Learning how to boost your immune system is not about a single magic pill, but about adopting a holistic set of lifestyle and dietary habits that support its complex functions.
These evidence-based strategies help create balance and resilience, fortifying your body’s natural defenses against pathogens.
In a world where health is paramount, understanding these mechanisms is more critical than ever.
According to the Centers for Disease Control and Prevention (CDC), people with weakened immune systems have a significantly higher risk of severe outcomes from common respiratory viruses, underscoring the importance of a well-functioning immune response.
This article delves deep into the science of immunity, moving beyond surface-level advice. We will explore ten proven methods for strengthening your defenses, explaining the biological mechanisms that make them effective.
You will learn about the specific foods and nutrients that fuel your immune cells, the critical role of sleep and stress management, and which supplements are backed by credible research.
We will also debunk common myths and provide a practical, actionable plan to help you integrate these changes into your daily life.
Read on to discover how you can build a stronger, more responsive immune defense system.
In This Article
What Is the Immune System and Why Is Balance Key?
Before we explore how to strengthen the immune system, it’s crucial to understand what it is and how it works.
The immune system is not a single organ but a vast, intricate network of cells, tissues, and organs that work in concert to defend the body against harmful invaders like bacteria, viruses, fungi, and toxins.
The concept of “boosting” can be misleading, the true goal is not to supercharge it, but to achieve harmony and balance.
An underactive immune system leaves you vulnerable to infection, while an overactive one can lead to autoimmune diseases and chronic inflammation.
The Two Arms of Defense: Innate vs. Adaptive Immunity
Think of your immune system as a highly sophisticated military with two main branches.
Each plays a distinct but coordinated role in protecting your health.
- Innate Immunity: The First Responders. This is your body’s non-specific, rapid-response system. It includes physical barriers like the skin and mucous membranes, which prevent germs from entering. If a pathogen breaches these barriers, innate immune cells like phagocytes (which means “eating cells”) and Natural Killer (NK) cells are deployed to engulf and destroy the invaders immediately. This response is fast but doesn’t create lasting memory of the pathogen.
- Adaptive Immunity: The Specialized Army. This is a more advanced, targeted system that develops over your lifetime. When the innate system can’t contain an infection, the adaptive system kicks in. It involves highly specialized cells called lymphocytes—T-cells and B-cells. This response is slower to activate but is incredibly precise and creates an “immunological memory”. This memory allows your body to recognize and mount a much faster and stronger attack if it encounters the same pathogen in the future, which is the principle behind vaccination.
Key Players: The Cells of Your Immune Army
To appreciate how lifestyle choices impact immunity, it helps to know the key players:
- T-cells: These are the “soldiers” of the adaptive system. Helper T-cells coordinate the immune response, while Cytotoxic T-cells directly hunt down and destroy infected cells.
- B-cells: These act as the “intelligence officers”. When activated, they produce antibodies—Y-shaped proteins that lock onto specific invaders, marking them for destruction.
- Natural Killer (NK) Cells: Part of the innate system, these are vigilant “sentinels” that can recognize and kill virus-infected cells and some tumor cells without prior sensitization.
- Phagocytes (e.g., Macrophages): These are the “clean-up crew” of the innate system, engulfing and digesting cellular debris, pathogens, and cancer cells. They also play a key role in activating the adaptive immune system.
Why “Boosting” Is Really About Achieving Harmony
The term “boost” implies a simple increase in power, but the immune system is a delicate balancing act. Pushing it too hard can be detrimental.
For example, an overactive immune response is the root cause of allergies, where the body attacks harmless substances like pollen, and autoimmune diseases like rheumatoid arthritis or lupus, where it mistakenly attacks its own healthy tissues.
Chronic, low-grade inflammation—a state of constant immune activation—is linked to numerous modern diseases, including heart disease, diabetes, and cancer.
Therefore, the strategies discussed in this article are not about indiscriminately “boosting” the number of immune cells. Instead, they are about providing your body with the resources it needs to maintain a balanced, efficient, and appropriately responsive immune system—one that fights off invaders effectively without causing collateral damage.
1. How Can You Boost Your Immune System with Food?
Nutrition is the cornerstone of a healthy immune system. The cells of your immune army require a constant supply of energy and specific micronutrients to function optimally.
A diet lacking in these essential components can impair the production and activity of immune cells and antibodies.
The Foundation: A Whole-Foods, Plant-Rich Diet
The most powerful way to support your immune system through diet is to focus on whole, unprocessed foods. Diets rich in a variety of fruits, vegetables, whole grains, and legumes provide a wide array of vitamins, minerals, antioxidants, and fiber.
These compounds work synergistically to protect your body from oxidative stress—damage caused by unstable molecules called free radicals—and to quell unnecessary inflammation, allowing your immune system to focus on real threats.
Key Immune-Supporting Nutrients and Where to Find Them
While a balanced diet is paramount, certain nutrients play a particularly vital role in immune function.
As detailed in a comprehensive 2022 review in the journal Nutrients, both micronutrients and macronutrients are critical for modulating immune responses. Here are some of the most important ones:
- Vitamin C: A powerful antioxidant that supports various cellular functions of both the innate and adaptive immune systems. It encourages the production of white blood cells and helps them function more effectively.
- Sources: Citrus fruits (oranges, grapefruit), bell peppers, strawberries, broccoli, kiwi.
- Vitamin D: Acts more like a hormone and is a potent immune modulator. It helps regulate both pro-inflammatory and anti-inflammatory responses, and its receptors are found on most immune cells.
- Sources: Fatty fish (salmon, mackerel), fortified milk and cereals, and sunlight exposure.
- Zinc: This mineral is crucial for the normal development and function of immune cells. Even a mild zinc deficiency can impair macrophage and T-cell function.
- Sources: Beans, nuts, seeds, whole grains, oysters, lean meats.
- Vitamin A: Essential for maintaining the integrity of mucosal barriers in your respiratory tract and gut, which are your first line of defense. It also plays a role in the function of T-cells and B-cells.
- Sources: Carrots, sweet potatoes, spinach, kale (as beta-carotene).
- Selenium: An important antioxidant that helps lower oxidative stress in the body, which in turn reduces inflammation and enhances immunity. It can strengthen the response to vaccination.
- Sources: Brazil nuts (just one or two a day is enough), seafood, whole grains, eggs.
This is supported by extensive research, such as a study published in PubMed Central, which highlights how deficiencies in these micronutrients can alter immune responses and increase susceptibility to infection.
The Anti-Inflammatory Power of the Mediterranean Diet
One dietary pattern that consistently demonstrates immune-supporting benefits is the Mediterranean diet.
Characterized by a high intake of fruits, vegetables, nuts, legumes, whole grains, fish, and olive oil, this diet is rich in anti-inflammatory compounds.
Research, including a 2024 study on the impact of the Mediterranean diet on immune function in older adults, shows that greater adherence to this diet is associated with lower levels of inflammatory markers like C-reactive protein (CRP) and IL-6, and a healthier gut microbiome, all of which contribute to a more balanced immune system.
2. Why Is Quality Sleep Crucial for a Strong Immune Response?
Sleep is not a passive state of rest, it is a critical period of restoration and reorganization for the entire body, especially the immune system.
A robust body of scientific evidence shows a powerful, bidirectional link between sleep and immunity: a healthy immune system promotes good sleep, and adequate sleep fortifies the immune system.
The Science of Sleep and Immunity: Cytokines and T-Cells
During deep, restorative sleep, your immune system releases proteins called cytokines.
Some of these cytokines are protective and play a crucial role in promoting inflammation when you have an infection or injury.
When you don’t get enough sleep, the production of these protective cytokines and infection-fighting antibodies is reduced.
Furthermore, groundbreaking research has shown that sleep enhances the effectiveness of T-cells. A 2019 study found that a good night’s sleep improves the potential of T-cells to adhere to and destroy cells infected with a virus.
The stress hormones adrenaline and noradrenaline, which are lower during sleep, can inhibit this “stickiness”.
As highlighted in a review on sleep deprivation and immune-related disease risk, chronic sleep loss can lead to a state of chronic inflammation and impair the adaptive immune response, making you more vulnerable to infections and reducing the efficacy of vaccines.
How Much Sleep Do You Really Need?
The National Sleep Foundation recommends 7 to 9 hours of quality sleep per night for most adults. Consistently falling short of this target—a condition known as chronic sleep deprivation—can have significant consequences.
Studies show that people who don’t get enough quality sleep are more likely to get sick after being exposed to a virus, such as the common cold. The recovery from illness may also take longer.
Practical Tips for Improving Your Sleep Hygiene
Improving your sleep isn’t just about quantity, it’s about quality. Here are some actionable steps to improve your sleep hygiene:
- Maintain a Consistent Schedule: Go to bed and wake up at the same time every day, even on weekends. This helps regulate your body’s internal clock, or circadian rhythm.
- Create a Restful Environment: Ensure your bedroom is dark, quiet, and cool. Use blackout curtains, earplugs, or a white noise machine if needed.
- Limit Blue Light Exposure: The blue light emitted by phones, tablets, and computers can suppress melatonin production, a hormone that signals your body it’s time to sleep. Avoid screens for at least an hour before bed.
- Develop a Relaxing Bedtime Routine: Engage in calming activities like reading a book, taking a warm bath, listening to soft music, or practicing mindfulness meditation to signal to your body that it’s time to wind down.
- Avoid Stimulants: Refrain from consuming caffeine and nicotine late in the day, as their stimulating effects can take hours to wear off.
3. What Type of Exercise Best Supports Immunity?
Regular physical activity is a pillar of healthy living, and its benefits extend deeply into the immune system.
Like a healthy diet, exercise contributes to general good health and therefore to a well-functioning immune system.
It improves cardiovascular health, helps control body weight, and protects against a variety of diseases.
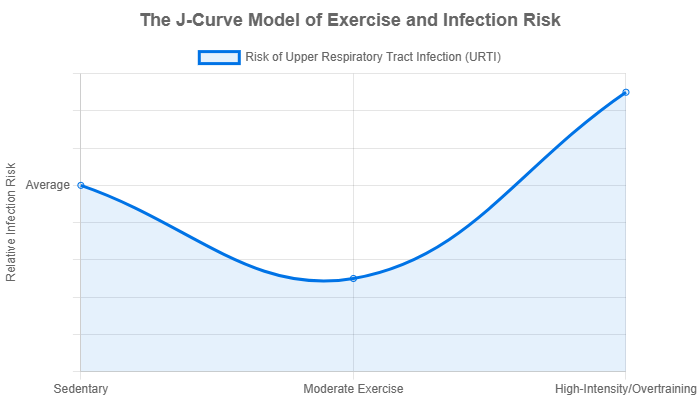
The “J-Curve” Explained: Finding Your Sweet Spot
The relationship between exercise and infection risk is often described by a model known as the “J-Curve”.
This concept, detailed in a landmark review in the Journal of Sport and Health Science, illustrates the following:
- Sedentary individuals have an average risk of infection.
- Those who engage in moderate, regular exercise see a significant reduction in their risk of infection. This is the bottom of the “J”.
- Conversely, individuals who engage in excessive, high-intensity exercise without adequate recovery (overtraining) see their infection risk rise above that of sedentary people. This forms the hook of the “J”.
This shows that the key is consistency and moderation. The goal is not to push your body to its absolute limit every day, but to engage in regular, moderately intense activity.
How Moderate Exercise Enhances Immunosurveillance
Regular, moderate exercise—such as a 30-45 minute brisk walk, a bike ride, or a swim—has several direct benefits for immunity.
During and after exercise, there is a temporary surge in the circulation of key immune cells, including NK cells and T-cells. This process is known as immunosurveillance.
By mobilizing these cells from their “barracks” (like the spleen and lymph nodes) into the bloodstream and peripheral tissues, exercise increases the body’s ability to detect and eliminate pathogens and cancerous cells before they can establish a foothold.
Over time, this regular patrol helps maintain a more vigilant and efficient immune system.
The Dangers of Overtraining
While moderate exercise is beneficial, too much of a good thing can be harmful. Prolonged, high-intensity training without sufficient rest can lead to a state of overtraining.
This condition is characterized by increased levels of stress hormones like cortisol and adrenaline, which have immunosuppressive effects.
It can lead to a temporary window of decreased immunity following a grueling workout, making athletes more susceptible to infections. This is why elite athletes often have carefully managed training and recovery schedules to mitigate this risk.
4. How Does Chronic Stress Weaken Your Immune System?
The mind and body are inextricably linked, and psychological stress can have profound and measurable effects on your physical health, particularly your immune system.
While short-term stress can momentarily enhance immune function (the “fight or flight” response), chronic, unrelenting stress has a decidedly negative impact.
The Cortisol Connection: Stress Hormones and Immunity
When you are under chronic stress, your body produces a continuous stream of the stress hormone cortisol. In the short term, cortisol is anti-inflammatory and helps contain the immune response.
However, when cortisol levels are persistently high, the immune system becomes desensitized to its effects. This is known as cortisol resistance.
This leads to a dysfunctional state where the body loses its ability to regulate the inflammatory response. As a result, levels of pro-inflammatory cytokines can rise, contributing to the chronic, low-grade inflammation associated with many diseases.
Furthermore, as research published in a 2024 review on the immunology of stress confirms, elevated cortisol can suppress the activity and production of lymphocytes, the very cells needed to fight off infection.
This dual effect—promoting inflammation while suppressing infection-fighting cells—is why chronic stress leaves you more vulnerable to everything from the common cold to more serious conditions.
Science-Backed Stress Reduction Techniques
Managing stress is a critical component of any plan for a healthy immune system. Here are several techniques with proven benefits:
- Mindfulness Meditation: This practice involves focusing on your breath and bringing your attention to the present moment without judgment. Studies have shown that regular mindfulness practice can reduce markers of inflammation and increase activity in brain regions associated with positive immune responses.
- Deep Breathing Exercises: Simple techniques like diaphragmatic breathing (belly breathing) can activate the parasympathetic nervous system, your body’s “rest and digest” system, which counteracts the “fight or flight” response and lowers cortisol levels.
- Yoga and Tai Chi: These mind-body practices combine physical postures, breathing exercises, and meditation. They are effective at reducing stress, improving mood, and have been shown to modulate immune system parameters favorably.
- Spending Time in Nature: Sometimes called “forest bathing”, spending time in natural environments has been shown to lower cortisol, reduce blood pressure, and boost the activity of NK cells.
5. Which Vitamins and Supplements Actually Support Immunity?
While a food-first approach is always best, strategic supplementation can help fill nutritional gaps and provide extra support, especially for nutrients that are difficult to obtain in sufficient quantities from diet alone.
However, it’s crucial to navigate the supplement aisle with a critical, evidence-based perspective.
Vitamin D: The Sunshine Vitamin’s Critical Role
Vitamin D stands out as one of the most important nutrients for immune function. As detailed in a comprehensive 2024 review on its anti-inflammatory roles, Vitamin D acts as a powerful immune system modulator.
Its active form, calcitriol, can bind to receptors on virtually all immune cells, including T-cells and B-cells, helping to regulate their function.
It helps to prevent an overzealous inflammatory response while ensuring the immune system can mount an effective attack against pathogens.
Vitamin D deficiency is widespread globally, particularly in regions with limited sun exposure.
Since it’s challenging to get enough from food alone, many experts recommend supplementation, especially during the winter months.
A blood test can determine your levels and help a healthcare provider recommend an appropriate dose.
Vitamin C & Zinc: Do They Work for Colds?
Vitamin C and zinc are perhaps the most famous immune-support supplements. The scientific consensus is nuanced:
- Vitamin C: For the general population, taking Vitamin C supplements daily does not appear to prevent colds. However, research suggests that taking a therapeutic dose (e.g., 1-2 grams) at the very onset of cold symptoms may shorten the duration of the cold by about a day and reduce the severity of symptoms.
- Zinc: Similar to Vitamin C, zinc appears to be most effective when taken within 24 hours of the first sign of a cold. Zinc lozenges, in particular, have been shown in some studies to significantly reduce the duration of the common cold, possibly by preventing the rhinovirus from replicating in the nasal passages.
The key takeaway is that these supplements are not a preventative shield but can be a useful tool to have on hand to use at the first sign of illness.
A Word of Caution: More Is Not Always Better
It is essential to approach supplementation with caution. The concept of “boosting” immunity with megadoses of vitamins can be ineffective and sometimes harmful. For example, excessively high doses of zinc can interfere with copper absorption and may even suppress immunity. Always consult with a healthcare professional before starting any new supplement regimen to ensure it is safe and appropriate for your individual needs. Supplements should complement, not replace, a healthy diet and lifestyle.
6. How Does a Healthy Gut Microbiome Boost Immunity?
The gastrointestinal tract is a major site of immune activity. In fact, an estimated 70-80% of your body’s immune cells are located in the gut.
This makes the health of your gut and its resident community of microorganisms—the gut microbiome—a critical factor in the overall function of your immune system.
Your Gut: The Immune System’s Headquarters
Your gut microbiome consists of trillions of bacteria, viruses, and fungi that live in your digestive tract.
This complex ecosystem plays a fundamental role in “training” your immune system from birth. It helps immune cells learn to distinguish between friendly bacteria and harmful invaders.
A diverse and balanced microbiome promotes a healthy gut lining, which acts as a crucial barrier preventing pathogens and toxins from entering the bloodstream.
When this barrier is compromised (a condition sometimes called “leaky gut“), it can trigger widespread inflammation and immune dysregulation.
The Power of Probiotics and Prebiotics
Nurturing a healthy gut microbiome involves a two-pronged approach using probiotics and prebiotics.
- Probiotics: These are live, beneficial bacteria that, when consumed in adequate amounts, can confer a health benefit. They help reinforce the gut barrier, compete with pathogenic bacteria for resources, and directly modulate the activity of immune cells. As a 2011 review on probiotics and immune health explains, certain probiotic strains can stimulate regulatory T-cells, which help to suppress excessive inflammation.
- Prebiotics: These are types of dietary fiber that humans cannot digest but serve as food for beneficial gut bacteria. By feeding the good microbes, prebiotics help them thrive and produce beneficial compounds like short-chain fatty acids (SCFAs). SCFAs, such as butyrate, are a primary energy source for cells lining the colon and have powerful anti-inflammatory effects throughout the body.
Foods to Nurture Your Gut
Incorporating a variety of gut-friendly foods is a delicious way to support your microbiome and, by extension, your immune system.
- Probiotic Sources: Fermented foods like yogurt (with live active cultures), kefir, sauerkraut, kimchi, miso, and kombucha.
- Prebiotic Sources: High-fiber foods like garlic, onions, leeks, asparagus, bananas, oats, barley, and apples. The key is dietary diversity—eating a wide range of plant foods helps to cultivate a more diverse and resilient microbiome.
7. Can Drinking More Water Really Help Your Immune System?
While drinking water won’t magically ward off a virus, proper hydration is a fundamental and often overlooked aspect of supporting your immune system’s daily operations.
Hydration’s Role in Lymphatic Function
One of the most important roles of water in immunity is its contribution to lymph. Lymph is a fluid that circulates throughout the lymphatic system, a network of tissues and organs that helps rid the body of toxins and waste.
Crucially, lymph is the vehicle that transports infection-fighting immune cells (like lymphocytes) throughout the body.
When you are dehydrated, the movement of lymph can slow down, potentially impairing your immune system’s ability to respond to threats efficiently.
Dehydration and Its Impact on Natural Defenses
Dehydration can also affect your body’s first lines of defense. Your mucous membranes in the nasal passages and throat are designed to trap pathogens.
When you are dehydrated, these membranes can become dry, compromising their effectiveness as a physical barrier. Staying hydrated helps keep these surfaces moist and functioning properly.
While there’s no need to overdo it, aiming for around 8 glasses (or 2 liters) of water per day is a good general guideline, with needs increasing with exercise or in hot climates.
8. How Does Alcohol Consumption Affect Your Immune Function?
While moderate alcohol consumption is a feature of some healthy lifestyle patterns, excessive intake can significantly disrupt and weaken immune responses, both in the short and long term.
The Short-Term and Long-Term Effects of Alcohol
Even a single episode of binge drinking can temporarily alter the immune system. It can reduce the number and function of all three major types of lymphocytes—T-cells, B-cells, and NK cells.
Over the long term, chronic heavy alcohol use has more profound consequences. It can damage the epithelial cells lining the gut, increasing gut permeability and allowing microbes to pass into the bloodstream, which triggers liver inflammation.
It also impairs the function of immune cells in the lungs, increasing susceptibility to respiratory infections like pneumonia.
Moderation Is Key
To support immune health, it’s best to limit alcohol intake. The Dietary Guidelines for Americans define moderate consumption as up to one drink per day for women and up to two drinks per day for men.
For your immune system, less is always better. If you don’t drink, there is no health reason to start.
9. What Are the Specific Impacts of Smoking on Immunity?
There is no ambiguity in the scientific community: smoking is devastating to the immune system.
It harms nearly every organ in the body and introduces a cocktail of thousands of chemicals that disrupt immune balance.
Damaging the Body’s First Lines of Defense
The chemicals in cigarette smoke directly damage the structures that protect you from respiratory infections.
For example, smoking paralyzes and destroys the cilia, the tiny hair-like structures that line your airways and are responsible for sweeping out mucus, debris, and pathogens.
This makes smokers far more vulnerable to infections like bronchitis and pneumonia.
A State of Imbalance
Smoking creates a state of chronic inflammation while simultaneously suppressing the adaptive immune response.
It compromises the function of key immune cells and is a major risk factor for developing autoimmune diseases like rheumatoid arthritis.
Quitting smoking is one of the single most powerful steps you can take to allow your immune system to recover and function properly.
10. Why Is Maintaining a Healthy Weight Important for Immunity?
Maintaining a healthy body weight through a balanced diet and regular exercise is crucial for immune function.
Excess body weight, particularly in the form of visceral fat (fat around the organs), is not metabolically inert, it acts like an endocrine organ itself.
Adipose Tissue, Inflammation, and Immune Response
Excess adipose tissue, especially visceral fat, actively produces and releases pro-inflammatory cytokines. This creates a state of chronic, low-grade inflammation throughout the body.
This constant inflammatory background noise can impair the immune system’s ability to respond effectively to acute threats like infections.
It keeps the system perpetually distracted and can lead to dysregulation of immune cell function, including that of T-cells and NK cells.
The Link to Improved Vaccine Efficacy
The state of chronic inflammation associated with obesity can also impact the effectiveness of vaccinations.
Several studies have shown that individuals with obesity may have a blunted or less durable antibody response to vaccines, including the flu shot.
By maintaining a healthy weight, you help to reduce background inflammation, allowing your immune system to mount a more robust and effective response when it truly matters.
How Can I Create a Personal Immune Support Plan?
Understanding the science is the first step, applying it consistently is what creates lasting change.
Building a resilient immune system is a marathon, not a sprint.
The key is to create sustainable habits rather than attempting a complete overhaul overnight.
A Step-by-Step Approach to Building Healthy Habits
Trying to implement all ten strategies at once can be overwhelming and lead to burnout. A more effective approach is to focus on small, incremental changes.
Pick one or two areas from the table below that feel most manageable to you. Work on them for a week or two until they feel like a natural part of your routine. Then, move on to another area.
This gradual process builds momentum and makes long-term success far more likely.
Informative Table: Your Immune Support Action Plan
| Focus Area | Science-Backed Goal | Simple First Step | Advanced Step |
|---|---|---|---|
| Nutrition | Increase intake of colorful vegetables and fruits to 5+ servings/day. | Add one extra serving of a vegetable (like spinach in a smoothie or a side salad with dinner) to your day. | Aim to “eat the rainbow” by including foods of at least 3-4 different colors (e.g., red peppers, leafy greens, blueberries) each day. |
| Sleep | Achieve 7-8 hours of quality sleep per night. | Set a consistent bedtime and stick to it, even on weekends. | Create a 30-minute “wind-down” routine without screens (e.g., reading, gentle stretching, listening to calm music). |
| Exercise | Engage in 150 minutes of moderate-intensity exercise per week. | Go for a brisk 20-minute walk three times this week. | Incorporate a mix of activities you enjoy, such as cycling, swimming, or dancing, to meet the 150-minute goal. |
| Stress Management | Incorporate a daily stress-reduction practice. | Practice 5 minutes of deep belly breathing once a day. | Explore a guided meditation app or join a beginner’s yoga class. |
| Gut Health | Increase intake of prebiotic fiber and probiotic foods. | Add a prebiotic-rich food like garlic or onion to a meal, or have a small serving of plain yogurt. | Incorporate a fermented food (like kefir or kimchi) into your diet a few times a week and increase your variety of plant-based foods. |
| Hydration | Ensure adequate daily fluid intake. | Keep a reusable water bottle on your desk or with you throughout the day as a visual reminder. | Start your day with a large glass of water before coffee or tea. |
What Common Myths About Boosting Immunity Should I Ignore?
In the quest for a stronger immune system, it’s easy to fall for misinformation. Here are the facts behind some common myths.
Myth: Megadosing Vitamin C Prevents All Colds
Fact: As discussed earlier, while Vitamin C is essential for immune function, there is little evidence that taking large doses prevents the common cold for the average person.
It may help reduce the duration and severity if taken at the first sign of symptoms, but it is not an impenetrable shield. Your body can only absorb so much Vitamin C at once, and the excess is simply excreted.
Myth: “Immune-Boosting” Products Are a Magic Bullet
Fact: The immune system is a complex, interconnected network. No single pill, potion, or superfood can “boost” it in isolation.
Products that make such claims are often oversimplifying the science for marketing purposes. True immune resilience is built upon the foundation of a consistently healthy lifestyle, not a quick fix.
Myth: Getting Cold Gives You a Cold
Fact: This is a persistent old wives’ tale. Viruses, not cold temperatures, cause colds and the flu.
The reason these illnesses are more common in winter is likely because people spend more time indoors in closer contact with others, allowing viruses to spread more easily.
Additionally, some viruses may survive longer and travel farther in the cold, dry air of winter.
Frequently Asked Questions About Ways to Boost Your Immune System
How quickly can I strengthen my immune system?
While some effects, like those from a good night’s sleep, can provide short-term support, building true immune resilience is a long-term process. Consistent healthy habits practiced over weeks and months yield the most significant and lasting results in strengthening your immune system.
What are the first signs of a weak immune system?
Frequent infections (e.g., more than four colds a year for an adult), slow-healing wounds, constant fatigue, and persistent digestive issues can be signs. It’s important to consult a healthcare provider for a proper diagnosis as these symptoms can have many causes.
Does age affect immunity?
Yes. The immune response capability tends to decline with age, a process known as immunosenescence. This makes older adults more susceptible to infections and can lead to a weaker response to vaccination. However, a healthy lifestyle can help mitigate some of these age-related changes.
Can I boost my immune system for just 24 hours?
You can support your immune system in the short term by getting a full night of quality sleep, staying well-hydrated, eating a nutritious meal, and managing stress. However, lasting strength and resilience come from long-term, consistent habits, not a 24-hour fix.
Are there specific foods that are best for immunity?
Focus on a variety of colorful fruits and vegetables, lean proteins, and healthy fats. Foods rich in key nutrients like garlic, ginger, spinach, almonds, citrus fruits, and berries are all excellent choices to include in a balanced diet for immune support.
Is it okay to exercise when I have a cold?
The general rule of thumb is the “neck check.” If your symptoms are mild and all “above the neck” (runny nose, mild sore throat), light to moderate exercise like walking is usually fine. If you have symptoms “below the neck” (chest congestion, body aches) or a fever, rest is best.
Do I need to take a multivitamin?
If your diet is balanced and rich in a wide variety of whole foods, you may not need one. However, a multivitamin can act as an insurance policy to fill any potential nutritional gaps. It’s best to consult a healthcare provider to assess your individual needs.
How important is hand washing for immunity?
It is critically important. Frequent and proper hand washing is one of the most effective and simplest ways to support your immune system by preventing exposure to pathogens in the first place. It is a crucial first line of defense against invading germs.
Conclusion
A strong and balanced immune system is not built overnight with a single product or quick fix.
It is the cumulative result of your daily choices and habits. As we’ve explored, the science points to a holistic approach that encompasses a nutrient-dense diet, restorative sleep, regular moderate exercise, and effective stress management.
Each of these pillars provides your body with the essential tools it needs to maintain a vigilant, efficient, and harmonious defense system.
By understanding the mechanisms behind these strategies—from the role of Vitamin D in modulating T-cells to the importance of a diverse gut microbiome—you are empowered to make informed decisions about your health.
Every small, positive change you make contributes to your overall resilience. The journey to a stronger immune system is a commitment to self-care and a powerful investment in your long-term well-being.
Start your journey to a stronger immune system today. Choose one strategy from the action plan in this guide to implement this week. Share which one you’re starting with in the comments below!
References
- CDC: Respiratory Viruses and People with Weakened Immune Systems
- Munteanu, C., & Schwartz, B. (2022). The relationship between nutrition and the immune system. Nutrients.
- Migliaccio, S., et al. (2024). The impact of the Mediterranean diet on immune function in older adults. Journal of Translational Medicine.
- Garbarino, S., et al. (2021). Role of sleep deprivation in immune-related disease risk and outcomes. Communications Biology.
- Nieman, D. C., & Wentz, L. M. (2019). The compelling link between physical activity and the body’s defense system. Journal of Sport and Health Science.
- Alotiby, A., & Al-Ghamdi, M. (2024). Immunology of Stress: A Review Article. Cureus.
- Fenercioglu, A. K., et al. (2024). The Anti-Inflammatory Roles of Vitamin D for Improving Health. International Journal of Molecular Sciences.
- Yan, F., & Polk, D. B. (2011). Probiotics and immune health. Current Opinion in Gastroenterology.

