Arthritis is a general term for joint inflammation, but it represents more than 100 conditions that cause pain, swelling, and stiffness in joints and connective tissues.
It is a leading cause of disability in the United States, affecting people of all ages, sexes, and races.
In fact, according to the CDC, an estimated 58.5 million U.S. adults currently have some form of arthritis.
While many associate arthritis with the natural wear and tear of aging, its causes are diverse, ranging from autoimmune disorders to genetic predispositions and infections.
Understanding the specific type of arthritis you have is the first and most critical step toward effective management and treatment.
This comprehensive guide will explore the different types of arthritis, their symptoms, causes, and the latest treatment strategies to help you navigate this complex condition and improve your quality of life. Read on to learn more.
In This Article
What Exactly is Arthritis? (A Deeper Definition)
The word “arthritis” literally means joint inflammation (from the Greek words arthron for “joint” and -itis for “inflammation“).
While this definition is accurate, it only scratches the surface of a condition that can impact nearly every aspect of a person’s life.
It’s not a single disease but a complex family of musculoskeletal disorders.
Beyond “Wear and Tear”: Understanding Joint Inflammation
At its core, arthritis involves the breakdown of cartilage.
Cartilage is the firm, flexible connective tissue in your joints that protects them by absorbing the pressure and shock created when you move.
When you have arthritis, this cartilage can become damaged and worn down, leading to bone rubbing against bone.
This causes the hallmark arthritis symptoms of pain, swelling and reduced range of motion.
However, the cause of this cartilage breakdown varies significantly.
In some forms of arthritis, like osteoarthritis, it’s a degenerative process. In others, like rheumatoid arthritis, the body’s own immune system mistakenly attacks the joints, causing inflammation that erodes the cartilage and bone.
The Scope of the Problem: Arthritis by the Numbers
The prevalence of arthritis is staggering and continues to grow as the population ages.
It is a significant public health issue that affects millions and carries a substantial economic burden.
According to a 2024 CDC report, not only do 58.5 million U.S. adults have doctor-diagnosed arthritis, but this number is projected to increase to 78 million by the year 2040. The condition also leads to over $303 billion annually in medical costs and lost earnings. Source: CDC Chronic Disease Indicators
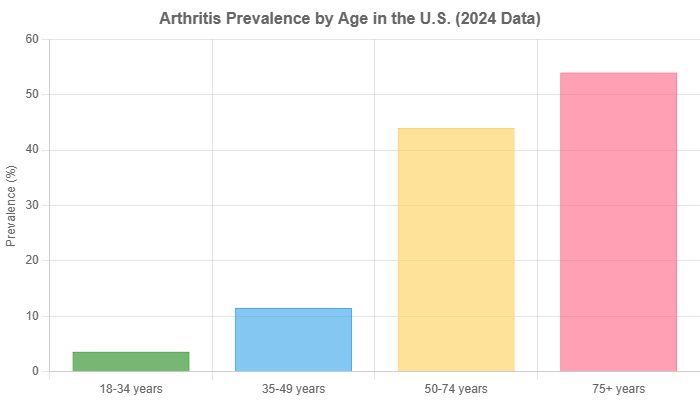
The prevalence of this condition increases sharply with age, but it is not exclusively a disease of the elderly. Millions of working-age adults and even children are affected.
What are the Most Common Types of Arthritis?
While there are over 100 different types of arthritis, a few are responsible for the vast majority of cases.
Understanding the distinctions is crucial because the treatment and management strategies for each are very different.
Osteoarthritis (OA): The “Wear and Tear” Arthritis
Osteoarthritis is the most common form of arthritis, affecting more than 33 million adults in the U.S. alone.
It is a degenerative joint disease that occurs when the protective cartilage on the ends of your bones wears down over time.
While it can damage any joint, OA most commonly affects joints in the hands, knees, hips and spine.
The damage in OA is often a slow, progressive process that worsens with age.
It’s often asymmetrical, meaning it might affect the right knee but not the left.
Symptoms include deep, aching pain, stiffness (especially in the morning or after inactivity) and a grating sensation during movement.
Rheumatoid Arthritis (RA): The Autoimmune Attacker
Rheumatoid arthritis is an autoimmune and inflammatory disease.
This means your immune system mistakenly attacks healthy cells in your body, causing painful swelling, primarily in the lining of the joints (the synovium).
This inflammation can eventually lead to bone erosion and joint deformity.
Unlike the wear-and-tear damage of osteoarthritis, RA can affect more than just your joints. In some people, the condition can also damage a wide variety of body systems, including the skin, eyes, lungs, heart and blood vessels.
RA typically affects joints symmetrically (e.g., both wrists or both ankles) and is characterized by prolonged morning stiffness that can last for hours.
Gout: The Crystal-Induced Arthritis
Gout is a common and complex form of inflammatory arthritis characterized by sudden, severe attacks of pain, swelling, redness, and tenderness in one or more joints, often at the base of the big toe.
It occurs when high levels of uric acid in the blood cause sharp, needle-like crystals (monosodium urate) to form and accumulate in and around a joint.
An attack of gout can occur suddenly, often waking you up in the middle of the night with the sensation that your big toe is on fire.
The affected joint is hot, swollen, and so tender that even the weight of a bedsheet may seem intolerable.
Gout is strongly linked to diet, obesity and genetics.
Psoriatic Arthritis (PsA): The Skin-and-Joint Connection
Psoriatic arthritis is a form of arthritis that affects some people who have the skin condition psoriasis.
Most people develop psoriasis first and are later diagnosed with PsA, but for some, the joint problems begin before skin patches appear.
The main symptoms are joint pain, stiffness, and swelling, which can affect any part of the body, including your fingertips and spine.
Hallmarks of PsA can include “sausage-like” swelling of the fingers or toes (dactylitis) and pitting or separation of the fingernails.
The severity of the skin and joint disease don’t always correlate, you can have mild psoriasis but severe arthritis, or vice versa.
Ankylosing Spondylitis (AS): Arthritis of the Spine
Ankylosing spondylitis is an inflammatory type of arthritis that, over time, can cause some of the small bones in your spine (vertebrae) to fuse.
This fusing makes the spine less flexible and can result in a hunched-forward posture.
It primarily affects the sacroiliac joints, where the spine connects to the pelvis, but can also affect other joints.
Symptoms typically begin in early adulthood and include pain and stiffness in the lower back and hips, especially in the morning and after periods of inactivity.
Men are more likely to develop AS than women.
Juvenile Idiopathic Arthritis (JIA): When Arthritis Affects Children
Juvenile idiopathic arthritis, formerly known as juvenile rheumatoid arthritis, is the most common type of arthritis in children under the age of 16.
It can cause persistent joint pain, swelling and stiffness.
Some children may experience symptoms for only a few months, while others have symptoms for the rest of their lives.
A serious complication of JIA is eye inflammation (uveitis), which can lead to vision loss if not detected and treated early.
Regular eye exams by an ophthalmologist are a critical part of managing this condition.
How Do Osteoarthritis vs. Rheumatoid Arthritis Differ?
Distinguishing between the two most common forms of arthritis, osteoarthritis and rheumatoid arthritis, is essential for proper diagnosis and treatment.
While both cause joint pain, their underlying causes and patterns are vastly different.
This is a key area of focus when discussing the different types of arthritis.
| Feature | Osteoarthritis (OA) | Rheumatoid Arthritis (RA) |
|---|---|---|
| Primary Cause | Mechanical wear and tear, breakdown of cartilage. | Autoimmune disease, immune system attacks the joint lining (synovium). |
| Symptom Onset | Develops slowly over many years. | Can develop relatively quickly, over weeks or months. |
| Joint Pattern | Often asymmetrical (affects one side of the body, e.g., one knee). | Typically symmetrical (affects both sides of the body, e.g., both wrists). |
| Morning Stiffness | Usually lasts less than 30 minutes. | Often lasts for more than an hour. |
| Commonly Affected Joints | Weight-bearing joints (knees, hips), hands, and spine. | Small joints of the hands and feet, wrists, elbows, ankles. |
| Systemic Symptoms | Rare, disease is localized to the joints. | Common, can include fatigue, fever and inflammation of other organs (lungs, heart, eyes). |
What are the Key Symptoms of Arthritis?
While symptoms vary depending on the specific type of arthritis, there are several common signs that point to an inflammatory joint condition.
Recognizing these early can lead to a faster diagnosis and better outcomes.
Universal Symptoms: Pain, Stiffness and Swelling
The most common signs and symptoms of arthritis involve the joints. These include:
- Pain: This can be constant or it may come and go. It may occur only with movement or also at rest.
- Stiffness: Joint stiffness is a classic symptom, particularly upon waking in the morning or after being inactive for a long period.
- Swelling: The skin over the affected joint may become red and swollen, feeling warm to the touch.
- Decreased range of motion: As the arthritis progresses, you may not be able to fully bend or straighten the affected joint.
Type-Specific Symptoms You Shouldn’t Ignore
Beyond the universal symptoms, certain types of arthritis have unique warning signs:
- Rheumatoid Arthritis: Look for symmetrical joint involvement and systemic symptoms like fatigue, low-grade fever and loss of appetite.
- Gout: An intense, sudden attack of pain in a single joint, most often the big toe, is the classic sign.
- Psoriatic Arthritis: Swelling of an entire finger or toe (“sausage digit”), nail changes (pitting), and lower back pain can indicate PsA.
- Ankylosing Spondylitis: Chronic pain and stiffness in the lower back and buttocks that improves with exercise but not with rest.
When to See a Doctor About Your Joint Pain
Occasional aches and pains are normal, but persistent joint symptoms are not.
You should make an appointment with your doctor if you have joint pain that lasts for more than a few days, is accompanied by swelling, redness, and warmth, or interferes with your daily activities.
Early diagnosis and an effective arthritis treatment plan are key to preventing long-term joint damage.
What Causes Arthritis and Who is at Risk?
The causes of arthritis are not fully understood, but a combination of factors appears to play a role.
Some of these you can’t change, while others are modifiable through lifestyle choices.
Unmodifiable Risk Factors: Age, Sex and Genetics
- Age: The risk of developing most types of arthritis, including OA, RA, and gout, increases with age.
- Sex: Women are more likely than men to develop rheumatoid arthritis, while most people who have gout are men. For osteoarthritis, women are also more commonly affected, especially after age 50.
- Family History: Some types of arthritis run in families. If your parents or siblings have the disorder, you may be more likely to develop it. Specific genes have been identified that increase the risk for RA and AS.
Modifiable Risk Factors: Obesity, Injury and Lifestyle
- Obesity: Carrying excess weight puts extra stress on joints, particularly weight-bearing ones like your knees, hips, and spine. According to the Arthritis Foundation, every pound of excess weight exerts about 4 pounds of extra pressure on the knees.
- Previous Joint Injury: People who have injured a joint, such as in a sports accident or a fall, are more likely to eventually develop osteoarthritis in that joint.
- Smoking: Smoking is a significant risk factor for developing rheumatoid arthritis and can also make the disease more severe.
- Occupation: Jobs that involve repetitive squatting, bending, or heavy lifting can put stress on the joints and increase the risk of OA.
The Role of Infection and the Immune System
In some cases, arthritis can be triggered by an infection.
Reactive arthritis is joint pain and swelling triggered by an infection in another part of your body, such as your intestines, genitals or urinary tract.
Septic arthritis is a painful infection in a joint that can come from germs that travel through your bloodstream from another part of your body.
In autoimmune forms of arthritis like RA and PsA, the immune system’s normal defense mechanisms go awry.
Instead of protecting the body, it produces inflammation that attacks its own tissues, leading to joint destruction.
How is Arthritis Diagnosed by Doctors?
A correct diagnosis is the cornerstone of effective arthritis management.
Because there are so many types, a doctor, often a specialist called a rheumatologist, will use a combination of methods to identify the specific cause of your joint pain.
The Diagnostic Process: From Conversation to Confirmation
The diagnostic journey typically begins with a detailed conversation about your symptoms and medical history.
Your doctor will want to know when your symptoms started, what makes them better or worse, which joints are affected and if you have a family history of arthritis.
Physical Examination and Medical History
During the physical exam, your doctor will check your joints for swelling, redness and warmth.
They will also assess your joints’ range of motion.
They will look for patterns in the affected joints (e.g., symmetrical vs. asymmetrical) and check for other physical signs related to specific types of arthritis, like skin rashes (psoriasis) or nodules (RA).
Imaging Tests: X-rays, MRI, and Ultrasound
Imaging tests can help visualize what is happening inside your joints.
- X-rays: These are excellent for revealing cartilage loss, bone damage, and bone spurs. They are often used to track the progression of osteoarthritis.
- Magnetic Resonance Imaging (MRI): MRIs use radio waves and a strong magnetic field to produce detailed images of soft tissues like cartilage, tendons and ligaments.
- Ultrasound: This technology uses sound waves to visualize soft tissues, cartilage, and fluid-filled structures within the joints, and can be used to guide injections.
Laboratory Tests: Blood Work and Joint Fluid Analysis
Analysis of different body fluids can help pinpoint the type of arthritis.
- Blood Tests: Certain blood tests look for markers of inflammation, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Other tests look for specific antibodies, like rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP), which are often present in people with RA.
- Joint Fluid Analysis: Your doctor may use a needle to draw fluid from an affected joint (arthrocentesis). This fluid can be tested for uric acid crystals to confirm a diagnosis of gout, or for bacteria to rule out a joint infection.
What are the Modern Treatment Options for Arthritis?
While there is no cure for most types of arthritis, treatments have improved dramatically in recent years.
The main goals of arthritis treatment are to reduce symptoms, improve joint function, and prevent further damage.
Treatment plans are highly individualized.
Medications: From NSAIDs to Advanced Biologics
A wide range of medications is used to manage arthritis:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter NSAIDs like ibuprofen and naproxen can relieve pain and reduce inflammation. Prescription-strength versions are also available.
- Corticosteroids: These powerful anti-inflammatory drugs, such as prednisone, can be taken orally or injected directly into a joint to quickly reduce inflammation and pain.
- Disease-Modifying Antirheumatic Drugs (DMARDs): These drugs, like methotrexate, are used for inflammatory types of arthritis like RA. They work by slowing or stopping the immune system from attacking the joints.
- Biologic Response Modifiers (“Biologics”): A newer class of DMARDs, biologics are genetically engineered proteins that target specific parts of the immune system that fuel inflammation. They have revolutionized the treatment of RA, PsA and AS.
The Cornerstone: Physical Therapy and Exercise
Exercise is crucial for managing arthritis.
A physical therapist can design a program to improve your range of motion, strengthen the muscles around your joints and reduce pain.
Low-impact activities like swimming, walking, and cycling are particularly beneficial as they strengthen muscles without putting excess stress on joints.
Surgical Interventions: When Is Joint Replacement Necessary?
If conservative measures don’t provide relief, surgery may be an option. Surgical procedures include:
- Joint Repair: In some cases, joint surfaces can be smoothed or realigned to reduce pain and improve function.
- Joint Fusion: This procedure is more often used for smaller joints, such as those in the wrist, ankle and fingers. It involves fusing the ends of the two bones in the joint together, eliminating the joint but also the pain.
- Joint Replacement (Arthroplasty): This procedure removes the damaged joint and replaces it with an artificial one made of metal, plastic, or ceramic. Hips and knees are the most commonly replaced joints.
Emerging Research: A Glimpse into the Future of Arthritis Treatment
The field of rheumatology is constantly evolving. Recent research highlights promising new avenues for treatment.
For example, studies presented in 2024 have explored using CAR-T therapy, originally developed for cancer, to “reset” the immune system in autoimmune diseases like lupus.
Another innovative approach involves using vagus nerve stimulation to reduce inflammation in rheumatoid arthritis.
These cutting-edge therapies offer hope for more effective and personalized treatments in the future. Source: CCRheumatology 2024 Year in Review.
Can Lifestyle Changes Help Manage Arthritis Symptoms?
Yes, absolutely. Alongside medical treatments, lifestyle modifications play a vital role in managing arthritis and improving overall well-being.
Empowering yourself with the right strategies can make a significant difference in your daily life.
The Anti-Inflammatory Diet: Foods That Help and Hurt
While no “miracle diet” cures arthritis, many studies show that an anti-inflammatory diet can help control symptoms.
The Mediterranean diet is often recommended. Key components include:
- Foods to Emphasize: Fatty fish (salmon, mackerel), a wide variety of fruits and vegetables, nuts, olive oil and whole grains.
- Foods to Limit: Processed foods, red meat, sugary drinks, and refined carbohydrates, which can promote inflammation.
The Importance of Weight Management
Maintaining a healthy weight is one of the most effective things you can do to manage arthritis, especially osteoarthritis of the knee and hip.
Losing even a small amount of weight can significantly reduce the stress on your joints, decrease pain and improve function.
The CDC notes that in adults with arthritis, those who are overweight or obese report more severe pain and activity limitations.
Protecting Your Joints in Daily Life
Making small adjustments to your daily activities can help protect your joints and conserve energy.
This includes using assistive devices (like jar openers or canes), alternating between periods of activity and rest, and using good posture and body mechanics when lifting or carrying objects.
How Does Arthritis Impact Quality of Life?
Arthritis is more than just a physical ailment, it can have a profound impact on a person’s mental health, social life and ability to work.
The Physical Toll: Disability and Activity Limitation
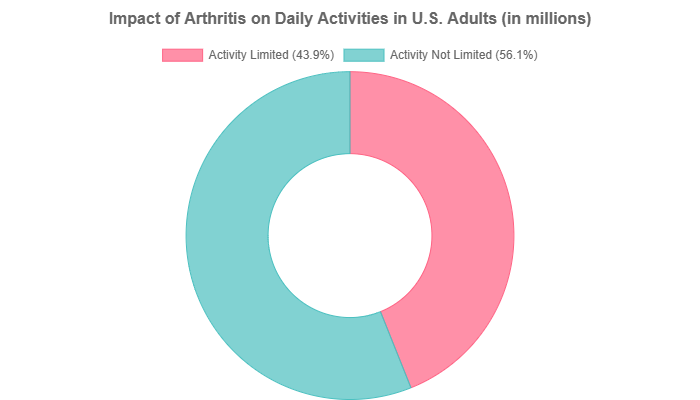
Severe arthritis can make simple daily tasks, like opening a jar or walking up stairs, incredibly difficult. It is a leading cause of work disability in the U.S.
According to the CDC, of the 58.5 million adults with arthritis, about 25.7 million (44%) report that it limits their usual activities.
This loss of function can lead to a loss of independence and a reduced quality of life.
The Mental and Emotional Impact
Living with chronic pain and physical limitations can be emotionally draining.
People with arthritis have a higher risk of developing anxiety and depression compared to the general population.
The unpredictability of flare-ups can create stress and make it difficult to plan social activities, leading to feelings of isolation.
It’s important to address the mental health aspects of arthritis as part of a comprehensive treatment plan.
Frequently Asked Questions (FAQ) About Arthritis
1. Can arthritis be cured?
There is no cure for most types of arthritis. However, with modern treatments and lifestyle management, it is possible to control symptoms, slow disease progression and maintain a high quality of life. Early and aggressive treatment is key.
2. Does cracking your knuckles cause arthritis?
No. This is a common myth. While the sound can be annoying, multiple studies have found no link between the habit of knuckle-cracking and the development of osteoarthritis in the hands.
3. Can weather affect arthritis pain?
Many people with arthritis report that their pain worsens with changes in the weather, particularly with drops in barometric pressure and cold, damp conditions. While the exact mechanism isn’t fully understood, these anecdotal reports are very common.
4. Is arthritis just a disease for old people?
No. While the risk increases with age, arthritis affects people of all ages. In the U.S., nearly 300.000 children have some form of juvenile arthritis, and millions of adults are diagnosed in their 20s, 30s and 40s.
5. What is the difference between a rheumatologist and an orthopedist?
A rheumatologist is a medical doctor who specializes in the non-surgical diagnosis and treatment of inflammatory and autoimmune conditions like RA. An orthopedist is a surgeon who treats musculoskeletal problems, including performing joint replacement surgery for severe OA.
6. Are “natural” supplements effective for arthritis?
Some supplements, like glucosamine/chondroitin for OA and omega-3 fatty acids for RA, have shown modest benefits in some studies, but results are mixed. Always talk to your doctor before starting any supplement, as they can interact with medications.
7. Can I exercise if my joints hurt?
Yes, but it’s important to choose the right kind of exercise. Low-impact activities like swimming, water aerobics, and cycling can strengthen muscles and improve flexibility without stressing joints. A physical therapist can help you create a safe and effective plan.
8. Is there a specific blood test to diagnose all types of arthritis?
No, there is no single test. Diagnosis is based on a combination of your medical history, a physical exam, imaging tests, and various blood tests that look for markers of inflammation or specific antibodies associated with certain types of arthritis.
Conclusion
Arthritis is a complex and multifaceted condition that affects millions of lives.
From the degenerative wear of osteoarthritis to the autoimmune attack of rheumatoid arthritis, each type presents unique challenges.
However, our understanding of these diseases and our ability to treat them has never been better.
By recognizing the symptoms, seeking an early and accurate diagnosis, and working with your healthcare team, you can create a comprehensive management plan.
This plan should combine modern medical treatments with crucial lifestyle strategies like exercise, a healthy diet and weight management.
While a cure may not yet exist, taking proactive control of your joint health is the most powerful step you can take toward living a full and active life despite your arthritis.
If you are experiencing persistent joint pain, don’t ignore it.
Talk to your doctor to begin your journey toward better joint health today.

