Cholesterol is a vital, waxy substance your body needs, but high levels in your blood can silently increase your risk for heart disease and stroke.
Understanding your key numbers—LDL, HDL, and triglycerides—is the single most important first step you can take to protect your cardiovascular health for years to come.
This isn’t a minor issue. According to the World Heart Federation, high cholesterol is a major controllable risk factor that contributes to an estimated 4.4 million deaths worldwide each year.
Despite its prevalence, high cholesterol is often misunderstood, shrouded in myths and confusion.
Many people don’t even know they have it until a major health event occurs.
This comprehensive guide is designed to cut through the noise.
We will demystify your blood test results, explain the crucial difference between “good” and “bad” cholesterol, and provide a clear, evidence-based action plan.
You will learn about powerful lifestyle changes and the latest medical treatments, all grounded in guidelines from leading health organizations like the American Heart Association (AHA) and the National Heart, Lung, and Blood Institute (NHLBI).
It’s time to take control of your numbers and your health.
In This Article
What Is Cholesterol and Why Does Your Body Need It?
Before we label cholesterol as a villain, it’s crucial to understand its fundamental role.
Far from being inherently bad, cholesterol is an essential building block for life.
It’s a type of lipid—a waxy, fat-like substance—that is so important, your liver produces all the cholesterol your body needs to function correctly.
What Exactly Is Cholesterol?
Think of cholesterol as a multi-purpose tool used throughout your body.
It’s a structural component of every single cell you have, providing stability and flexibility to cell membranes.
Without it, our cells would be fragile and dysfunctional.
Beyond this structural role, cholesterol is a precursor for several critical substances.
Key Insight: Your body manufactures about 75% of the cholesterol in your blood. The other 25% comes from the food you eat, primarily from animal products. This is why both genetics and diet play a role in your overall cholesterol levels.
Here are some of the essential functions of cholesterol:
- Building Cell Membranes: It provides structural integrity to the outer layer of all animal cells, regulating what enters and exits.
- Producing Hormones: Cholesterol is the starting material for creating vital steroid hormones, including stress hormones like cortisol and sex hormones like testosterone and estrogen.
- Making Vitamin D: When your skin is exposed to sunlight, it converts a form of cholesterol into Vitamin D, which is essential for bone health and immune function.
- Creating Bile Acids: Your liver converts cholesterol into bile acids, which are necessary for digesting fats and absorbing fat-soluble vitamins (A, D, E, and K) in your gut.
What’s the Difference Between “Good” (HDL) and “Bad” (LDL) Cholesterol?
Since cholesterol is a fatty substance, it doesn’t mix well with blood, which is mostly water.
To travel through the bloodstream, cholesterol is packaged into particles called lipoproteins.
These are like tiny transport vehicles made of fat (lipid) on the inside and protein on the outside.
The type of lipoprotein determines whether cholesterol is considered “good” or “bad”.
The Transport Analogy:
Imagine your arteries are highways. Lipoproteins are the “transport trucks” carrying cholesterol cargo.
- LDL (Low-Density Lipoprotein) trucks are responsible for delivering cholesterol from the liver to cells throughout the body. When there are too many LDL trucks on the highway, they can get stuck, break down and spill their cargo into the artery walls. This causes a “traffic jam” that builds up over time, forming plaque.
- HDL (High-Density Lipoprotein) trucks are the “cleanup crew”. They travel through the highways, pick up excess cholesterol from the arteries and other tissues and transport it back to the liver for disposal.
Low-Density Lipoprotein (LDL): The “Bad” Cholesterol
LDL cholesterol is often called “bad” because when you have high levels of it, it contributes directly to the formation of plaque in your arteries.
This process is called atherosclerosis. The plaque is a thick, hard deposit that can narrow the arteries, making them less flexible.
This restriction of blood flow can lead to serious complications, including chest pain (angina), heart attack, or stroke if a plaque ruptures and forms a blood clot.
High-Density Lipoprotein (HDL): The “Good” Cholesterol
HDL cholesterol earns its “good” reputation because it acts as a scavenger.
High levels of HDL are protective because they indicate that your body is efficient at removing excess cholesterol from your arteries.
A higher HDL level is associated with a lower risk of cardiovascular disease.
This is why, unlike other cholesterol numbers, a higher HDL is better.
Triglycerides: The Other Fat in Your Blood
While often discussed alongside cholesterol, triglycerides are a different type of lipid.
They are the most common type of fat in your body and serve as a major source of energy.
When you eat, your body converts any calories it doesn’t need to use right away into triglycerides, which are then stored in your fat cells.
High triglyceride levels, especially when combined with high LDL or low HDL cholesterol, are a dangerous combination.
This pattern, known as dyslipidemia, significantly accelerates the process of atherosclerosis and is a strong predictor of heart disease, particularly in individuals with metabolic syndrome or type 2 diabetes.
Decoding Your Numbers: A Practical Guide to Your Lipid Panel
Understanding your cholesterol isn’t about guesswork, it’s about data.
A simple blood test, known as a lipid panel or lipid profile, provides a detailed snapshot of the fats circulating in your bloodstream.
This section will empower you to read and interpret your own results like a pro.
How Do I Get My Cholesterol Checked?
A lipid panel is a routine blood test.
A healthcare professional will draw a small sample of blood, usually from a vein in your arm.
To ensure the most accurate results, you will typically be asked to fast for 9 to 12 hours before the test.
This means consuming nothing but water.
Fasting is particularly important for an accurate triglyceride measurement.
Since triglyceride levels can rise significantly after a meal, eating before the test can artificially inflate this number and, consequently, your calculated total cholesterol.
Always follow your doctor’s specific instructions.
What Are Healthy Cholesterol Levels? (The Master Chart)
Your lipid panel results will be reported in milligrams per deciliter (mg/dL).
While your doctor will interpret these numbers in the context of your overall health, understanding the general guidelines is crucial.
The following table, based on data from the NHLBI and Cleveland Clinic, provides a comprehensive overview of cholesterol levels for different groups.
Important Note: For individuals with existing heart disease, diabetes, or multiple risk factors, your doctor may recommend much lower LDL targets (e.g., below 70 mg/dL or even below 55 mg/dL) for optimal protection.
| Category | Level | Children & Teens (≤19) | Adults (≥20) |
|---|---|---|---|
| Total Cholesterol | Optimal | < 170 mg/dL | 125-200 mg/dL |
| Borderline High | 170-199 mg/dL | 200-239 mg/dL | |
| High | ≥ 200 mg/dL | ≥ 240 mg/dL | |
| LDL (“Bad”) Cholesterol | Optimal | < 110 mg/dL | < 100 mg/dL |
| Near Optimal | 110-129 mg/dL | 100-129 mg/dL | |
| Borderline High | – | 130-159 mg/dL | |
| High / Very High | ≥ 130 mg/dL | ≥ 160 mg/dL (High) ≥ 190 mg/dL (Very High) | |
| HDL (“Good”) Cholesterol | Optimal (Protective) | > 45 mg/dL | ≥ 60 mg/dL |
| Acceptable / Poor | – | Men: < 40 mg/dL (Poor) Women: < 50 mg/dL (Poor) | |
| Triglycerides | Optimal | < 90 mg/dL | < 150 mg/dL |
| Borderline High | 90-129 mg/dL | 150-199 mg/dL | |
| High / Very High | ≥ 130 mg/dL | ≥ 200 mg/dL (High) ≥ 500 mg/dL (Very High) |
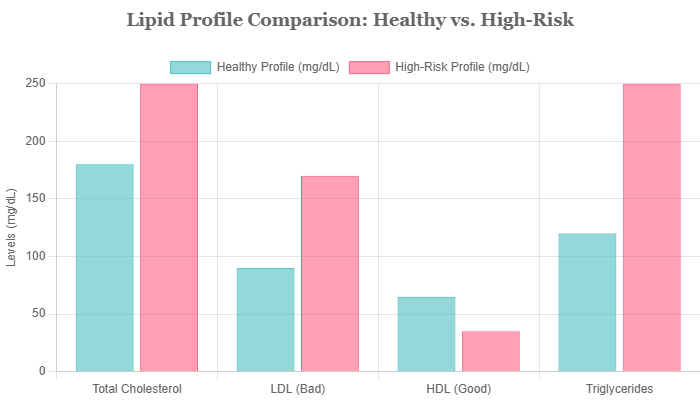
Visual comparison of a healthy lipid profile versus a high-risk profile, illustrating the contribution of each component.
What Is Non-HDL Cholesterol and Why Is It Important?
This is a value you might see on your report, or you can calculate it yourself: Total Cholesterol – HDL Cholesterol = Non-HDL Cholesterol.
This number represents all the “bad” cholesterol-carrying lipoproteins in your blood, including LDL, VLDL (Very-Low-Density Lipoprotein) and others.
Many experts now believe that non-HDL cholesterol is a better predictor of cardiovascular risk than LDL alone.
Why? Because it captures the total burden of artery-clogging particles.
While LDL is the primary target of therapy, a high non-HDL level can signal a risk even if your LDL is near-optimal.
For most adults, a healthy non-HDL cholesterol goal is below 130 mg/dL.
How Often Should I Have My Cholesterol Tested?
The frequency of cholesterol testing depends on your age, family history and existing risk factors.
The Centers for Disease Control and Prevention (CDC) and AHA provide the following general recommendations:
- Children and Adolescents: Should be tested at least once between ages 9 and 11, and again between ages 17 and 21. Testing may start earlier and be more frequent if there is a strong family history of high cholesterol or premature heart disease.
- Low-Risk Adults (Age 20+): Most healthy adults should have their cholesterol checked every 4 to 6 years.
- Individuals with Risk Factors: If you have risk factors such as a family history of high cholesterol, heart disease, diabetes, high blood pressure, or if you smoke or are obese, your doctor will likely recommend more frequent testing (e.g., annually or even more often).
- Individuals on Treatment: If you are taking cholesterol-lowering medication, your doctor will monitor your levels more regularly (e.g., 4-12 weeks after starting or changing a dose, and then every 3-12 months thereafter) to ensure the treatment is effective.
The Risks of High Cholesterol: From Causes to Consequences
One of the most dangerous aspects of high cholesterol is its insidious nature.
It doesn’t announce its presence with pain or discomfort.
Instead, it works silently in the background, setting the stage for life-threatening events.
Understanding the causes and the chain of events it triggers is key to appreciating the need for proactive management.
What Are the Symptoms of High Cholesterol?
To be perfectly clear: high cholesterol itself has no symptoms. It is a silent condition.
You can have dangerously high levels for years, or even decades and feel completely fine.
The only way to know you have it is through a blood test.
The “symptoms” people associate with high cholesterol are actually the symptoms of its consequences—advanced atherosclerosis. These can include:
- Angina (Chest Pain): Caused by reduced blood flow to the heart.
- Heart Attack: Occurs when blood flow to a part of the heart is completely blocked.
- Stroke: Occurs when blood flow to the brain is blocked.
- Peripheral Artery Disease (PAD): Leg pain when walking, caused by narrowed arteries in the limbs.
In very rare and severe cases of genetic high cholesterol, a person might develop visible signs called xanthomas.
These are yellowish, fatty deposits that can appear on the skin (especially around the eyelids), joints or on tendons.
What Causes High Cholesterol?
High cholesterol is typically the result of a complex interplay between lifestyle and genetics.
Some factors are within our power to change, while others are not.
Lifestyle Factors You Can Control
- Unhealthy Diet: A diet high in saturated fats (found in red meat, full-fat dairy, butter and tropical oils like coconut and palm oil) and trans fats (found in some fried foods and commercially baked goods) is the primary dietary driver of high LDL cholesterol.
- Lack of Physical Activity: A sedentary lifestyle lowers protective HDL cholesterol and can contribute to weight gain, which in turn raises LDL and triglycerides.
- Obesity: Having a body mass index (BMI) of 30 or greater is strongly linked to higher levels of LDL and triglycerides and lower levels of HDL.
- Smoking: Smoking damages the lining of your blood vessels, making them more susceptible to plaque buildup. It also significantly lowers HDL cholesterol.
- Excessive Alcohol Consumption: Drinking too much alcohol can raise triglyceride levels and contribute to high blood pressure and weight gain.
Factors You Cannot Control
- Genetics & Family History: Your genes can influence how your body produces and clears cholesterol. A condition called Familial Hypercholesterolemia (FH) is a prime example. It’s a genetic disorder that causes extremely high LDL levels from birth, leading to a very high risk of premature heart disease. If your parents have high cholesterol, you are more likely to have it too.
- Age and Sex: Cholesterol levels naturally tend to rise with age. Before menopause, women typically have lower total cholesterol levels than men of the same age. After menopause, however, women’s LDL levels often increase.
- Other Medical Conditions: Certain conditions like chronic kidney disease, hypothyroidism, and type 2 diabetes can negatively affect cholesterol levels.
How Does High Cholesterol Lead to Heart Disease?
The journey from high cholesterol to a heart attack is a slow, progressive process known as atherosclerosis.
It unfolds over many years through a predictable sequence of events:
- Excess LDL in the Blood: When there is more LDL cholesterol than the body’s cells can use, these particles continue to circulate in the bloodstream.
- Infiltration and Oxidation: LDL particles penetrate the inner lining of the artery wall (the endothelium). Once inside, they can become chemically modified (oxidized), which triggers an inflammatory response.
- Immune Response and Plaque Formation: The body’s immune system sends white blood cells (macrophages) to the site to “clean up” the oxidized LDL. These macrophages engulf the LDL, becoming “foam cells”. As these foam cells accumulate and die, they form the core of a fatty streak, the earliest form of an atherosclerotic plaque.
- Plaque Growth and Artery Narrowing: Over time, more cholesterol, cellular waste, calcium, and other substances build up. A fibrous cap forms over the plaque. This growing plaque narrows the artery’s channel, restricting the flow of oxygen-rich blood.
- Plaque Rupture and Clot Formation: The most dangerous event occurs when the fibrous cap on a plaque becomes unstable and ruptures. The body perceives this as an injury and rushes to form a blood clot (a thrombus) at the site. This clot can rapidly grow and completely block the artery, cutting off blood flow and causing a heart attack or stroke.
Taking Control: Your Action Plan for Lowering Cholesterol
Receiving a high cholesterol diagnosis is not a sentence—it’s a call to action.
The good news is that cholesterol levels are highly manageable.
For many, a combination of dedicated lifestyle changes can produce dramatic improvements.
For others, these changes, combined with modern medications, can effectively control risk.
How Can I Lower My Cholesterol Naturally with Diet and Exercise?
Lifestyle modification is the cornerstone of cholesterol management.
The Therapeutic Lifestyle Changes (TLC) program, developed by the NHLBI, is a proven framework for success.
The Heart-Healthy Eating Plan
Your diet has a profound impact on your cholesterol.
The focus should be on reducing harmful fats and increasing beneficial ones, along with fiber.
- Reduce Saturated and Trans Fats: This is the most effective dietary change for lowering LDL cholesterol.
- Limit: Red meat (beef, pork, lamb), processed meats (sausages, bacon), poultry with skin, full-fat dairy products (butter, cheese, cream) and tropical oils (coconut, palm).
- Eliminate: Industrially produced trans fats, often listed as “partially hydrogenated oils” on labels of fried foods, stick margarines, and some commercial baked goods.
- Increase Soluble Fiber: Soluble fiber acts like a sponge in your digestive system, binding to cholesterol and preventing its absorption into the bloodstream.
- Excellent Sources: Oats (oatmeal, oat bran), barley, beans, lentils, apples, pears, citrus fruits and Brussels sprouts. Aim for at least 10-25 grams of soluble fiber per day.
- Embrace Unsaturated Fats: Monounsaturated and polyunsaturated fats can help lower LDL levels and are beneficial for overall heart health.
- Good Sources: Avocados, nuts (almonds, walnuts), seeds (flax, chia) and vegetable oils like olive oil and canola oil.
- Add Omega-3 Fatty Acids: While they don’t directly lower LDL, omega-3s reduce triglycerides and inflammation and have other heart-protective benefits.
- Find them in: Fatty fish like salmon, mackerel, herring, and sardines (aim for two servings per week), as well as walnuts and flaxseeds.
The Power of Physical Activity
Exercise is a potent tool for improving your lipid profile.
It is one of the most effective ways to raise protective HDL cholesterol.
It also helps lower LDL and triglycerides, aids in weight management and improves overall cardiovascular fitness.
The Mayo Clinic recommends aiming for at least 150 minutes of moderate-intensity aerobic exercise (like brisk walking, swimming or cycling) or 75 minutes of vigorous-intensity aerobic exercise (like running or HIIT) per week, spread throughout the week. Incorporating resistance training (weight lifting) at least two days a week provides additional benefits.
What Medications Are Used to Treat High Cholesterol?
When lifestyle changes are not enough to reach your cholesterol goals, or if your risk is very high, your doctor will recommend medication.
These drugs are highly effective and have been extensively studied.
Statins: The First Line of Defense
Statins are the most commonly prescribed and most effective class of drugs for lowering LDL cholesterol.
They work by blocking a key enzyme in the liver (HMG-CoA reductase) that is necessary for producing cholesterol.
This reduction in liver cholesterol production prompts the liver to pull more LDL cholesterol out of the bloodstream.
Commonly prescribed statins include Atorvastatin (Lipitor), Rosuvastatin (Crestor) and Simvastatin (Zocor).
They can lower LDL by 20% to over 50%, depending on the drug and dose.
Understanding Statin Side Effects
While statins are safe and well-tolerated by most people, they can have side effects.
It’s important to discuss any concerns with your doctor.
The most common reported side effect is muscle pain (myalgia).
In most cases, this is mild, but if you experience significant or persistent muscle pain or weakness, you should contact your doctor immediately.
Other potential side effects include digestive issues and a small increased risk of developing type 2 diabetes or elevated liver enzymes.
However, for individuals who need them, the cardiovascular benefits of statins overwhelmingly outweigh the risks.
Beyond Statins: Other Cholesterol-Lowering Drugs
For patients who cannot tolerate statins or who need additional LDL lowering, other medications are available:
- Ezetimibe (Zetia): This drug works differently from statins. It blocks the absorption of cholesterol from food in the small intestine. It is often prescribed in combination with a statin.
- PCSK9 Inhibitors: A powerful class of injectable drugs (like Repatha and Praluent) that dramatically lower LDL. They work by blocking a protein called PCSK9, which allows the liver to remove much more LDL from the blood. They are typically used for high-risk patients or those with familial hypercholesterolemia.
- Bile Acid Sequestrants: These drugs (like cholestyramine) work in the intestines by binding to bile acids, forcing the liver to use more cholesterol to make new bile acids, thus lowering blood cholesterol.
- Inclisiran (Leqvio): A newer-generation injectable therapy that uses RNA interference to lower LDL cholesterol. It requires only two injections per year after the initial doses. Recent research, as highlighted in a 2025 review on PubMed Central, confirms its effectiveness in lowering LDL, though long-term cardiovascular outcome data is still being gathered.
Debunking Common Cholesterol Myths
Misinformation about cholesterol is rampant.
Let’s clear up some of the most persistent myths with evidence-based facts, drawing from sources like the CDC.
Myth: Are Eggs Bad for My Cholesterol?
Fact: For decades, eggs were villainized because their yolks are high in dietary cholesterol. However, extensive research has shown that for most people, dietary cholesterol has a much smaller impact on blood cholesterol levels than saturated and trans fats do. The 2015-2020 Dietary Guidelines for Americans removed the specific daily limit on dietary cholesterol. Enjoying eggs in moderation as part of a balanced diet is perfectly fine for most individuals.
Myth: If I’m Thin, Do I Need to Worry About Cholesterol?
Fact: This is a dangerous misconception. People of all body types and weights can have high cholesterol. While obesity is a risk factor, genetics play a powerful role. A thin person with a genetic predisposition for high cholesterol can have much higher levels than an overweight person without that genetic trait. No one is immune, and everyone should be tested.
Myth: Is All Cholesterol Bad?
Fact: As we’ve established, this is false. Your body needs cholesterol to build cells, make hormones, and perform other vital functions. The key is the balance and the type of lipoprotein carrying it. HDL (“good”) cholesterol is actively protective, and having high levels of it is beneficial. The problem arises from an excess of LDL (“bad”) cholesterol.
Myth: Can I Stop My Medication Once My Numbers Are Normal?
Fact: Absolutely not, unless directed by your doctor. Cholesterol-lowering medications like statins are not a “cure”. They work to control your cholesterol levels while you are taking them. Your numbers are normal *because* the medication is working. Stopping the medication will almost certainly cause your cholesterol levels to return to their previous high state, along with the associated risks.
Your Cholesterol Questions Answered (FAQ Section)
1. What is a dangerous level of LDL cholesterol?
An LDL level of 190 mg/dL or higher is considered very high and dangerous, often suggesting a genetic cause like familial hypercholesterolemia. However, any level above 160 mg/dL is high, and for people with other risk factors, even levels above 100 mg/dL may require treatment.
2. Can drinking water lower cholesterol?
While staying well-hydrated is essential for overall health, drinking water does not directly lower cholesterol. However, choosing water over sugary drinks can help with weight management, which indirectly supports healthy cholesterol levels.
3. What is the best drink to lower cholesterol?
Drinks rich in soluble fiber or antioxidants can help. Green tea, oat milk, and soy milk are good choices. Tomato juice is rich in lycopene, which can improve lipid levels, and drinks with plant sterols/stanols are specifically designed to lower cholesterol.
4. Can stress cause high cholesterol?
Chronic stress can indirectly lead to high cholesterol. It may trigger unhealthy coping mechanisms like poor diet choices, physical inactivity, and smoking. Some research also suggests stress hormones like cortisol may directly influence cholesterol production.
5. What is the fastest way to lower cholesterol?
The fastest way is typically with high-intensity statin medication, which can show significant results in weeks. For lifestyle changes, a very strict diet low in saturated fat and high in soluble fiber, combined with daily exercise, can also produce noticeable changes within a few months.
6. Can you have high cholesterol and be a vegetarian?
Yes. While vegetarian diets are often lower in saturated fat, they can still contain it from sources like full-fat dairy, cheese, and tropical oils. Furthermore, genetics play a major role, so even with a perfect diet, some individuals may still have genetically high cholesterol.
7. Does VLDL cholesterol matter?
Yes. VLDL (Very-Low-Density Lipoprotein) mainly carries triglycerides. High VLDL levels contribute to plaque buildup and are part of the “non-HDL cholesterol” calculation. High triglycerides are a key component of VLDL, making it an important risk factor.
8. What is Lipoprotein(a) or Lp(a)?
Lp(a) is a specific type of LDL-like particle whose level is almost entirely determined by genetics. High Lp(a) is a significant independent risk factor for heart disease and stroke. It is not measured in a standard lipid panel but can be ordered as a separate test, especially for those with a strong family history of premature heart disease.
Conclusion
Understanding cholesterol is the first, most powerful step toward safeguarding your long-term cardiovascular health.
We’ve journeyed from the basic science of this essential lipid to the practical realities of managing it.
The critical takeaways are clear:
- Cholesterol is not the enemy, excess “bad” cholesterol is. Your body needs it, but an imbalance, particularly high LDL and triglycerides with low HDL, silently fuels heart disease.
- Know your numbers. A simple lipid panel is your personal risk report. Understanding your Total, LDL, HDL, and Triglyceride levels is non-negotiable for proactive health management.
- Lifestyle changes are your first line of defense. A heart-healthy diet and regular physical activity are potent tools that can dramatically improve your lipid profile and overall well-being.
- Modern medicine offers a powerful safety net. When lifestyle isn’t enough, medications like statins are proven to be safe and highly effective at reducing risk and preventing heart attacks and strokes.
Your cholesterol numbers are not just data points on a lab report, they are a direct reflection of your internal health and a predictor of your future.
Don’t wait for symptoms to appear—by then, the damage is already done. Be proactive.
Schedule a check-up with your healthcare provider. Discuss your personal risk factors, get your cholesterol tested, and work together to create a personalized management plan. Taking charge of your cholesterol today is one of the greatest investments you can make in a longer, healthier life.
We invite you to share your own experiences, questions, or successes in the comments below.
Your journey can inspire and help others on their path to better heart health.
Reference
[1] Cholesterol: Understanding Levels & Numbers – Cleveland Clinic
https://my.clevelandclinic.org/health/articles/11920-cholesterol-numbers-what-do-they-mean
[2] Statin side effects: Weigh the benefits and risks – Mayo Clinic
[3] Therapeutic Lifestyle Changes (TLC) To Lower Cholesterol – NHLBI
https://www.nhlbi.nih.gov/education/TLC-Therapeutic-Lifestyle-Changes-Lower-Cholesterol
[4] High Cholesterol & Cardiovascular Health – World Heart Federation
https://world-heart-federation.org/what-we-do/cholesterol/
[5] Top 5 lifestyle changes to improve your cholesterol – Mayo Clinic
[6] Cholesterol Myths and Facts – CDC
https://www.cdc.gov/cholesterol/about/myths.html
[7] Blood Cholesterol – Diagnosis | NHLBI, NIH
https://www.nhlbi.nih.gov/health/blood-cholesterol/diagnosis
[8] Current usage of inclisiran for cardiovascular diseases