Heavy periods, medically known as menorrhagia, are most commonly caused by hormonal imbalances, noncancerous uterine growths like fibroids and polyps, and certain underlying medical conditions or medications.
While often dismissed as “just a bad period”, persistent heavy menstrual bleeding is a recognized medical issue that can significantly impact a person’s health and quality of life.
If you find yourself planning your life around your menstrual cycle, constantly worried about bleeding through clothes, or feeling drained and exhausted, you are not alone.
It’s a widespread concern, in fact, up to one-third of women will seek medical treatment for heavy menstrual bleeding during their lifetime.
This statistic underscores a critical reality: heavy periods are not just an inconvenience but a legitimate health concern that deserves attention and proper management.
This article provides a comprehensive exploration of the multifaceted causes behind heavy periods. We will delve into the specific hormonal, structural, and medical factors that can lead to excessive bleeding.
Furthermore, we will clarify the clinical definition of a “heavy” period, outline the diagnostic process your doctor might follow, and provide an overview of the effective treatment options available today.
Understanding the root cause is the first step toward finding relief—let’s explore what might be happening.
In This Article
What Exactly Is Considered a Heavy Period?
While the experience of a menstrual cycle is unique to each individual, medicine has established clear guidelines to differentiate a normal flow from one that is clinically heavy.
The term menorrhagia refers to menstrual bleeding that is excessive in volume, duration, or both.
While the older clinical definition involved measuring blood loss (more than 80 milliliters, or about 5.5 tablespoons, per cycle), this is impractical for most people to track at home.
Therefore, healthcare providers now rely on a set of practical, symptom-based criteria to diagnose heavy periods. If you experience one or more of the following, you may have menorrhagia:
- Frequent Changes: You need to change your tampon or sanitary pad every hour, or every two hours, for several consecutive hours.
- Doubling Up: You have to use double sanitary protection (e.g., a tampon and a pad) to control your menstrual flow.
- Nighttime Disruptions: You need to wake up during the night specifically to change your sanitary protection.
- Prolonged Bleeding: Your period consistently lasts longer than seven days.
- Large Blood Clots: You regularly pass blood clots that are the size of a quarter or larger.
- Symptoms of Anemia: You experience persistent fatigue, weakness, shortness of breath, dizziness, or have pale skin, which can be signs of iron deficiency due to excessive blood loss.
- Lifestyle Interference: Your menstrual flow is so heavy that it prevents you from doing your normal daily activities, such as going to work, exercising, or attending social events.
If these symptoms resonate with your experience, it is a strong indicator that your bleeding is heavier than the normal range and warrants a discussion with a healthcare professional.
The Core Analysis: Detailed Causes of Heavy Periods
Heavy menstrual bleeding is not a disease in itself but rather a symptom of an underlying issue.
The causes are diverse, ranging from subtle hormonal shifts to structural abnormalities within the uterus.
Understanding these potential triggers is the cornerstone of an accurate diagnosis and effective treatment plan.
How Common Are the Different Causes of Heavy Periods?
The causes of menorrhagia vary significantly based on a woman’s age, genetics, and overall health. However, research provides a general picture of the most frequent culprits.
The chart below illustrates an estimated prevalence of the primary causes of heavy menstrual bleeding, based on clinical data and studies. It’s important to note that an individual may have more than one contributing factor.
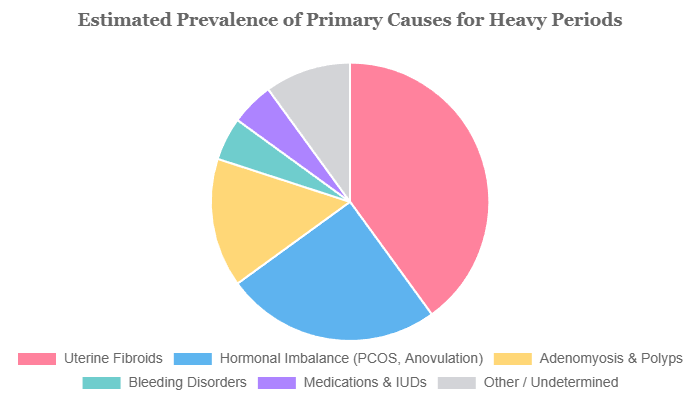
Note: These percentages are estimates and can vary. “Hormonal Imbalance” includes anovulatory cycles, PCOS, and thyroid issues. A significant number of cases may have overlapping causes or remain undetermined.
What Hormonal Imbalances Can Cause Heavy Periods?
The menstrual cycle is a finely tuned orchestra conducted by hormones, primarily estrogen and progesterone. When these hormones are out of sync, the result can be chaotic, often manifesting as heavy or irregular bleeding.
This is one of the most common reasons for menorrhagia, especially in adolescents who have just started menstruating and in women approaching menopause (perimenopause).
Estrogen and Progesterone Imbalance
To understand this, think of the uterine lining (endometrium) as a lawn.
- Estrogen is like the fertilizer, its job in the first half of the cycle is to build up a thick, nutrient-rich endometrial lining to prepare for a potential pregnancy.
- Progesterone, released after ovulation, is like a stabilizing agent. It matures the lining and keeps it intact until either a pregnancy occurs or hormone levels drop, triggering a period.
In a cycle where ovulation does not occur (an anovulatory cycle), the body produces estrogen but very little progesterone. This is called “unopposed estrogen”.
Without progesterone to stabilize it, the endometrium continues to grow thicker and more vascular.
Eventually, this overgrown lining becomes unstable and outgrows its blood supply, leading to a disorganized, heavy, and often prolonged shedding—a heavy period.
Polycystic Ovary Syndrome (PCOS)
PCOS is a common endocrine disorder that is a primary example of chronic hormonal imbalance leading to heavy periods. Women with PCOS often have irregular or infrequent ovulation, leading to long stretches of unopposed estrogen.
This can cause them to miss periods for months at a time. When a period finally does occur, the excessively built-up uterine lining results in a very heavy and prolonged bleed.
Research published in sources like the Journal of Clinical Endocrinology & Metabolism consistently links PCOS with abnormal uterine bleeding patterns, including menorrhagia.
Thyroid Dysfunction
The thyroid gland, located in your neck, is the body’s master metabolic regulator. It also plays a crucial, though often overlooked, role in reproductive health.
Both an underactive thyroid (hypothyroidism) and an overactive thyroid (hyperthyroidism) can disrupt the delicate hormonal balance that governs the menstrual cycle.
Hypothyroidism, in particular, can interfere with ovulation, affect clotting factors, and lead to heavy, prolonged periods.
Because its symptoms (like fatigue) can overlap with those of anemia from heavy bleeding, it’s a critical factor for doctors to investigate.
Can Growths or Issues with My Uterus Cause Heavy Bleeding?
Structural abnormalities within or on the uterus are another major category of causes for heavy periods.
These growths are typically benign (noncancerous), but their size and location can physically interfere with the uterus’s normal function, leading to significant bleeding.
Uterine Fibroids (Leiomyomas)
Fibroids are extremely common muscular tumors that grow in the wall of the uterus. Up to 70-80% of women will have fibroids by age 50, though not all will cause symptoms.
When they do, heavy bleeding is the most common complaint. Fibroids cause menorrhagia in several ways:
- Increased Surface Area: They can enlarge the uterine cavity, creating more endometrial lining to be shed each month.
- Vascular Disruption: They can press on blood vessels or develop their own abnormal vessels, leading to increased blood flow.
- Impaired Contractions: They can prevent the uterus from contracting effectively during menstruation. These contractions are essential for compressing blood vessels and stopping bleeding.
The location of the fibroid matters most. Submucosal fibroids, which bulge into the uterine cavity, are the most likely to cause severe bleeding, even when small.
Intramural fibroids (within the uterine wall) and subserosal fibroids (on the outer surface) can also cause issues if they are large.
Uterine Polyps
Uterine polyps are small, soft, finger-like growths that develop from the endometrium itself. Think of them as skin tags on the inside of the uterus.
While they are also typically noncancerous, they are composed of fragile endometrial tissue and blood vessels.
This fragility means they can bleed spontaneously, leading to bleeding between periods (intermenstrual bleeding) or contributing to a heavier flow during menstruation.
Adenomyosis
Adenomyosis is a more complex and often underdiagnosed condition. It occurs when the endometrial tissue, which normally lines the uterus, begins to grow into the muscular wall of the uterus (the myometrium).
This displaced tissue behaves as it normally would: it thickens, breaks down, and bleeds during each menstrual cycle.
However, because the blood is trapped within the uterine muscle, it causes the uterus to become enlarged, swollen, and tender. This leads to characteristically very heavy, painful periods (dysmenorrhea) and a feeling of pelvic pressure.
“Adenomyosis is often called the ‘evil twin’ of endometriosis. While endometriosis grows outside the uterus, adenomyosis grows inside the uterine wall, causing a boggy, irritated uterus that bleeds heavily.” – A common clinical analogy.
To help clarify these distinct but related conditions, here is a comparative table:
| Condition | What It Is | How It Causes Bleeding | Common Associated Symptoms |
|---|---|---|---|
| Uterine Fibroids | Benign tumors of uterine muscle tissue. | Increases uterine surface area; distorts cavity; prevents proper uterine contractions to stop bleeding. | Heavy bleeding, pelvic pressure or pain, frequent urination, backache. |
| Uterine Polyps | Small, fragile growths of the uterine lining (endometrium). | Fragile tissue and blood vessels can bleed easily, contributing to overall flow or causing spotting. | Heavy bleeding, irregular bleeding, bleeding between periods, postmenopausal bleeding. |
| Adenomyosis | Uterine lining tissue grows into the muscular wall of the uterus. | Trapped tissue bleeds within the muscle, causing inflammation, an enlarged uterus, and poor contractions. | Severely heavy and painful periods, chronic pelvic pain, painful intercourse, enlarged/tender uterus. |
What Medical Conditions are Linked to Heavy Periods?
Beyond hormonal and structural issues, several systemic medical conditions can manifest as heavy menstrual bleeding. In these cases, menorrhagia is a symptom of a body-wide problem.
Bleeding Disorders
For some individuals, heavy periods are the first and most obvious sign of an underlying, often inherited, bleeding disorder. Conditions like Von Willebrand disease, the most common inherited bleeding disorder, impair the blood’s ability to form a stable clot.
During menstruation, when hundreds of tiny blood vessels in the uterine lining are exposed, an effective clotting process is essential to control blood loss. If this process is faulty, bleeding can be excessive and prolonged.
According to the American College of Obstetricians and Gynecologists (ACOG), up to 20% of adolescents with severe menorrhagia may have an underlying bleeding disorder.
Pelvic Inflammatory Disease (PID)
PID is an infection of the female reproductive organs, including the uterus, fallopian tubes, and ovaries. It’s most often caused by sexually transmitted bacteria that spread from the vagina.
The infection causes significant inflammation and irritation of the pelvic organs. This inflammation can disrupt the normal cycle and lead to a range of bleeding problems, including heavy periods, irregular bleeding, and pain.
Liver or Kidney Disease
Advanced chronic diseases of the liver or kidneys can have a profound impact on the entire body, including the menstrual cycle. The liver is crucial for metabolizing hormones and producing proteins necessary for blood clotting.
When liver function is impaired (e.g., in cirrhosis), hormone levels can become imbalanced, and clotting factors can be depleted, leading to a tendency for increased bleeding.
Similarly, chronic kidney disease can affect hormone regulation and contribute to anemia, exacerbating the effects of heavy periods.
Endometrial Hyperplasia and Cancer (Important Disclaimer)
This is a less common but critically important cause to rule out. Endometrial hyperplasia is a condition where the uterine lining becomes abnormally thick due to an overgrowth of cells, usually from prolonged unopposed estrogen.
While it is a benign condition, certain types of hyperplasia (atypical hyperplasia) are considered precancerous and increase the risk of developing endometrial (uterine) cancer.
Both endometrial hyperplasia and endometrial cancer can cause abnormal uterine bleeding, including very heavy periods or postmenopausal bleeding.
While the vast majority of heavy periods are NOT caused by cancer, it is a possibility that your doctor must consider, especially if you are postmenopausal, have risk factors like obesity or PCOS, or experience a sudden, significant change in your bleeding pattern.
Disclaimer: Any instance of bleeding after menopause requires immediate medical evaluation. If you have risk factors or concerning symptoms, it is essential to consult a healthcare provider to rule out serious conditions.
Can Medications or Medical Devices Cause Heavy Periods?
Sometimes, the cause of heavy bleeding is iatrogenic, meaning it is caused by medical treatment.
Certain medications and devices can directly or indirectly increase menstrual flow.
Intrauterine Devices (IUDs)
It is crucial to differentiate between the two main types of IUDs:
- Copper IUD (Non-Hormonal): The copper IUD (e.g., Paragard) is a highly effective, hormone-free contraceptive. However, its primary side effect is a known increase in menstrual bleeding and cramping. The copper creates a local inflammatory reaction in the uterus, which is thought to be the mechanism for both contraception and heavier, more painful periods. This effect is usually most pronounced in the first 3-6 months after insertion but can persist for some users.
- Hormonal IUDs: In stark contrast, hormonal IUDs (e.g., Mirena, Kyleena, Liletta) release a small amount of a progestin hormone directly into the uterus. This hormone thins the uterine lining, making them a first-line treatment for heavy periods. Most users experience significantly lighter periods, and many stop having periods altogether.
Blood Thinners (Anticoagulants and Antiplatelets)
This link is straightforward. Medications designed to prevent blood clots will naturally increase all types of bleeding, including menstrual bleeding. This includes:
- Anticoagulants: Warfarin (Coumadin), heparin, and newer direct oral anticoagulants (DOACs) like rivaroxaban (Xarelto), apixaban (Eliquis), and dabigatran (Pradaxa).
- Antiplatelet drugs: Aspirin and clopidogrel (Plavix).
If you are taking any of these medications for a condition like atrial fibrillation, deep vein thrombosis, or heart disease, you may experience heavier periods as a side effect.
It’s important not to stop these medications but to discuss the heavy bleeding with your doctor, who can manage the issue.
Other Medications
While less common, other classes of drugs have been anecdotally or occasionally linked to changes in menstrual flow. These can include certain antipsychotics, antidepressants, and corticosteroids.
Chemotherapy drugs used to treat cancer can also affect ovarian function and the uterine lining, leading to abnormal bleeding.
Diagnosis & When to Seek Help
Recognizing that your periods are a problem is the first step. The next is seeking a professional diagnosis.
This process can feel intimidating, but it is a systematic way for your doctor to identify the root cause of your bleeding and find the right solution for you.
How Do I Know When to See a Doctor for Heavy Periods?
The single most important reason to see a doctor is this: If your period is negatively impacting your quality of life, it’s time to talk to a healthcare provider. You do not have to “just live with” debilitating periods.
Use this checklist. Make an appointment if you regularly experience:
- Bleeding that requires changing pads/tampons every hour.
- Periods lasting longer than 7 days.
- Passing clots larger than a quarter.
- Symptoms of anemia like extreme fatigue, dizziness, or shortness of breath.
- Period pain or bleeding that causes you to miss work, school, or social activities.
Additionally, there are certain “red flag” symptoms that require more urgent medical attention:
- Sudden, severe pelvic pain.
- Bleeding after you have gone through menopause.
- Unusually heavy bleeding during pregnancy.
What Can I Expect During a Doctor’s Visit?
A thorough evaluation for heavy periods is a multi-step process. Being prepared for what to expect can help reduce anxiety and ensure you get the most out of your appointment.
- Medical History & Symptom Tracking
This is the most important part of the evaluation. Your doctor will ask detailed questions about your menstrual and medical history. To prepare, it’s incredibly helpful to track your cycles for 1-2 months beforehand. Note the start and end dates, estimate your flow (e.g., number of pads/tampons used per day, noting heavy vs. light days), the size of any clots, and any associated symptoms like pain or fatigue. Be ready to discuss your personal and family medical history, all medications you take (including supplements), and your contraceptive history. - Physical Exam
A physical exam will likely include checking your vital signs and a general examination. A pelvic exam is also standard. During the pelvic exam, your doctor will visually inspect the cervix and manually feel the uterus and ovaries to check for any obvious abnormalities in size, shape, or tenderness that might suggest fibroids or adenomyosis. A Pap test may also be performed if you are due for one. - Blood Tests
Blood work is essential for uncovering underlying issues. Common tests include:- Complete Blood Count (CBC): This test is crucial to check for iron-deficiency anemia by measuring your hemoglobin and hematocrit levels.
- Thyroid-Stimulating Hormone (TSH): This screens for thyroid dysfunction, a common and reversible cause of heavy bleeding.
- Coagulation Studies: If a bleeding disorder is suspected, tests like a prothrombin time (PT), partial thromboplastin time (PTT), and von Willebrand factor antigen will be ordered.
- Pelvic Ultrasound
A pelvic ultrasound is a non-invasive imaging test that uses sound waves to create a picture of your pelvic organs. It is the primary tool for identifying structural causes of heavy bleeding. A transvaginal ultrasound, where a small probe is placed in the vagina, provides the clearest images of the uterus, uterine lining, and ovaries, allowing the doctor to detect fibroids, polyps, adenomyosis, and measure the thickness of the endometrium. - Further Procedures (If Needed)
If the initial evaluation is inconclusive or if there’s a suspicion of an abnormality inside the uterine cavity, your doctor may recommend more advanced tests:- Hysteroscopy: A thin, lighted tube with a camera (hysteroscope) is inserted through the cervix into the uterus. This allows the doctor to directly visualize the inside of the uterine cavity to identify and sometimes even remove polyps or small fibroids at the same time.
- Endometrial Biopsy: A small sample of the uterine lining is removed and sent to a lab to be examined under a microscope. This is done to rule out endometrial hyperplasia or cancer, especially in women over 45 or those with specific risk factors.
Overview of Management and Treatment Options
The good news is that heavy periods are highly treatable. The best treatment for you will depend on the underlying cause, the severity of your bleeding, your overall health, and your future reproductive plans.
The goal is to reduce bleeding, improve quality of life, and correct any associated problems like anemia.
How Are Heavy Periods Treated?
Treatment options range from simple at-home care and medications to minimally invasive procedures and surgery.
Medical Treatments (Non-Hormonal & Hormonal)
Medications are often the first line of defense, especially when no major structural abnormality is found.
- Non-Hormonal Medications:
- NSAIDs (Nonsteroidal Anti-inflammatory Drugs): Over-the-counter medications like ibuprofen (Advil, Motrin) or naproxen sodium (Aleve), when taken on a schedule starting just before or at the onset of your period, can reduce menstrual blood flow by 20-50%. They work by lowering levels of prostaglandins, hormone-like substances involved in pain and inflammation.
- Tranexamic Acid (Lysteda): This is a prescription non-hormonal medication taken only during the days of heavy bleeding. It works by helping the blood in the uterus to clot more effectively, preventing the breakdown of clots that normally occurs. It can reduce bleeding by up to 60% and is a great option for women who want to avoid hormones.
- Hormonal Treatments:
- Hormonal Contraceptives: Combination birth control pills, the patch, and the vaginal ring are very effective at regulating cycles and reducing flow by preventing ovulation and thinning the uterine lining.
- Hormonal IUDs: As mentioned earlier, progestin-releasing IUDs like Mirena are a highly effective, long-term treatment, reducing menstrual flow by over 90% in many women.
- Progestin-Only Therapies: Progestin, the synthetic form of progesterone, can be given as a pill (e.g., norethindrone) or an injection (Depo-Provera). It counteracts the effects of estrogen, thins the uterine lining, and can significantly lighten or even stop periods.
Procedural and Surgical Options
When medications are not effective or a structural problem like large fibroids is the cause, procedures may be recommended.
- Endometrial Ablation: This is a minimally invasive procedure that destroys the lining of the uterus. It is very effective at reducing or eliminating menstrual bleeding. However, it is only an option for women who have completed childbearing, as pregnancy after ablation is dangerous.
- Uterine Artery Embolization (UAE): A procedure specifically for treating fibroids. A radiologist blocks the blood vessels that supply the fibroids, causing them to shrink and die.
- Myomectomy: The surgical removal of fibroids while leaving the uterus intact. This is the preferred option for women with fibroids who wish to preserve their fertility.
- Hysterectomy: The surgical removal of the uterus. This is the only 100% definitive cure for heavy menstrual bleeding. It is a major surgery and is typically reserved as a last resort after other treatments have failed or are not appropriate.
Lifestyle and At-Home Management
While lifestyle changes alone may not solve severe menorrhagia, they can support medical treatment and help manage symptoms.
- Iron-Rich Diet: If you have heavy periods, you are at high risk for iron-deficiency anemia. It is crucial to consume iron-rich foods like red meat, poultry, fish, lentils, beans, spinach, and fortified cereals. Your doctor will likely recommend an iron supplement as well.
- Maintain a Healthy Weight: Excess body fat can produce estrogen, contributing to hormonal imbalances. Maintaining a healthy weight through diet and exercise can help regulate cycles.
- Stress Management: Chronic stress can disrupt the hormonal axis that controls the menstrual cycle. Practices like yoga, meditation, and regular exercise can be beneficial.
Associated Risks & Complications
Ignoring heavy periods can lead to significant health consequences that extend beyond the monthly inconvenience.
The most direct and common complication is a direct result of chronic blood loss.
What Are the Health Risks of Untreated Heavy Periods?
Iron-Deficiency Anemia
This is, by far, the most significant health risk of untreated menorrhagia. Your body uses iron to make hemoglobin, a protein in red blood cells that carries oxygen from your lungs to the rest of your body.
When you lose more blood each month than your body can replace, your iron stores become depleted. Without enough iron, your body cannot produce enough healthy red blood cells, leading to iron-deficiency anemia.
The symptoms of anemia are not just “feeling a little tired”. They can be debilitating and include:
- Extreme fatigue and lack of energy that is not relieved by rest.
- Weakness and decreased ability to exercise.
- Pale skin, especially noticeable on the face, nails, and inner eyelids.
- Shortness of breath, even with minimal exertion.
- Headaches and dizziness or lightheadedness.
- Cold hands and feet.
- Brittle nails or a craving for non-food items like ice (pica).
Severe, long-term anemia can also put a strain on your heart, as it has to work harder to pump oxygen-rich blood through your body.
Severe Pain and Discomfort
Heavy bleeding is often accompanied by significant menstrual pain (dysmenorrhea). This is particularly true when the uterus has to pass large blood clots, which requires strong, painful uterine contractions.
Conditions like adenomyosis and fibroids can also cause a constant, dull pelvic ache or pressure in addition to the acute cramping during the period.
Impact on Quality of Life
The “experience”, component of living with heavy periods cannot be overstated. The constant fear of bleeding through clothing can lead to significant anxiety and social isolation.
Many individuals report having to miss work or school, avoiding travel, shying away from physical activity, and experiencing a negative impact on their intimate relationships.
The emotional and psychological toll of managing a condition that is both physically draining and socially stressful is a major, though often hidden, complication.
Frequently Asked Questions About Heavy Periods
Here are direct answers to some of the most common questions people have about heavy menstrual bleeding.
Q1: Can stress cause heavy periods?
Yes, indirectly. High levels of chronic stress can disrupt the hormonal signals from the brain that regulate your menstrual cycle. This can lead to anovulation (not ovulating), which in turn can cause a missed period followed by a very heavy one due to the buildup of the uterine lining.
Q2: Why am I suddenly having heavy periods with large clots?
A sudden change could be due to several factors, including a new hormonal imbalance (common in perimenopause), the development of a fibroid or polyp, or a side effect of a new medication. Passing large clots often means bleeding is rapid, and the body’s anticoagulants can’t keep up.
Q3: Is it normal for periods to get heavier in your 30s or 40s (perimenopause)?
It is very common. During perimenopause, the transition to menopause, ovulation becomes more erratic. This leads to hormonal fluctuations, particularly anovulatory cycles with unopposed estrogen, which can cause periods to become heavier and more irregular before they eventually stop.
Q4: Can I get pregnant if I have heavy periods?
It depends on the cause. If heavy periods are due to anovulatory cycles, it can be difficult to conceive. However, if they are caused by something structural like fibroids, fertility may not be affected unless the fibroid is blocking the fallopian tubes or distorting the uterine cavity.
Q5: What’s the difference between a heavy period and a hemorrhage?
A heavy period (menorrhagia) is excessive but cyclical bleeding. A hemorrhage is acute, severe, and potentially life-threatening bleeding. If you are soaking through a pad or tampon in less than an hour, feel dizzy or faint, or have a racing heart, seek immediate medical attention.
Q6: Can diet changes help reduce heavy menstrual bleeding?
While diet alone is unlikely to cure severe menorrhagia, an anti-inflammatory diet rich in fruits, vegetables, and omega-3s may help. Most importantly, an iron-rich diet is crucial to combat anemia. Some studies suggest vitamin A and C may also play a role in managing bleeding.
Q7: How quickly can treatments for heavy periods work?
It varies. Medications like tranexamic acid and NSAIDs can provide relief within the first cycle of use. Hormonal treatments like birth control pills may take 2-3 cycles to show their full effect. A hormonal IUD can take 3-6 months to significantly reduce bleeding.
Q8: Are heavy periods a sign of infertility?
Not necessarily, but they can be related. Conditions that cause heavy periods, such as PCOS, anovulation, and large uterine fibroids, can also make it more difficult to become pregnant. A proper diagnosis is key to understanding any potential impact on your fertility.
Conclusion
Heavy periods are far more than a monthly nuisance, they are a legitimate medical condition with a wide range of identifiable causes and effective treatments.
As we’ve explored, the reasons for excessive menstrual bleeding are diverse, stemming from complex hormonal imbalances, structural issues within the uterus like fibroids and adenomyosis, and other underlying medical conditions.
The key takeaways are clear:
- Heavy menstrual bleeding is common, but it is not normal to suffer from it.
- The most frequent causes fall into three main categories: hormonal dysregulation, uterine abnormalities, and systemic health problems or medications.
- An accurate diagnosis, achieved through a careful medical history, physical exam, blood tests, and imaging, is the essential first step toward finding relief.
- Untreated heavy periods can lead to significant health issues, most notably iron-deficiency anemia, and can severely diminish your quality of life.
You do not have to “just live with” heavy periods. If your menstrual cycle is disrupting your life, schedule a conversation with your healthcare provider to discuss your symptoms and explore your options.
Empowering yourself with knowledge is the first step. The second is taking action. We hope this guide has provided you with the clarity and confidence to begin that journey.
Have you experienced heavy periods? Share your story or questions in the comments below to support others in our community.
Reference
[1] Heavy menstrual bleeding – Symptoms and causes – Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/menorrhagia/symptoms-causes/syc-20352829
[2] Fibroid Studies | Women’s Health Clinical Research Center
https://whcrc.ucsf.edu/fibroid-studies
[3] Abnormal Uterine Bleeding in Premenopausal Women – AAFP
https://www.aafp.org/pubs/afp/issues/2019/0401/p435.html
[4] Heavy menstrual bleeding – Symptoms and causes – Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/menorrhagia/symptoms-causes/syc-20352829
[5] The relationship between heavy menstrual bleeding, iron deficiency …
https://www.sciencedirect.com/science/article/abs/pii/S0002937823000248
[6] Treatment of Heavy Menstrual Bleeding in Women With Uterine …
https://clinicaltrials.gov/study/NCT03317795
[7] Heavy periods: Can folic acid help? – Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/menorrhagia/expert-answers/heavy-periods/faq-20058365
[8] From menarche to menopause, heavy menstrual bleeding is the …
https://www.sciencedirect.com/science/article/pii/S0015028222004770
[9] Treatment of Anemia Owing to Increased Menstrual Blood Loss

