Neuropathy is nerve damage that disrupts the intricate communication network between your brain, spinal cord, and the rest of your body.
This condition affects millions of people, with recent studies indicating a global prevalence of around 14.6%, a figure that rises significantly with age.
It can manifest as tingling, pain, numbness, or weakness, profoundly impacting one’s quality of life.
Understanding the specific type of neuropathy you have is the first and most critical step toward effective management and treatment.
This comprehensive guide will explore the vast landscape of neuropathy, breaking down its complex classifications, diverse causes, and varied symptoms.
We will delve into the diagnostic process, outline current and emerging treatment options, and provide practical advice for living with the condition.
By the end, you will have a clear, authoritative understanding of neuropathy in all its forms.
In This Article
What is Neuropathy? A Deep Dive into the Nervous System
At its core, neuropathy is a disease or dysfunction of one or more nerves.
To grasp what this means, it’s essential to understand the system it affects: the peripheral nervous system.
Understanding the Peripheral Nervous System
Your nervous system has two main parts. The central nervous system (CNS) is the command center, consisting of the brain and spinal cord.
The peripheral nervous system (PNS) is the vast network of nerves that branch out from the CNS, connecting it to your limbs, organs and skin.
Think of the CNS as the power plant and the PNS as the electrical grid that delivers power to every house in the city.
This grid is made of nerve cells called neurons, which have long, wire-like extensions called axons.
Many axons are wrapped in a fatty, insulating layer called the myelin sheath, which helps signals travel quickly and efficiently.
Neuropathy occurs when these nerve cells, their axons, or their myelin sheaths are damaged.
How Nerve Damage Disrupts Communication
According to the National Institute of Neurological Disorders and Stroke (NINDS), nerve damage disrupts signaling in three primary ways:
- Loss of signals: Like a cut wire, the nerve fails to send signals, leading to numbness or muscle weakness.
- Inappropriate signaling: The damaged nerve sends signals when it shouldn’t, causing tingling, burning or phantom pain.
- Signal distortion: The nerve alters the messages it sends, like a radio station with static, leading to confusing sensations or poor coordination.
How is Neuropathy Classified?
With over 100 identified types, neuropathy is not a single condition but a spectrum of disorders.
To make sense of them, doctors use several classification systems.
Classification by Nerve Type: Sensory, Motor and Autonomic
The PNS contains three main types of nerves, and neuropathy symptoms depend on which ones are affected.
- Sensory Nerves: These transmit information from your skin and muscles to your brain, such as touch, temperature, vibration, and pain. Damage can cause tingling, numbness, burning pain, or an inability to feel temperature changes.
- Motor Nerves: These carry signals from your brain to your muscles, controlling voluntary movement. Damage can lead to muscle weakness, cramps, twitching (fasciculations) and loss of muscle mass (atrophy).
- Autonomic Nerves: These control involuntary bodily functions like heart rate, blood pressure, digestion, sweating and bladder function. Damage can cause dizziness upon standing, excessive or reduced sweating, digestive issues and bladder problems.
Most people have a mixed neuropathy, affecting two or all three nerve types to varying degrees.
Classification by Nerve Fiber Size: Small vs. Large Fiber
Nerve fibers also come in different sizes, and this distinction is crucial for diagnosis and treatment.
- Large Fiber Neuropathy: Affects the larger, myelinated nerve fibers responsible for vibration sense, light touch and muscle control (proprioception). Symptoms include loss of balance (especially with eyes closed), weakness and diminished reflexes. Standard nerve tests like EMG/NCS are effective at detecting this type.
- Small Fiber Neuropathy: Affects the small, thinly myelinated or unmyelinated fibers that transmit pain and temperature sensations. As detailed in a StatPearls review, classic symptoms include burning pain, pins-and-needles and sensitivity to touch, often starting in the feet. Standard nerve tests may be normal, requiring specialized tests like a skin biopsy.
Classification by Distribution: Mononeuropathy vs. Polyneuropathy
Neuropathy can also be described by how many nerves are affected and where.
- Mononeuropathy: Damage to a single peripheral nerve. A classic example is Carpal Tunnel Syndrome, where the median nerve in the wrist is compressed.
- Multiple Mononeuropathy: Damage to two or more separate nerves in different parts of the body.
- Polyneuropathy: Widespread, simultaneous damage to many peripheral nerves throughout the body. This is the most common pattern, often starting in the feet and hands and progressing inward in a “stocking-glove” distribution.
What are the Major Types of Acquired Neuropathy?
Acquired neuropathies develop after birth due to disease, injury or exposure to toxins.
They are far more common than inherited forms.
Peripheral Neuropathy: The Most Common Form
Peripheral neuropathy is an umbrella term for damage to any nerves of the peripheral nervous system.
As the Cleveland Clinic explains, it’s the most common form and is often used interchangeably with “neuropathy”.
Most of the conditions discussed in this guide fall under this category.
Diabetic Neuropathy: A Leading Cause Worldwide
Diabetes is the single most common cause of neuropathy.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), about half of all people with diabetes will develop some form of nerve damage.
High blood sugar injures nerve fibers over time. There are several types:
- Peripheral Diabetic Neuropathy: The most common type, affecting the feet and legs first, followed by the hands and arms.
- Autonomic Diabetic Neuropathy: Affects nerves controlling internal organs, leading to issues with heart rate, blood pressure, digestion (gastroparesis) and bladder control.
- Proximal Neuropathy (Diabetic Amyotrophy): Affects nerves in the thighs, hips, or buttocks, typically on one side, causing severe pain and muscle weakness.
- Focal Neuropathy (Mononeuropathy): Damage to a single, specific nerve, often causing sudden weakness or pain in the hand, head, torso or leg.
Autoimmune Neuropathies: When the Body Attacks Itself
In these conditions, the body’s immune system mistakenly attacks its own nerve tissues.
- Guillain-Barré Syndrome (GBS): A rare, acute disorder where the immune system attacks the myelin sheath of peripheral nerves. It often follows a viral or bacterial infection and causes rapidly progressing weakness and tingling, usually starting in the legs and moving up. It is a medical emergency that can lead to total paralysis.
- Chronic Inflammatory Demyelinating Polyneuropathy (CIDP): Often considered the chronic counterpart to GBS, CIDP involves a slower, progressive or relapsing-remitting course of weakness and sensory loss over two months or more. Treatment often involves immunosuppressive therapies.
Chemotherapy-Induced Peripheral Neuropathy (CIPN)
A common and debilitating side effect of certain cancer treatments, particularly platinum-based drugs, taxanes and vinca alkaloids.
CIPN causes pain, numbness, and tingling in the hands and feet.
A 2022 review in Frontiers in Pharmacology highlights that the antidepressant duloxetine is the only medication with strong evidence to support its use for managing painful CIPN.
Autonomic Neuropathy: The “Invisible” Condition
This type specifically targets the autonomic nerves. While diabetes is a major cause, it can also result from other conditions.
As the Mayo Clinic notes, symptoms can be wide-ranging, including dizziness, inability to regulate body temperature, digestive problems and sexual dysfunction.
What About Inherited and Cranial Neuropathies?
Hereditary Neuropathies: The Genetic Link
These are caused by genetic mutations passed down through families.
While rarer than acquired forms, they can be severe.
- Charcot-Marie-Tooth Disease (CMT): The most common inherited neurological disorder. According to a GeneReviews summary, CMT is a group of disorders affecting both motor and sensory nerves. It typically causes muscle weakness and atrophy in the lower legs and feet, leading to high arches (pes cavus) and foot drop.
Cranial Neuropathies: Affecting the Head and Face
These involve damage to one of the 12 pairs of cranial nerves that emerge directly from the brain.
- Trigeminal Neuropathy: Affects the fifth cranial nerve, causing facial numbness, tingling or a continuous burning pain. It is distinct from trigeminal neuralgia, which causes sharp, stabbing pain attacks. A StatPearls article emphasizes that this condition can be a sign of an underlying tumor or autoimmune disease.
- Bell’s Palsy: A temporary paralysis or weakness of the muscles on one side of the face, caused by inflammation or damage to the seventh cranial nerve (the facial nerve).
What are the Common Symptoms of Neuropathy?
Symptoms are highly variable and depend on the type and location of the damaged nerves.
The table below summarizes common symptoms based on the primary nerve type affected.
| Nerve Type | Common Symptoms | Functional Impact |
|---|---|---|
| Sensory | Numbness, tingling (“pins and needles”), burning or sharp pain, extreme sensitivity to touch (allodynia), loss of ability to feel temperature or pain. | Difficulty with fine motor tasks (buttoning a shirt), risk of unnoticed injuries (burns, cuts), chronic pain, sleep disruption. |
| Motor | Muscle weakness, loss of coordination, frequent falling, painful cramps, muscle twitching (fasciculations), muscle atrophy (shrinking). | Difficulty walking or climbing stairs, trouble with grip strength, foot drop (inability to lift the front part of the foot). |
| Autonomic | Dizziness or fainting upon standing (orthostatic hypotension), excessive or no sweating, heat intolerance, digestive issues (bloating, constipation, diarrhea), bladder problems, sexual dysfunction. | Inability to regulate blood pressure, risk of dehydration or heat stroke, unpredictable digestive and bladder function. |
What Causes Neuropathy and Who is at Risk?
Neuropathy can stem from a wide array of causes, though in some cases, no specific cause can be identified (idiopathic neuropathy).
- Systemic Diseases: Diabetes is the number one cause. Others include kidney disease, liver disorders, hormonal imbalances (like hypothyroidism) and certain cancers.
- Physical Trauma: Injuries from accidents, falls, or repetitive stress can compress, crush or sever nerves.
- Infections: Viruses and bacteria can directly attack nerves. Examples include shingles (varicella-zoster virus), Lyme disease, HIV and Hepatitis C.
- Autoimmune Diseases: Lupus, rheumatoid arthritis, and Sjögren’s syndrome can all lead to neuropathy.
- Vitamin Deficiencies: Lack of B vitamins (especially B12, B6, and B1), vitamin E, and copper are crucial for nerve health. Conversely, an excess of vitamin B6 can also be toxic to nerves.
- Toxins and Medications: Exposure to heavy metals (lead, mercury), industrial chemicals, and certain medications (especially chemotherapy) are well-known causes. Chronic alcohol abuse is also a major contributor.
- Genetics: Inherited conditions like Charcot-Marie-Tooth disease.
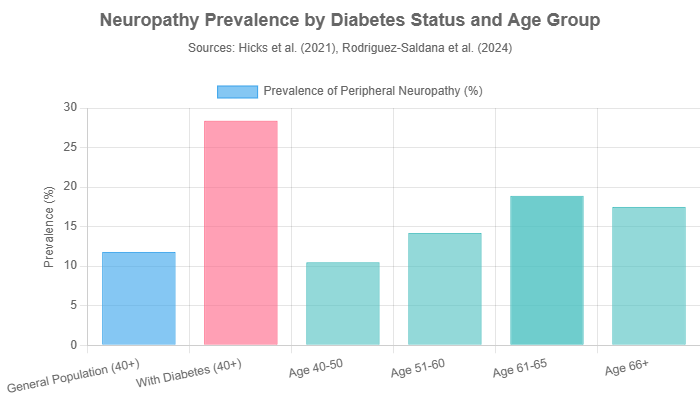
The risk of developing neuropathy increases with age. As the chart below illustrates, based on recent epidemiological data, prevalence rises steadily in older populations and is significantly higher in individuals with diabetes.
How is Neuropathy Diagnosed?
Diagnosing neuropathy can be complex due to the wide variety of symptoms and causes.
The process is a form of medical detective work.
The Diagnostic Process: From History to Physical Exam
A doctor will typically start with:
- A detailed medical history: Questions about your symptoms, lifestyle, alcohol use, exposure to toxins, family history of neurological disease and other medical conditions.
- A physical and neurological exam: The doctor will check your reflexes, muscle strength and tone, ability to feel different sensations (light touch, vibration, temperature) and your coordination and balance.
Advanced Diagnostic Tests
If neuropathy is suspected, further tests are used to confirm the diagnosis and identify the cause.
- Blood Tests: Can detect vitamin deficiencies, diabetes, abnormal immune function, kidney or liver problems and other underlying conditions.
- Nerve Conduction Studies (NCS) and Electromyography (EMG): These tests measure the electrical activity of your nerves and muscles. An NCS assesses the speed and strength of signals in large nerve fibers, while an EMG records electrical activity in muscles to differentiate between nerve and muscle disorders.
- Skin Biopsy: The gold standard for diagnosing small fiber neuropathy. A tiny piece of skin is removed (usually from the lower leg) and examined under a microscope to count the density of nerve fiber endings.
- Autonomic Testing: A series of tests that evaluate how your autonomic nerves are functioning, such as tests that measure sweating (QSART), heart rate, and blood pressure responses.
- Imaging Tests: MRI or CT scans may be used to look for tumors, herniated discs, or other structural problems that could be pressing on nerves.
What are the Treatment Options for Neuropathy?
There is no one-size-fits-all treatment for neuropathy.
The approach depends entirely on the underlying cause and the specific symptoms.
Treating the Underlying Cause
The most important step is to address the root cause of the nerve damage. This might include:
- Controlling blood sugar in people with diabetes.
- Correcting vitamin deficiencies with supplements.
- Treating infections with appropriate medications.
- Managing autoimmune diseases with immunosuppressive drugs.
- Stopping alcohol consumption or exposure to toxins.
In some cases, when the underlying cause is treated, nerves can slowly recover and regenerate.
Managing Symptoms: Pain Relief and Medication
For many, managing symptoms, especially chronic pain, is a primary goal.
Standard pain relievers are often ineffective. Instead, doctors use:
- Antidepressants: Certain tricyclic antidepressants (like amitriptyline) and serotonin-norepinephrine reuptake inhibitors (SNRIs like duloxetine and venlafaxine) can relieve neuropathic pain.
- Anti-seizure Medications: Drugs developed to treat epilepsy, such as gabapentin and pregabalin, are frequently prescribed to reduce nerve pain.
- Topical Treatments: Creams or patches containing lidocaine or capsaicin can provide localized relief for some people.
Therapies and Interventions
- Physical Therapy: Can help improve strength, balance, and mobility, reducing the risk of falls.
- Transcutaneous Electrical Nerve Stimulation (TENS): A device that delivers a gentle electric current to the skin, which may help disrupt pain signals.
- Intravenous Immunoglobulin (IVIg) and Plasma Exchange: These treatments are used for autoimmune neuropathies like GBS and CIDP to remove or neutralize the harmful antibodies attacking the nerves.
Can Neuropathy Be Prevented?
Prevention focuses on managing risk factors.
The most effective strategy is to manage underlying medical conditions that can lead to neuropathy. This includes:
- Strict blood sugar control for individuals with diabetes.
- Eating a balanced diet rich in fruits, vegetables, whole grains, and lean protein to prevent vitamin deficiencies.
- Regular exercise to improve circulation and overall health.
- Avoiding excessive alcohol consumption.
- Protecting yourself from injuries and avoiding repetitive motions that put pressure on nerves.
Living with Neuropathy: Practical Tips and Strategies
Living with chronic neuropathy requires adaptation and proactive self-care.
- Foot Care is Critical: If you have numbness in your feet, inspect them daily for cuts, blisters, or sores you might not feel. Wear well-fitting, protective shoes.
- Home Safety: Remove tripping hazards like loose rugs, ensure good lighting, and install handrails in bathrooms and stairways to prevent falls.
- Temperature Awareness: Be cautious with hot water, as you may not be able to accurately judge temperature, increasing the risk of burns.
- Seek Support: Connect with support groups, either online or in person. Sharing experiences with others who understand can be incredibly valuable for mental and emotional well-being.
Frequently Asked Questions (FAQ) about Neuropathy
1. Can neuropathy be cured?
It depends on the cause. If the neuropathy is caused by a treatable condition like a vitamin deficiency or nerve compression, it can sometimes be reversed. For many chronic forms, like diabetic neuropathy, the focus is on managing symptoms and preventing further progression, not a complete cure.
2. Is neuropathy a fatal condition?
Most types of neuropathy are not fatal. However, severe cases, such as Guillain-Barré Syndrome which can affect breathing muscles, or autonomic neuropathy affecting heart function, can be life-threatening if not managed properly.
3. What is the difference between neuropathy and neuralgia?
Neuropathy is a general term for nerve damage or disease. Neuralgia specifically refers to severe, sharp, shock-like pain that follows the path of a nerve, often without other signs of nerve damage like numbness or weakness.
4. Does exercise help with neuropathy?
Yes, regular, moderate exercise is highly recommended. It can improve blood flow to the nerves, reduce pain, improve muscle strength, and enhance balance, which helps prevent falls.
5. Are there specific foods I should eat or avoid for neuropathy?
A balanced diet rich in B vitamins, antioxidants (from fruits and vegetables), and healthy fats is beneficial. It’s crucial to limit sugar and processed foods, especially for diabetic neuropathy and to avoid excessive alcohol.
6. Why is my neuropathy pain worse at night?
Many people experience this. The exact reason isn’t fully understood, but it may be due to fewer distractions at night, changes in body temperature, or hormonal fluctuations during the sleep cycle that can make you more sensitive to pain signals.
7. Can stress make neuropathy worse?
Yes, emotional and physical stress can exacerbate neuropathy symptoms. Stress can increase inflammation and make the body more sensitive to pain. Stress management techniques like meditation, yoga, and deep breathing can be helpful.
8. What is idiopathic neuropathy?
Idiopathic neuropathy means that after extensive testing, a specific cause for the nerve damage cannot be found. This accounts for a significant number of cases, particularly in older adults.
Conclusion
Neuropathy is a complex and multifaceted condition, but it is not an insurmountable one.
From the tingling in your toes caused by small fiber damage to the sudden weakness of a cranial neuropathy, understanding the specific nature of your nerve issue is the cornerstone of effective management.
Advances in diagnostics are making it easier to pinpoint the type and cause, while a growing arsenal of treatments offers hope for symptom relief and improved function.
If you are experiencing any symptoms of neuropathy, the most important action you can take is to consult a healthcare professional.
An early and accurate diagnosis opens the door to treatments that can slow progression, manage pain, and preserve your quality of life.
By arming yourself with knowledge and working closely with your medical team, you can navigate the challenges of neuropathy and continue to lead a full and active life.
Reference
[1] https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/symptoms-causes/syc-20352061
[2] https://www.ninds.nih.gov/health-information/disorders/peripheral-neuropathy
[3] https://my.clevelandclinic.org/health/diseases/14737-neuropathy

