoms and preventing progression.
A recent Cochrane review highlighted that multimodal non-operative treatments can be beneficial, though surgery may offer more symptom improvement in the long run for many. (Lusa V, et al., 2024).
| Treatment Option | How It Works | Best For | Considerations |
|---|---|---|---|
| Wrist Splinting / Brace | Keeps the wrist in a neutral position, especially at night, to maximize space in the carpal tunnel and reduce pressure on the nerve. | Mild to moderate symptoms, particularly nocturnal (nighttime) tingling and numbness. | A simple, low-risk first step. A carpal tunnel brace is widely recommended. |
| Corticosteroid Injections | A powerful anti-inflammatory medication is injected directly into the carpal tunnel to reduce swelling around the tendons. | Providing rapid, temporary relief for moderate symptoms. Can also be used as a diagnostic tool. | Relief may last for several weeks or months, but symptoms often return. Effects can diminish with repeated injections. |
| Activity Modification | Identifying and altering or avoiding activities that trigger symptoms. This includes taking frequent breaks and improving ergonomics. | Symptoms clearly linked to specific repetitive tasks or postures. | Crucial for long-term management, both with and without other treatments. |
| Oral Medications (NSAIDs) | Nonsteroidal anti-inflammatory drugs like ibuprofen or naproxen can help relieve pain and reduce inflammation. | Short-term relief of associated pain and discomfort. | Generally less effective than injections for treating the underlying nerve compression, but can help with symptom management. |
Surgical Treatments: When Is It Necessary?
Surgery is recommended when non-surgical treatments fail to provide adequate relief, or when symptoms are severe and persistent (e.g., constant numbness, muscle weakness or atrophy).
The procedure, known as a carpal tunnel release, aims to permanently increase the size of the tunnel to relieve pressure on the nerve.
The surgery involves cutting the transverse carpal ligament, which forms the roof of the tunnel.
This releases the pressure on the median nerve. There are two main surgical techniques:
- Open Carpal Tunnel Release: The surgeon makes a small incision (about 1-2 inches) in the palm of the hand to directly view and cut the ligament. This is the traditional method and has a very high success rate.
- Endoscopic Carpal Tunnel Release: This technique uses one or two smaller incisions (about half an inch) and a miniature camera (endoscope) to guide the surgeon in cutting the ligament from the inside. This may result in slightly less post-operative pain and a faster return to some activities.
A newer, even less invasive option is ultrasound-guided carpal tunnel release, where the surgeon uses real-time ultrasound imaging to guide a tiny instrument to cut the ligament without a traditional incision.
Research, such as a 2024 study in JHS GO, shows promising clinical results with this technique (Cano LC, et al., 2024).
Can Exercises and Lifestyle Changes Help?
Yes, for many individuals, especially those with mild symptoms, specific exercises and ergonomic adjustments can make a significant difference in managing and preventing carpal tunnel syndrome.
Effective Carpal Tunnel Exercises
The goal of carpal tunnel exercises is to help the median nerve and flexor tendons glide more freely within the carpal tunnel.
The American Academy of Orthopaedic Surgeons (AAOS) recommends several “gliding” exercises. Perform these gently and stop if you feel sharp pain.
Tendon and Nerve Gliding Exercises (Repeat 5-10 times, several times a day):
- Starting Position: Begin with your wrist in a neutral, straight position, fingers and thumb extended upwards.
- Hook Fist: Bend your fingertips down to touch the top of your palm.
- Full Fist: Make a full, gentle fist.
- Tabletop: Keep your knuckles bent but straighten your fingers so your hand looks like a flat tabletop.
- Straight Fist: Keep your fingers straight and bend at the knuckles, as if pointing down.
- Return to Start: Straighten your fingers and wrist again.
These movements encourage the nerve and tendons to move, which can help reduce adhesions and improve circulation.
Workplace Ergonomics: A Guide to Prevention
Creating an ergonomic workspace is one of the most powerful preventive measures you can take.
The goal is to keep your wrists in a neutral (straight) position as much as possible.
- Adjust Your Chair and Keyboard: Your keyboard should be at a height that allows your forearms to be parallel to the floor, with your wrists straight, not bent up or down.
- Watch Your Posture: Sit up straight, with your shoulders back. Poor posture can cause a chain reaction of nerve compression starting from the neck.
- Use an Ergonomic Mouse: Choose a mouse that fits your hand comfortably and doesn’t force your wrist into an awkward angle. A vertical mouse can be a good option.
- Take Frequent Breaks: Every 30-60 minutes, take a short break to stand up, stretch your hands and wrists and change your position.
- Reduce Force: Relax your grip and type softly. Pounding on the keyboard or gripping a mouse tightly increases strain.
The Role of a Carpal Tunnel Brace
A carpal tunnel brace or splint is a cornerstone of non-surgical treatment. Its primary function is to hold the wrist in a neutral position.
This is especially important at night, as many people unknowingly flex their wrists while sleeping, which compresses the median nerve for hours.
By preventing this, a brace can significantly reduce or eliminate nighttime symptoms and allow the nerve to rest and recover.
Recovery and Life After Treatment
What to Expect After Carpal Tunnel Surgery
Recovery from carpal tunnel release surgery varies depending on the surgical technique and the severity of the nerve compression before the procedure.
- Immediately After: You will likely have a bandage or dressing on your wrist. Your surgeon will encourage you to move your fingers to prevent stiffness.
- First Few Days/Weeks: Some soreness, swelling, and stiffness are normal. Pain is usually well-managed with over-the-counter medication. Lifting restrictions will be in place.
- Return to Activities: Most people can return to light desk work within a few days to a week. Returning to more physically demanding jobs may take several weeks to a few months.
- Full Recovery: While symptom relief (especially of tingling) can be immediate, it can take several months for grip and pinch strength to fully return. Scar tenderness may also persist for a few months.
Long-Term Outcomes and Success Rates
Carpal tunnel release surgery is one of the most successful procedures in all of medicine.
Studies consistently show that success rates are over 90% in terms of symptom relief.
A long-term follow-up study found that over 75% of patients rated their outcome as “cured” years after surgery (Louie, D et al., 2012).
However, if there was severe, long-standing nerve damage before surgery, some residual numbness or weakness may persist.
This underscores the importance of seeking treatment early.
Carpal Tunnel vs. Other Conditions
Hand numbness and pain can arise from various sources.
A key part of diagnosis is differentiating CTS from other conditions, a process known as differential diagnosis.
- Cervical Radiculopathy: A “pinched nerve” in the neck can cause pain, numbness, and tingling that radiates down the arm and into the hand, mimicking CTS. However, it is often associated with neck pain and symptoms may be affected by neck movements.
- Arthritis: Both osteoarthritis and rheumatoid arthritis can cause hand pain and stiffness. Arthritis pain is typically centered in the joints, whereas CTS pain is nerve-related (tingling, burning). However, the inflammation from arthritis can be a contributing cause of CTS.
- Peripheral Neuropathy: This is generalized nerve damage, often caused by diabetes. It typically causes symmetrical numbness and tingling in a “glove and stocking” pattern (affecting both hands and feet), unlike the specific median nerve distribution of CTS.
- Tendonitis: Inflammation of the tendons in the wrist can cause pain and swelling, but usually does not cause the distinct tingling and numbness characteristic of nerve compression.
Frequently Asked Questions (FAQ)
1. Does typing or using a computer cause carpal tunnel syndrome?
While prolonged computer use with poor ergonomics can contribute to wrist strain and aggravate existing CTS, the scientific evidence does not support it as a direct cause. CTS is more strongly linked to genetics, medical conditions and other anatomical factors.
2. Will carpal tunnel go away on its own?
In some cases, such as when it’s caused by pregnancy, symptoms may resolve after childbirth. However, for most people, CTS is a progressive condition that tends to worsen over time without treatment.
3. Is surgery the only option for carpal tunnel?
No. Surgery is typically reserved for severe cases or when conservative treatments like splinting, injections and activity modification have failed. Many people find significant relief with non-surgical methods.
4. How painful is recovery from carpal tunnel surgery?
Most patients report that post-surgical pain is manageable and less severe than the nerve pain they had before the operation. Discomfort is usually controlled with ice, elevation and over-the-counter pain relievers.
5. Can I get carpal tunnel in both hands?
Yes, it is very common for carpal tunnel syndrome to be bilateral (affecting both hands), although one hand is often more symptomatic than the other.
6. What’s the best sleeping position for carpal tunnel?
The best position is with your wrists held straight (neutral). Wearing a wrist splint or brace to bed is the most effective way to ensure your wrists stay in this position while you sleep.
7. Does a carpal tunnel brace actually help?
Absolutely. A brace is one of the most effective non-surgical treatments, especially for relieving nighttime symptoms. It works by preventing wrist flexion, which reduces pressure on the median nerve.
8. Is my hand pain carpal tunnel or arthritis?
The key difference is the type of sensation. CTS typically involves tingling, numbness, or a burning/shock-like feeling. Arthritis pain is usually a deep, aching pain located in the joints, often accompanied by stiffness.
9. Can I still exercise with carpal tunnel?
Yes, but with modifications. Avoid exercises that put heavy strain on your wrists (like certain push-ups or heavy weightlifting). Focus on nerve gliding exercises and activities that don’t involve forceful gripping or wrist bending.
10. How long does it take to diagnose carpal tunnel?
The initial diagnosis can often be made during a single doctor’s visit based on your history and a physical exam. However, scheduling and completing confirmatory tests like an EMG/NCS can take a few weeks.
Conclusion
Carpal tunnel syndrome is more than just a minor annoyance, it’s a progressive condition that can significantly impact your quality of life and ability to perform everyday tasks.
From the first tingles in the night to potential muscle weakness, the symptoms are a clear signal from your body that a critical nerve is under pressure.
The good news is that understanding this condition is the first step toward managing it effectively.
With a wide range of treatments available—from simple ergonomic adjustments and a carpal tunnel brace to highly successful surgical procedures—there is a clear path to relief.
Early diagnosis and intervention are paramount to preventing permanent nerve damage and ensuring the best possible outcome.
If you are experiencing any of the symptoms described in this guide, do not ignore them.
Consult with a healthcare professional to get an accurate diagnosis and discuss a treatment plan tailored to your needs.
By taking proactive steps, you can protect your hands and regain control over your health and well-being.

