For decades, vitamin D has been known as the “sunshine vitamin”, essential for strong bones.
But this simple label masks its true identity. Vitamin D is not merely a vitamin, it’s a potent steroid hormone that actively commands and regulates the immune system, helping it fight infections while crucially preventing it from overreacting and attacking the body itself.
This dual role makes it one of the most critical, yet often overlooked, players in our overall health.
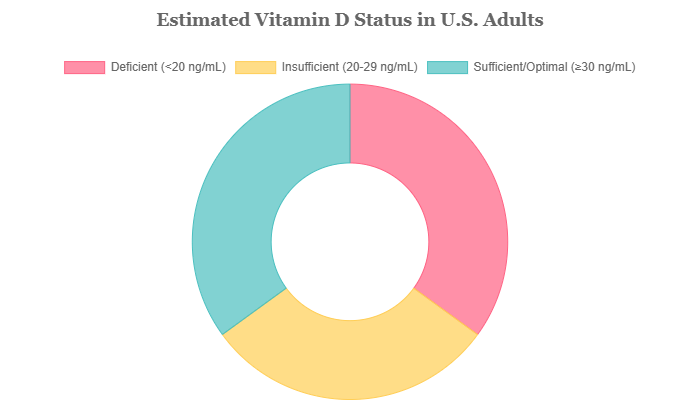
This isn’t a niche concern. An estimated 35% of adults in the United States have a vitamin D deficiency, according to data from the Centers for Disease Control and Prevention (CDC) and other health institutions.
This makes it a widespread and silent public health issue, quietly undermining the immune defenses of millions.
Many people who are deficient have no obvious symptoms, yet their bodies may be less equipped to handle immunological challenges.
In this definitive guide, we will move beyond the headlines and delve into the science.
You will learn precisely how vitamin D works at a cellular level to orchestrate your immune response, its proven role in preventing infections and its potential to reduce the risk of autoimmune diseases.
We will also provide a clear action plan to help you identify deficiency and optimize your levels through sun, food, and smart supplementation.
Let’s explore the science-backed ways this ‘sunshine vitamin’ acts as your body’s master immune regulator.
In This Article
The Core Connection: How Vitamin D Commands Your Immune System
To truly appreciate the importance of vitamin D, we must look inside the body at the molecular level.
Its influence isn’t passive, it’s an active, dynamic process of communication and control.
This section breaks down the precise mechanisms that link this hormone to your body’s defense network, moving from the cellular “docking stations” to its role in fighting off invaders and calming internal friendly fire.
How Does Vitamin D Actually “Talk” to Your Immune Cells?
The entire relationship between vitamin D and immunity hinges on a single, elegant mechanism: a specialized receptor found within our most important immune cells.
This isn’t a random association, it’s a hard-wired biological system.
The Vitamin D Receptor (VDR): The “Docking Station” in Every Immune Cell
Think of your key immune cells—the T-cells that direct the attack, the B-cells that create antibodies and the macrophages that engulf pathogens—as highly secure facilities.
To get inside and give orders, you need the right key. Nearly all of these cells are equipped with a special protein called the Vitamin D Receptor (VDR).
The VDR acts as a “docking station” or a lock. The active form of vitamin D, known as calcitriol or 1,25(OH)2D, is the key.
When you have sufficient vitamin D, it circulates in the blood, finds these immune cells and its active form binds to the VDR. This binding event initiates a cascade of actions.
The vitamin D-VDR complex travels to the cell’s nucleus—its command center—and interacts directly with its DNA.
Here, it functions as a transcription factor, turning specific genes on or off.
According to a review in the Journal of Investigative Medicine, this process can regulate the expression of hundreds of genes, many of which are directly involved in immune function.
This is the biological foundation for all of vitamin D’s profound effects on our health.
Can Vitamin D Help You Fight Off Colds, Flu and Other Infections?
One of the most exciting areas of vitamin D research is its role in bolstering our first line of defense against invading pathogens.
The evidence strongly suggests that maintaining adequate levels is a crucial strategy for staying healthy, especially during cold and flu season.
Boosting Your First Line of Defense: The Innate Immune System
Your body has two main branches of immunity. The first is the innate immune system, your non-specific, immediate defense force.
When a virus or bacterium enters your body, this system is the first to respond.
Macrophages, a type of white blood cell, are key players here, acting as sentinels and garbage collectors.
This is where vitamin D plays a direct and powerful role. When the active form of vitamin D binds to the VDR in a macrophage, it triggers a gene that produces powerful antimicrobial peptides (AMPs).
The most well-studied of these is **cathelicidin**. As described in research published in Future Microbiology, cathelicidin acts like a natural antibiotic.
It can physically puncture the protective outer membranes of a wide range of pathogens, including bacteria, viruses and fungi, causing them to burst and die.
In a state of vitamin D deficiency, your immune cells’ ability to produce this crucial weapon is significantly impaired, leaving you more vulnerable to infection.
The Evidence: Respiratory Infections and COVID-19
The link between vitamin D and respiratory health is not just theoretical. A large body of clinical evidence supports it.
A landmark meta-analysis published in the British Medical Journal (BMJ), which pooled data from 25 randomized controlled trials involving over 11.000 participants, delivered a clear verdict.
Vitamin D supplementation was found to reduce the risk of acute respiratory tract infections, such as the common cold and influenza.
Crucially, the study highlighted that the benefit was most significant for individuals who were very deficient to begin with (blood levels below 10 ng/mL).
For this group, supplementation cut the risk of respiratory infection in half. Daily or weekly supplementation was also found to be more effective than large, infrequent doses.
During the COVID-19 pandemic, interest in vitamin D surged. While it is not a cure or a replacement for vaccines and other public health measures, the science points to a supportive role.
Numerous observational studies found a strong correlation between low vitamin D levels and an increased risk of infection, hospitalization and severe outcomes from COVID-19.
While clinical trials on using vitamin D as a treatment have yielded mixed results, the consensus among many experts is that correcting a deficiency and maintaining sufficient levels is a wise, low-risk strategy to support overall immune resilience.
What is the Link Between Vitamin D and Autoimmune Diseases?
Perhaps the most surprising and profound role of vitamin D is not in activating the immune system, but in calming it down.
Autoimmune diseases—like multiple sclerosis, rheumatoid arthritis and type 1 diabetes—occur when the immune system mistakenly attacks the body’s own healthy tissues.
Vitamin D acts as a master modulator, helping to prevent this devastating friendly fire.
Calming an Overactive Response: The Adaptive Immune System
The second branch of immunity is the adaptive immune system.
This is your specialized, memory-based defense force, composed primarily of T-cells and B-cells.
In autoimmune conditions, this system becomes dysregulated.
Pro-inflammatory T-cells, particularly types known as Th1 and Th17, become overactive and lead the assault on the body’s own cells.
Vitamin D intervenes directly in this process. By binding to the VDR on these T-cells, it discourages their proliferation and reduces their production of inflammatory signaling molecules (cytokines).
But its most critical role may be in promoting a different kind of T-cell: the regulatory T-cell (Treg). As their name implies, Tregs are the peacekeepers of the immune system.
Their primary job is to suppress excessive immune reactions and tell the other aggressive cells to “stand down”.
Research published in Frontiers in Immunology highlights that vitamin D directly promotes the development and function of these Tregs, helping to maintain self-tolerance and prevent autoimmunity.
Groundbreaking Research: The VITAL Trial and Autoimmunity
For years, the link between vitamin D and autoimmunity was based on observational data.
That changed with the publication of results from the **VITAL (VITamin D and OmegA-3 TriaL)**, a large-scale, randomized clinical trial conducted by researchers at Harvard Medical School and Brigham and Women’s Hospital.
The VITAL trial, involving nearly 26.000 participants, provided the strongest evidence to date. The key finding, published in the BMJ in 2022, was that supplementation with 2.000 IU of vitamin D3 per day for five years led to a **22% reduction in the incidence of confirmed autoimmune diseases**, including rheumatoid arthritis, psoriasis and autoimmune thyroid disease.
This was a landmark result, moving the conversation from correlation to causation.
It suggests that maintaining optimal vitamin D levels could be a powerful preventative strategy against a range of debilitating autoimmune conditions.
A Closer Look at Specific Conditions: MS, RA and IBD
The evidence for vitamin D’s role is particularly strong in certain autoimmune diseases:
- Multiple Sclerosis (MS): There is a well-established geographical link where MS prevalence increases in regions farther from the equator with less sunlight. Numerous observational and genetic studies have shown that low vitamin D levels are a significant risk factor for developing MS and are associated with increased disease activity and progression in those who have it.
- Rheumatoid Arthritis (RA): Many studies have found that patients with RA are more likely to be deficient in vitamin D, and that lower levels correlate with higher disease activity and joint pain. The VITAL trial’s findings further bolster the case for its protective role.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis are also linked to vitamin D deficiency. The vitamin helps regulate the immune response in the gut lining and maintain the integrity of the gut barrier, both of which are compromised in IBD.
Are You Getting Enough? The Silent Epidemic of Deficiency
Given its critical role in immune health, ensuring adequate vitamin D levels is paramount.
However, deficiency is remarkably common, and because its symptoms can be subtle or even non-existent, many people are unaware their immune systems are operating at a disadvantage.
What Are the Symptoms of Vitamin D Deficiency?
While a blood test is the only definitive way to know your status, certain signs and symptoms can be red flags.
Many of these are directly tied to the immune dysregulation that occurs when vitamin D levels are low.
- Getting Sick Often or Frequent Infections: This is a classic sign. If you find yourself catching every cold or flu that goes around, it could be a direct result of an impaired innate immune response due to low vitamin D and insufficient production of the antimicrobial peptide cathelicidin.
- Fatigue and Tiredness: While fatigue has many causes, persistent, unexplained exhaustion is a common complaint among those with very low vitamin D levels.
- Bone and Back Pain: This is a more traditional symptom related to vitamin D’s role in calcium absorption. Aching bones, particularly in the lower back, can indicate inadequate bone mineralization.
- Depressed Mood: The link between low vitamin D and mood is an active area of research. Receptors for vitamin D are found in areas of the brain associated with mood regulation and some studies have linked deficiency to a higher risk of depression, especially seasonal affective disorder.
- Impaired Wound Healing: If cuts and scrapes seem to take an unusually long time to heal, it could be related to vitamin D’s role in controlling inflammation and fighting infection at the site of an injury.
It’s crucial to remember that these symptoms are non-specific.
However, if you experience several of them, especially frequent illness, it’s a strong reason to discuss your vitamin D status with a healthcare provider.
Who Is Most at Risk for Vitamin D Deficiency?
Certain lifestyle, genetic, and health factors can dramatically increase your risk of having low vitamin D levels.
Understanding these can help you be more proactive about your health.
- People with Darker Skin: Melanin, the pigment that gives skin its color, acts as a natural sunscreen. While this protects against skin cancer, it also reduces the skin’s ability to produce vitamin D from sunlight. Individuals with darker skin tones may need significantly more sun exposure to produce the same amount of vitamin D as someone with lighter skin.
- Older Adults: As we age, our skin becomes less efficient at synthesizing vitamin D. Furthermore, older adults may spend more time indoors and have lower dietary intakes, compounding the risk.
- People with Limited Sun Exposure: This includes office workers, individuals living in northern latitudes (like the northern U.S., Canada and Europe) where the sun’s rays are too weak for much of the year and those who consistently wear sun-protective clothing.
- Individuals with Obesity: Vitamin D is fat-soluble, meaning it can be stored in body fat. In individuals with obesity, more vitamin D is sequestered in fat tissue, making it less available for use in the bloodstream. They often require higher doses to achieve sufficient blood levels.
- People with Certain Medical Conditions: Conditions that affect fat absorption, such as Crohn’s disease, celiac disease and cystic fibrosis, can impair the absorption of vitamin D from food. Chronic kidney or liver disease can also interfere with the body’s ability to convert vitamin D into its active form.
How Can I Know My Vitamin D Level for Sure?
The only definitive way to diagnose a deficiency is with a simple blood test called the **25-hydroxyvitamin D test**, often written as 25(OH)D.
This test measures the main storage form of vitamin D in your body and is the most accurate indicator of your status.
Different organizations have slightly different cutoffs, but the general consensus, including guidelines from the National Institutes of Health (NIH), is summarized below.
| Serum 25(OH)D Level (ng/mL) | Serum 25(OH)D Level (nmol/L) | Status | Implication for Health |
|---|---|---|---|
| < 12 ng/mL | < 30 nmol/L | Deficient | Associated with rickets in children and osteomalacia in adults. Poses a significant risk for impaired immune function. |
| 12–19.9 ng/mL | 30–49.9 nmol/L | Insufficient | Generally inadequate for bone and overall health. Immune function may be suboptimal. |
| 20–29.9 ng/mL | 50–74.9 nmol/L | Sufficient (for bone health) | Considered adequate for bone health by the Institute of Medicine, but may not be optimal for other functions. |
| 30–60 ng/mL | 75–150 nmol/L | Optimal Range | Many experts and organizations like The Endocrine Society suggest this range for optimal overall health, including immune function and disease prevention. |
| > 100 ng/mL | > 250 nmol/L | Potential Toxicity | Levels this high are associated with risk of adverse effects and are typically only seen with extreme, prolonged supplement use. |
Your Action Plan: How to Optimize Vitamin D Levels
Correcting a deficiency and maintaining optimal vitamin D levels is one of the most impactful steps you can take for your immune health.
This requires a multi-pronged approach involving sensible sun exposure, dietary choices, and, for most people, supplementation.
How Much Vitamin D Do You Really Need Per Day?
This is a subject of significant debate among experts. The official Recommended Dietary Allowances (RDAs) set by the U.S.
Institute of Medicine (IOM) are based on the amount needed to maintain bone health in the general population.
- Adults 19–70 years: 600 IU (15 mcg) per day
- Adults 71+ years: 800 IU (20 mcg) per day
However, many leading researchers and organizations, including The Endocrine Society, argue that these amounts are often insufficient to achieve optimal blood levels for immune function and overall disease prevention.
They suggest that many adults may need a daily intake of **1.500–2.000 IU** to maintain a blood level of 30 ng/mL or higher.
For those who are deficient, a doctor may prescribe a higher temporary dose (e.g., 5.000 IU daily or 50.000 IU weekly) to raise levels more quickly.
The key takeaway: Don’t guess. The best approach is to get your levels tested and work with a healthcare provider to determine the right daily intake for your specific needs, lifestyle and health status.
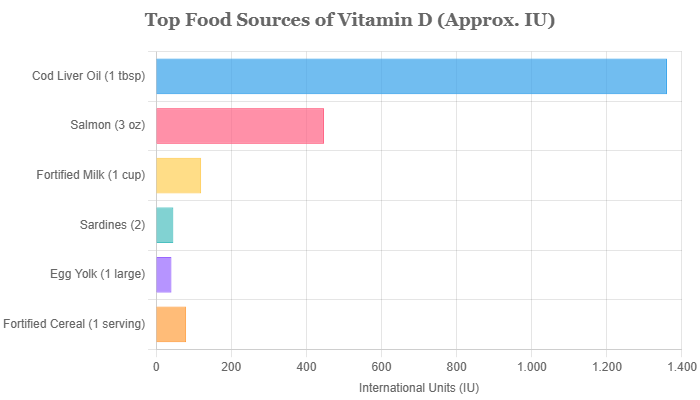
What Are the Best Food Sources of Vitamin D?
Very few foods are naturally rich in vitamin D, which is why deficiency is so common.
Relying on diet alone is challenging for most people, but including these foods can certainly help.
- Natural Sources: The best natural sources are fatty fish. Salmon, mackerel, herring, and sardines are excellent choices. Cod liver oil is exceptionally high in vitamin D. Smaller amounts are found in beef liver and egg yolks (the D is in the yolk, so don’t just eat the whites!).
- Fortified Foods: In the United States, many foods are fortified with vitamin D to help the population meet their needs. These include cow’s milk, many plant-based milks (soy, almond, oat), some orange juices, yogurts and breakfast cereals. Always check the label to confirm.
- Mushrooms: Mushrooms are a unique plant-based source. They produce vitamin D2 when exposed to UV light. Some brands specifically treat their mushrooms with UV light to boost their vitamin D content.
Should I Supplement with Vitamin D2 or Vitamin D3?
When you walk down the supplement aisle, you’ll see two main forms of vitamin D: D2 and D3.
The choice is clear and backed by strong scientific evidence.
Vitamin D3 (cholecalciferol) is the superior choice. This is the form of vitamin D that your body naturally produces in the skin in response to sunlight. It is also the form found in animal-based foods like fatty fish.
Vitamin D2 (ergocalciferol) is derived from plant sources, like yeast or mushrooms.
While it can raise blood levels of vitamin D, multiple studies and meta-analyses have concluded that **D3 is significantly more effective and potent** at raising and maintaining 25(OH)D concentrations in the blood over the long term.
A study published in the American Journal of Clinical Nutrition found D3 to be about 87% more potent than D2 in raising vitamin D levels.
For this reason, most experts and clinicians recommend D3 supplements.
Can You Get Enough Vitamin D From the Sun Safely?
Sunlight is the most natural and potent way to get vitamin D.
When UVB rays from the sun hit your skin, a cholesterol precursor is converted into vitamin D3.
However, its effectiveness is highly variable and depends on:
- Latitude and Season: Above about 37 degrees north latitude (roughly a line running through San Francisco, St. Louis and Richmond), the sun’s rays are too weak from about November to March to produce any vitamin D.
- Time of Day: Production is most efficient during midday hours (roughly 10 a.m. to 3 p.m.) when the sun is highest in the sky.
- Skin Tone: As mentioned, darker skin requires longer exposure.
- Age: Older skin is less efficient at production.
- Sunscreen: Sunscreen with an SPF of 30 or higher can reduce vitamin D synthesis in the skin by more than 95%.
A balanced recommendation for many people with lighter skin during peak months is **10-30 minutes of midday sun exposure** to the arms, legs and back a few times per week, *without sunscreen*.
After this short period, it is crucial to apply sunscreen to protect against skin aging and the risk of skin cancer.
It’s a delicate balance, and for many, especially during winter or for those at high risk, supplementation remains the most reliable strategy.
Safety, Synergy and Final Considerations
Optimizing your vitamin D status is not just about taking a supplement, it’s about understanding the full context of how it works in your body.
This includes being aware of safety limits and the other key nutrients that work in concert with vitamin D.
Can You Take Too Much Vitamin D?
The short answer is yes, but it is very difficult to do. **Vitamin D toxicity is extremely rare** and does not occur from sun exposure (your body has a feedback mechanism to stop production) or from food.
It is almost always the result of taking massive doses of supplements (e.g., over 50.000 IU daily) for extended periods.
The main consequence of toxicity is a buildup of calcium in the blood, a condition called hypercalcemia. This can cause symptoms like nausea, vomiting, weakness, frequent urination and can eventually lead to bone pain and kidney problems.
To prevent this, the Institute of Medicine has set a Tolerable Upper Intake Level (UL) for most adults at **4.000 IU (100 mcg) per day**.
While doses higher than this may be used therapeutically under a doctor’s supervision for short periods, you should not exceed this amount on your own.
Do Other Nutrients Affect How Vitamin D Works?
Vitamins and minerals rarely work in isolation. For vitamin D to function optimally, it relies on several key partners.
This is a nuance often missed in basic health advice but is critical for getting the most benefit.
- Magnesium: This is arguably the most important co-factor. Magnesium is required for the enzymatic reactions in both the liver and the kidneys that convert the storage form of vitamin D (from sun or supplements) into its active hormonal form, calcitriol. A significant portion of the population is also insufficient in magnesium, meaning that even if you take vitamin D, your body may not be able to use it effectively without enough magnesium.
- Vitamin K2: Vitamin D and Vitamin K2 have a powerful synergistic relationship, particularly for bone and cardiovascular health. Vitamin D’s primary role is to increase calcium absorption from the gut. Vitamin K2’s job is to direct that calcium to the right places (bones and teeth) and keep it out of the wrong places (arteries and soft tissues). Taking high doses of vitamin D without adequate K2 could theoretically lead to calcium deposition in arteries, so many experts recommend taking them together.
Ensuring you have adequate intake of these co-factors, particularly magnesium, is an advanced strategy for maximizing the benefits of your vitamin D optimization plan.
Frequently Asked Questions (FAQ)
1. How does vitamin D boost immunity?
Vitamin D helps immune cells produce natural antibiotic-like substances (like cathelicidin) to kill pathogens. It also acts as a modulator, preventing the immune system from overreacting and causing autoimmune damage by promoting regulatory T-cells.
2. What is the best form of vitamin D to take?
Vitamin D3 (cholecalciferol) is the best form. It is the type your body makes from sunlight and is proven to be significantly more effective at raising and maintaining blood vitamin D levels compared to vitamin D2.
3. Can low vitamin D make you sick all the time?
Yes. A key sign of deficiency is getting frequent infections, like colds or the flu. This is because low vitamin D impairs your innate immune system’s ability to fight off invading viruses and bacteria effectively.
4. How long does it take to correct a vitamin D deficiency?
With proper supplementation under a doctor’s guidance, it typically takes 2-3 months to correct a deficiency and reach optimal blood levels. Consistency is key, as levels will drop again if supplementation is stopped.
5. Will I get enough vitamin D if I sit by a window?
No. Window glass (like UVB-blocking glass in cars) blocks the specific UVB rays required for your skin to produce vitamin D. You must have direct sun exposure on your skin to generate vitamin D.
6. Is 2.000 IU of vitamin D3 safe to take daily?
For most adults, yes. 2.000 IU per day is well within the safe upper limit of 4.000 IU and is the dose used in many clinical trials, like the VITAL study, for long-term health benefits. However, it’s always best to consult your doctor.
7. Does vitamin D help with inflammation?
Yes, it is a potent anti-inflammatory agent. It works by reducing the production of pro-inflammatory cytokines and discouraging the proliferation of inflammatory immune cells, which is why it’s so important in managing and preventing autoimmune conditions.
8. What’s the difference between vitamin D and D3?
Vitamin D is the general name for the nutrient. Vitamin D3 (cholecalciferol) is a specific form, the one made in your skin and found in animal foods. Vitamin D2 is the plant-based form. D3 is the preferred form for supplementation.
Conclusion
We have journeyed deep into the science of vitamin D, moving far beyond its reputation as a simple bone vitamin.
The evidence is clear and compelling: vitamin D is a sophisticated hormonal regulator that is absolutely essential for a balanced and effective immune system.
It sharpens your body’s innate defenses to fight off pathogens while simultaneously calming your adaptive immune system to prevent the friendly fire of autoimmunity.
The silent epidemic of deficiency means that a significant portion of the population is navigating the world with a compromised immune shield. But the good news is that this is a correctable problem.
Through awareness, sensible sun exposure, a targeted diet, and, most importantly, smart and consistent supplementation, you can restore your body’s supply of this critical nutrient.
The single most important step you can take is to move from guessing to knowing.
Talk to your healthcare provider about getting your 25(OH)D levels checked.
This simple test provides the data needed to create a personalized plan, ensuring your immune system has the robust support it needs to protect you today and for years to come.
We encourage you to share this article and discuss your own experiences or questions in the comments below.
Empowering ourselves and our communities with this knowledge is the first step toward better health for all.
Reference
[1] The Anti-Inflammatory Roles of Vitamin D for Improving Human Health
https://pmc.ncbi.nlm.nih.gov/articles/PMC11674702
[2] Vitamin D, the immune system, and its relationship with diseases
https://epag.springeropen.com/articles/10.1186/s43054-022-00135-w
[3] Vitamin D Deficiency: Causes, Symptoms & Treatment
https://my.clevelandclinic.org/health/diseases/15050-vitamin-d-vitamin-d-deficiency
[4] Vitamin D’s Effect on Immune Function – PMC – PubMed Central
https://pmc.ncbi.nlm.nih.gov/articles/PMC7281985
[5] Vitamin D: recent advances, associated factors, and its role in …
https://www.nature.com/articles/s41538-025-00460-5
[6] Immunomodulatory actions of vitamin D in various immune-related …
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.950465/full
[7] Vitamin D2 vs. Vitamin D3: What’s the Difference?
https://www.verywellhealth.com/vitamin-d-two-vs-d-three-7095309
[8] The Human Cathelicidin Antimicrobial Peptide (CAMP) Gene Is a …
[9] Role of vitamin D in COVID-19 and other viral infections

