Epididymitis is the inflammation of the epididymis, a coiled tube at the back of the testicle that stores and carries sperm.
This condition is a significant cause of scrotal pain and discomfort, affecting over 600.000 men in the United States each year, making it the most common cause of acute scrotal pain in adults.
While often caused by a bacterial infection, including sexually transmitted infections (STIs), it can also arise from other issues.
Understanding the signs, causes, and proper treatment of epididymitis is crucial for a swift recovery and preventing serious complications.
This comprehensive guide will walk you through everything you need to know about epididymitis.
We will explore its symptoms in detail, uncover the various causes, explain how doctors diagnose the condition, and outline the most effective treatment strategies.
By the end of this article, you will have a clear understanding of how to manage epididymitis and when to seek medical care.
In This Article
What is Epididymitis? A Detailed Overview
To fully grasp what epididymitis is, it’s helpful to first understand the anatomy involved and the different forms the condition can take.
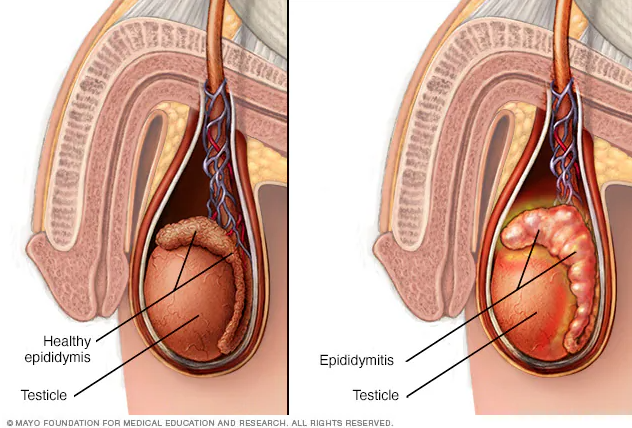
Epididymitis is an inflammation of the coiled tube, called the epididymis, at the back of the testicle.
Defining Epididymitis
Epididymitis (pronounced ep-ih-did-uh-MY-tis) is a medical condition characterized by inflammation of the epididymis.
This inflammation causes swelling, redness, and pain in the scrotum.
While it can affect males of any age, it is most frequently diagnosed in those between 20 and 40 years old.
The primary cause is typically a bacterial infection that travels up the urinary tract.
The Anatomy of the Epididymis: A Quick Guide
The epididymis is a vital component of the male reproductive system.
It is a single, long, tightly coiled tube that sits on the posterior (back) surface of each testicle. Its primary function is to transport, mature, and store sperm produced in the testes.
The epididymis can be divided into three sections:
- The Head (Globus Major): The most proximal part, which connects to the testes via the efferent ductules. It receives immature sperm from the testes.
- The Body (Corpus): The middle section where sperm continue to mature and gain motility (the ability to swim).
- The Tail (Cauda): The most distal part, which connects to the vas deferens. The tail serves as the primary storage site for mature sperm before ejaculation.
Inflammation usually begins in the tail of the epididymis and can spread to the body and head, and sometimes to the testicle itself.
Acute vs. Chronic Epididymitis: Understanding the Difference
Epididymitis is classified as either acute or chronic based on the duration of symptoms. This distinction is critical as it can influence the diagnostic approach and treatment plan.
| Feature | Acute Epididymitis | Chronic Epididymitis |
|---|---|---|
| Duration | Symptoms last for less than 6 weeks. | Symptoms persist for 6 weeks or longer, or the condition recurs frequently. |
| Onset of Pain | Usually gradual over one to two days, but can be sudden. | Often a slow, insidious onset of discomfort or a dull ache. |
| Symptoms | Characterized by significant pain, swelling, redness, and warmth in the scrotum. Fever and urinary symptoms are common. | Primarily characterized by long-standing pain or discomfort, often without significant swelling. The pain may be constant or intermittent. |
| Common Cause | Bacterial infection (STI or urinary pathogens). | The cause is often difficult to identify (idiopathic). It may follow an unresolved acute infection or be related to other structural or nerve-related issues. |
What is Epididymo-orchitis?
Due to the close proximity of the epididymis and the testicle, inflammation can easily spread from one to the other.
When epididymitis spreads to the adjacent testicle, the condition is called epididymo-orchitis.
Orchitis is the inflammation of a testicle. It can be difficult, even for a doctor, to distinguish whether the inflammation is confined to the epididymis, the testicle, or both.
Therefore, healthcare professionals often use the term “epididymo-orchitis” to describe the condition, especially when significant swelling is present.
How Common is Epididymitis? (Epidemiology and Statistics)
Epididymitis is a relatively common urological condition with a significant impact on men’s health and the healthcare system.
Incidence in the United States and Globally
According to data from sources like the Centers for Disease Control and Prevention (CDC) and research published in StatPearls, epididymitis is a widespread issue:
- An estimated 600.000 cases of acute epididymitis are diagnosed in the United States each year.
- It accounts for approximately 1 in 1.000 men developing the condition annually.
- Epididymitis is the fifth most common urologic diagnosis for men between the ages of 18 and 50.
- Globally, studies show varying incidence rates, with a European study estimating it at 2.45 per 1.000 men.
Age-Related Demographics: Who is Most at Risk?
The cause and prevalence of epididymitis vary significantly with age:
- Men aged 20-39: This group sees the highest incidence. The vast majority of cases (around 50%) are caused by sexually transmitted infections, primarily Chlamydia trachomatis and Neisseria gonorrhoeae.
- Men over 39: In this age group, the cause is more commonly non-sexually transmitted bacteria, such as Escherichia coli (E. coli), often associated with urinary tract infections (UTIs) or bladder outlet obstruction from an enlarged prostate (benign prostatic hyperplasia).
- Prepubertal Children: Epididymitis is less common in children but does occur, with an annual incidence of about 1.2 per 1.000 boys. In this group, it is often linked to structural abnormalities of the urinary tract, urine reflux, or post-infectious syndromes rather than STIs. The mean age of presentation is around 9-11 years.
Impact on Healthcare Systems
The condition leads to a substantial number of medical visits. It is the most frequent cause of scrotal pain presenting to outpatient clinics and emergency departments.
Chronic epididymitis, in particular, can be challenging to manage and may account for up to 80% of patients presenting with scrotal pain in an outpatient setting, often requiring multiple visits and specialist consultations.
What Are the Symptoms of Epididymitis?
The symptoms of epididymitis can range from mild discomfort to severe pain and typically develop over a few days. Without treatment, they tend to worsen.
Key Symptoms of Acute Epididymitis
If you have acute epididymitis, you might experience one or more of the following symptoms:
- Testicle Pain and Tenderness: This is the hallmark symptom. The pain is usually on one side and often comes on gradually. It typically starts at the back of the testicle where the epididymis is located.
- Scrotal Swelling, Redness, or Warmth: The affected side of the scrotum may become swollen, appear red or discolored, and feel warm to the touch.
- Pain During Urination (Dysuria): A burning or painful sensation when you pass urine.
- Urgent or Frequent Need to Urinate: Feeling like you need to urinate more often than usual or having a sudden, strong urge to go.
- Penile Discharge: An abnormal discharge from the tip of the penis, which is a strong indicator of an STI.
- Pain or Discomfort in the Lower Abdomen or Pelvic Area: The pain can sometimes radiate from the scrotum to the lower abdomen or flank.
- Blood in the Semen (Hematospermia): This can be alarming but is a possible symptom of inflammation in the reproductive tract.
- Fever and Chills: A low-grade fever and chills can accompany the infection.
- Enlarged or Tender Lymph Nodes in the groin area.
Symptoms of Chronic Epididymitis
Chronic epididymitis presents differently.
The primary symptom is long-lasting (more than 6 weeks) pain or discomfort in the scrotum, testicle, or epididymis.
Unlike the acute form, significant swelling and redness are usually absent.
The pain can be a constant, dull ache or a sharp, intermittent pain that may worsen with activities like sitting for long periods, driving, or sexual activity.
When to Seek Emergency Medical Care
Do not ignore scrotal pain or swelling.
While epididymitis is common, some symptoms require immediate medical attention to rule out more dangerous conditions like testicular torsion (a twisted testicle), which can lead to the loss of a testicle if not treated within hours.
Seek emergency treatment immediately if you experience:
- Sudden, severe pain in the scrotum.
- Nausea and vomiting accompanying the scrotal pain.
- A testicle that is positioned higher than normal or at an unusual angle.
You should see a healthcare provider promptly if you have penile discharge or pain during urination, as these are signs of an infection that needs treatment.
Symptoms in Children and Adolescents
In children, symptoms are similar to adults and may include:
- Scrotal pain, redness, or tenderness.
- Pain or burning during urination.
- Discomfort in the lower abdomen.
- Fever.
It is crucial to have any child with scrotal pain evaluated immediately to rule out testicular torsion, which is more common in this age group than epididymitis.
What Causes Epididymitis? From Infections to Injury
The vast majority of epididymitis cases are caused by a bacterial infection.
The way the infection reaches the epididymis and the type of bacteria involved often depend on a person’s age and sexual habits.
The Pathophysiology: How Does the Infection Happen?
In most cases, epididymitis results from the retrograde ascent of pathogens.
This means that bacteria from the urethra (the tube that carries urine out of the body) or bladder travel backward through the male reproductive tract—up the vas deferens—to infect the epididymis. This can happen due to:
- Sexually Transmitted Infections: Bacteria are introduced into the urethra during sexual contact.
- Urinary Tract Infections: Bacteria already present in the bladder or prostate spread to the epididymis.
Sexually Transmitted Infections (STIs) – The Primary Cause in Younger Men
In sexually active men, especially those under 35, STIs are the most common culprits. The two main bacteria responsible are:
- Chlamydia trachomatis (causing Chlamydia)
- Neisseria gonorrhoeae (causing Gonorrhea)
These infections typically start as urethritis (inflammation of the urethra) and can be asymptomatic before spreading to the epididymis.
Non-Sexually Transmitted Infections – Common in Older Men
In men over 35, children, and men who are not sexually active, epididymitis is more often caused by enteric (intestinal) bacteria that have led to a urinary tract infection (UTI) or prostatitis (prostate infection). The most common bacterium is:
- Escherichia coli (E. coli)
These infections are often associated with underlying urinary tract issues, such as an enlarged prostate, which can cause urine to flow backward or stagnate.
Non-Infectious Causes
Not all cases of epididymitis are caused by infection. Other potential causes include:
- Chemical Epididymitis: This occurs when urine flows backward (refluxes) into the epididymis, causing irritation without an infection. It can be triggered by heavy lifting, straining, or exercising with a full bladder.
- Trauma or Injury: A direct blow or injury to the groin or scrotum can cause inflammation of the epididymis.
- Medication-Induced Epididymitis: The heart medication amiodarone is known to cause epididymal inflammation in some men. This is usually dose-dependent and resolves by lowering the dose or switching medications (under a doctor’s supervision).
Rare Causes
In some less common scenarios, epididymitis can be caused by:
- Tuberculosis (TB): In regions where TB is prevalent, it can spread to the genitourinary system and cause a granulomatous infection in the epididymis.
- Viral Infections: The mumps virus is a well-known cause of orchitis (testicle inflammation) and can sometimes cause epididymo-orchitis, especially in post-pubertal males. Other viruses like coxsackievirus have also been implicated.
- Systemic Diseases: Autoimmune conditions like Behçet’s disease or sarcoidosis can rarely manifest with epididymal inflammation.
Who is at Risk for Developing Epididymitis?
Certain behaviors, medical conditions, and anatomical factors can increase your risk of developing epididymitis. The risk factors are often divided into those related to sexually transmitted and non-sexually transmitted causes.
Risk Factors for Sexually Transmitted Epididymitis
Any sexual behavior that increases the risk of contracting an STI also increases the risk of epididymitis. These include:
- Having sex without a condom.
- Having multiple sexual partners or a partner who has multiple partners.
- A personal history of a prior STI.
- Being a young, sexually active male (under 35).
- Engaging in insertive anal intercourse, which can expose the urethra to enteric bacteria like E. coli.
Risk Factors for Non-Sexually Transmitted Epididymitis
Risk factors for epididymitis not caused by STIs are often related to the urinary system. These include:
- Age: Being older than 35 increases the risk of bladder outlet obstruction.
- Benign Prostatic Hyperplasia (BPH): An enlarged prostate can block the flow of urine from the bladder, increasing the risk of UTIs that can spread to the epididymis.
- Recent Urinary Tract Surgery or Instrumentation: Procedures involving the insertion of a scope (cystoscopy) or a urinary catheter can introduce bacteria into the urinary tract.
- Anatomical Abnormalities: Structural problems in the urinary tract, present from birth, can increase the risk, especially in children.
- Chronic or Recurrent Urinary Tract Infections (UTIs).
- Being Uncircumcised: Some studies suggest a slightly higher risk in uncircumcised males.
- A Weakened Immune System: Conditions like HIV can make a person more susceptible to various infections that could lead to epididymitis.
How is Epididymitis Diagnosed?
Diagnosing epididymitis involves a combination of a physical examination, a review of your medical history, and laboratory or imaging tests.
A key goal of the evaluation is to distinguish epididymitis from testicular torsion, a surgical emergency.
The Physical Examination: What to Expect
A healthcare provider will perform a thorough physical exam, which includes:
- Scrotal Examination: The provider will gently examine your scrotum for swelling, tenderness, redness, and warmth. They will palpate the epididymis (at the back of the testicle) to check for tenderness and induration (hardening).
- Prehn’s Sign: The provider may gently lift the affected scrotum. If the pain is relieved by elevation, it is a positive Prehn’s sign, which is suggestive of epididymitis. If the pain worsens or does not change, it may suggest testicular torsion. However, this sign is not completely reliable.
- Cremasteric Reflex: The provider may stroke or pinch the inner thigh. A normal response is the elevation of the testicle on that side. This reflex is typically present in epididymitis but is often absent in cases of testicular torsion.
- Abdominal and Groin Exam: To check for hernias or tender lymph nodes.
- Digital Rectal Exam (DRE): To check the prostate for tenderness or enlargement, which could suggest prostatitis as a related cause.
Laboratory Tests: Uncovering the Cause
Lab tests are essential for identifying the underlying cause, especially if an infection is suspected.
- Urinalysis and Urine Culture: A urine sample will be tested for signs of infection, such as white blood cells (pyuria) and bacteria. A culture can identify the specific bacteria causing a UTI and determine which antibiotics will be effective.
- STI Testing: If an STI is suspected, a urine sample or a swab from the urethra will be collected for a Nucleic Acid Amplification Test (NAAT). This is a highly sensitive test for detecting Chlamydia trachomatis and Neisseria gonorrhoeae.
- Blood Tests: A complete blood count (CBC) may show an elevated white blood cell count, indicating an infection. Inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) may also be elevated.
Imaging Tests: Ruling Out Other Conditions
Imaging is not always necessary but is crucial when the diagnosis is uncertain or to rule out testicular torsion.
- Color Doppler Ultrasound: This is the preferred imaging test for acute scrotal pain. It uses sound waves to create images of the testicles and surrounding tissues and can also assess blood flow.
- In epididymitis, the ultrasound typically shows an enlarged, inflamed epididymis with increased blood flow (hyperemia).
- In testicular torsion, it will show decreased or absent blood flow to the affected testicle.
- Other Scans: Radionuclide scanning is highly accurate but less commonly used due to its limited availability. CT scans are generally not used for initial diagnosis but may be helpful if an abdominal or pelvic source of pain is suspected.
Differentiating Epididymitis from Testicular Torsion
Distinguishing between these two conditions is the most critical part of the diagnostic process. Here is a summary of the key differences:
| Feature | Epididymitis | Testicular Torsion |
|---|---|---|
| Onset of Pain | Gradual (over days) | Sudden and severe (over hours) |
| Associated Symptoms | Fever, urinary symptoms (pain, frequency), penile discharge are common. | Nausea and vomiting are common, fever and urinary symptoms are rare. |
| Cremasteric Reflex | Usually present | Usually absent |
| Prehn’s Sign | Pain may be relieved by scrotal elevation. | Pain is not relieved (or worsens) with elevation. |
| Ultrasound Finding | Increased blood flow to the epididymis. | Decreased or absent blood flow to the testicle. |
What is the Most Effective Epididymitis Treatment?
Treatment for epididymitis focuses on eradicating the underlying infection, relieving symptoms, and preventing complications.
The approach depends on the cause and severity of the condition.
Immediate Supportive Care at Home
Regardless of the cause, supportive measures are key to managing pain and inflammation. These can be started immediately:
- Bed Rest: Rest for 1-2 days, especially in the early stages.
- Scrotal Elevation: Lie down and elevate your scrotum on a rolled-up towel. This helps improve drainage and reduce swelling.
- Ice Packs: Apply cold packs wrapped in a cloth to the scrotum for 15-20 minutes at a time, several times a day. This helps reduce inflammation and numb the pain.
- Scrotal Support: Wearing an athletic supporter (jockstrap) can provide support and relieve discomfort when you are standing or walking.
- Avoid Heavy Lifting: Refrain from straining or heavy lifting until you have fully recovered.
Antibiotic Therapy: The Core of Treatment
Since most cases of acute epididymitis are bacterial, antibiotics are the primary treatment.
The choice of antibiotic is based on the most likely causative organism, which is determined by your age and sexual history.
Treatment is often started presumptively, before test results are back.
According to the 2024 European Guideline on Epididymo-orchitis and CDC recommendations, antibiotic regimens are tailored to the suspected pathogen.
| Patient Group / Likely Cause | Recommended Antibiotic Regimen | Duration |
|---|---|---|
| Likely caused by STIs (Chlamydia/Gonorrhea) (e.g., sexually active men <35) | Ceftriaxone 500 mg* (or 1 g per 2024 EU guideline) as a single intramuscular (IM) injection PLUS Doxycycline 100 mg orally twice a day | 10 days for Doxycycline |
| Likely caused by STIs AND Enteric Organisms (e.g., men who practice insertive anal sex) | Ceftriaxone 500 mg* (or 1 g) as a single IM injection PLUS Levofloxacin 500 mg orally once a day | 10 days for Levofloxacin |
| Likely caused by Enteric Organisms ONLY (e.g., men >35 with BPH, recent urologic surgery) | Levofloxacin 500 mg orally once a day OR Ofloxacin 300 mg orally twice a day | 10 days |
*Note: For persons weighing ≥150 kg (330 lbs), a 1 g dose of ceftriaxone is recommended by the CDC. Always follow your doctor’s specific prescription.
It is crucial to complete the entire course of antibiotics, even if you start to feel better, to ensure the infection is fully cleared and to prevent recurrence or complications.
Pain Management
In addition to supportive care, pain can be managed with:
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Over-the-counter medications like ibuprofen (Advil, Motrin) or naproxen (Aleve) can help reduce both pain and inflammation.
- Prescription Pain Relievers: For severe pain, your doctor may prescribe stronger pain medication.
Treating Chronic Epididymitis: A Multifaceted Approach
Managing chronic epididymitis is more complex, as an active infection is often not the cause. Treatment may involve:
- A longer course of antibiotics (4-6 weeks) to rule out a persistent, low-grade infection.
- NSAIDs for inflammation.
- Nerve pain medications, such as gabapentin or amitriptyline.
- Physical therapy for pelvic floor muscle dysfunction.
- In rare, refractory cases, referral to a pain management specialist or consideration of surgery.
When is Hospitalization Necessary?
Most men can be treated on an outpatient basis. However, hospitalization may be required if you have:
- Severe pain that cannot be managed at home.
- Signs of a systemic infection, such as high fever or sepsis.
- An abscess that needs to be drained.
- Inability to take oral antibiotics (e.g., due to vomiting).
- Uncertainty in the diagnosis, where testicular torsion cannot be definitively ruled out.
Surgical Interventions
Surgery is rarely needed for epididymitis but may be considered in specific situations:
- Abscess Drainage: If a collection of pus (an abscess) forms, it may need to be drained with a needle or through a surgical incision.
- Epididymectomy: In severe cases of chronic, debilitating pain that do not respond to any other treatments, the surgical removal of the epididymis may be an option. This is considered a last resort.
What is the Recovery and Prognosis for Epididymitis?
With prompt and appropriate treatment, the prognosis for acute epididymitis is excellent.
However, recovery takes time, and it’s important to follow your doctor’s instructions carefully.
Recovery Timeline: What to Expect Week by Week
- First 72 Hours: You should start to notice an improvement in pain and fever within 2 to 3 days of starting antibiotics. If your symptoms do not improve or worsen, you must contact your healthcare provider immediately.
- Week 1-2: The most severe pain and swelling should have subsided significantly. You may still feel some tenderness and discomfort.
- Several Weeks to Months: While the infection clears up relatively quickly, the residual tenderness, induration (hardness), and swelling of the epididymis can take several weeks or even a couple of months to resolve completely. This is normal.
The Importance of Follow-Up Care
A follow-up visit with your doctor is important to ensure the infection has been completely cured.
This is especially true if your symptoms persist.
For sexually transmitted epididymitis, it’s also vital to ensure your sexual partners have been treated to prevent reinfection.
If you were treated for STI-related epididymitis, you and your partner(s) should abstain from sexual intercourse until you have both completed treatment and your symptoms have fully resolved.
Long-Term Outlook and Potential for Recurrence
Most men recover from acute epididymitis with no long-term problems. However, recurrence is possible, especially if the initial infection was not fully treated or if underlying risk factors (like BPH or recurrent UTIs) are not addressed.
In a small number of cases, acute epididymitis can transition into chronic epididymitis, leading to long-term pain.
What Are the Potential Complications of Untreated Epididymitis?
Delaying treatment for epididymitis can lead to serious and sometimes permanent complications. This is why seeking timely medical care is so important.
Abscess Formation (Scrotal or Testicular)
An untreated infection can lead to the formation of a pus-filled pocket called an abscess in the epididymis or testicle.
An abscess causes severe pain and swelling and usually requires surgical drainage.
Reduced Fertility or Sterility
Inflammation can cause scarring and blockage of the epididymis, which is the tube sperm must travel through.
If this happens on both sides (bilateral epididymitis), it can lead to infertility.
While this is a rare complication of a single episode, the risk increases with recurrent infections.
Testicular Atrophy (Shrinkage)
Severe or prolonged inflammation, especially in cases of epididymo-orchitis, can damage the testicle and disrupt its blood supply.
This can cause the testicle to shrink (atrophy) and may impair its ability to produce sperm and testosterone.
Sepsis (A Life-Threatening Complication)
In rare, severe cases, the infection can spread from the scrotum into the bloodstream, leading to sepsis.
Sepsis is a life-threatening medical emergency that causes a body-wide inflammatory response and can lead to organ failure.
Chronic Pain
One of the most common complications is the development of chronic epididymitis or chronic scrotal pain (orchialgia).
This can be a debilitating condition that significantly impacts quality of life.
How Can Epididymitis Be Prevented?
While not all cases of epididymitis can be prevented, you can take steps to significantly reduce your risk, particularly for infection-related causes.
Practicing Safer Sex
To protect against STIs that cause epididymitis:
- Use Condoms: Consistently and correctly use condoms during any sexual activity.
- Limit Sexual Partners: Reducing your number of sexual partners lowers your risk of exposure to STIs.
- Get Regular STI Screenings: If you are sexually active, especially with new or multiple partners, get tested regularly for STIs.
Managing Urinary Health
To prevent epididymitis caused by urinary pathogens:
- Treat UTIs Promptly: Seek treatment for any symptoms of a urinary tract infection.
- Manage Prostate Issues: If you have an enlarged prostate (BPH), work with your urologist to manage the condition and ensure good bladder emptying.
- Stay Hydrated: Drinking plenty of water helps flush bacteria from your urinary system.
- Don’t “Hold It”: Urinate when you feel the urge and try to empty your bladder completely.
Other Preventive Measures
- Mumps Vaccination: The MMR (measles, mumps, rubella) vaccine effectively prevents mumps, a viral cause of epididymo-orchitis.
- Groin Protection: Wear appropriate protective gear during contact sports to prevent trauma.
Frequently Asked Questions (FAQ) about Epididymitis
1. Can epididymitis go away on its own?
No, bacterial epididymitis will not go away on its own and requires antibiotic treatment. Delaying treatment can lead to serious complications. Non-infectious chemical epididymitis may resolve with rest and anti-inflammatory measures, but a medical diagnosis is essential to rule out infection.
2. Is epididymitis contagious?
The condition itself is not contagious. However, if it is caused by an STI like chlamydia or gonorrhea, the underlying infection can be passed to a sexual partner. It is crucial for both you and your partners to be treated.
3. How long does it take for epididymitis to heal?
Pain and fever typically improve within 2-3 days of starting antibiotics. However, the swelling and tenderness in the scrotum can take several weeks or even a few months to completely disappear. It’s important to be patient with the healing process.
4. Can I exercise with epididymitis?
You should avoid strenuous exercise, heavy lifting, and activities that put pressure on the groin area (like cycling) until you are fully recovered. Gentle walking is usually fine, but listen to your body and rest as needed.
5. Does ejaculating help or hurt epididymitis?
Ejaculation is unlikely to make the condition worse, but it can be painful during an acute infection. It’s best to abstain from sexual activity, including masturbation, until you have completed your treatment and your doctor says it is safe to resume.
6. Can stress cause epididymitis?
Stress itself does not directly cause epididymitis. However, stress can lead to unconscious tensing of pelvic floor muscles, which could potentially contribute to pain syndromes or exacerbate symptoms in chronic epididymitis. It is not a cause of acute infectious epididymitis.
7. Is epididymitis a sign of cancer?
Epididymitis is not a sign of cancer. However, testicular cancer can sometimes present with a lump or pain, so it is a critical part of the differential diagnosis. If a lump persists after treatment, your doctor will investigate further to rule out cancer.
8. What’s the difference between epididymitis and orchitis?
Epididymitis is inflammation of the epididymis (the tube at the back of the testicle). Orchitis is inflammation of the testicle itself. When both are inflamed, it is called epididymo-orchitis. Epididymitis is much more common than isolated orchitis.
9. Can I get epididymitis if I’m not sexually active?
Yes. While STIs are a common cause in younger men, epididymitis in older men, children, and those not sexually active is often caused by bacteria from a urinary tract infection (UTI) or non-infectious issues like chemical irritation or trauma.
Conclusion
Epididymitis is a common and painful condition, but with a clear understanding and prompt medical care, it is highly treatable.
The key takeaways are to never ignore scrotal pain, seek immediate help for sudden or severe symptoms to rule out testicular torsion, and always complete the full course of prescribed antibiotics.
By practicing safer sex and managing urinary health, you can significantly reduce your risk.
If you are experiencing symptoms, the best course of action is to consult a healthcare provider for an accurate diagnosis and a personalized treatment plan.
Taking control of your health is the first and most important step toward a full recovery.
We hope this guide has provided you with valuable and authoritative information. If you found this article helpful, please consider sharing it with others who might benefit.
Do you have a personal experience with epididymitis or a question we didn’t cover? Leave a comment below to engage with our community.

