Type 2 diabetes is a chronic metabolic condition characterized by the body’s inability to effectively use insulin, leading to high levels of glucose (sugar) in the blood.
This happens because the body’s cells either resist the effects of insulin—a hormone essential for energy regulation—or the pancreas doesn’t produce enough insulin to maintain normal glucose levels.
The scale of this health challenge is staggering. According to the Centers for Disease Control and Prevention (CDC), over 38 million Americans have diabetes, and an overwhelming 90-95% of them have type 2 diabetes.
Even more alarming, an estimated 97.6 million U.S. adults—more than 1 in 3—have prediabetes, a serious health condition where blood sugar levels are higher than normal, but not yet high enough to be diagnosed as type 2 diabetes.
This places a vast portion of the population on a direct path toward developing the full-blown disease.
But a diagnosis is not a destiny. Understanding this condition is the first and most powerful step toward taking control.
This guide is designed to be your definitive resource, moving beyond the basic definition to explore its intricate causes, often-hidden symptoms, and the full spectrum of its impact on the body.
We will delve into how it’s diagnosed, its far-reaching complications, and most importantly, provide a deep dive into the evidence-based strategies for effective management, prevention, and even remission.
Continue reading to empower yourself with the knowledge needed to navigate your health journey with confidence.
In This Article
Part 2: What Is Type 2 Diabetes and How Does It Develop?
To truly grasp type 2 diabetes, we must look inside the body at the intricate dance between glucose and insulin.
This condition doesn’t appear overnight, it’s the result of a progressive breakdown in a fundamental metabolic process that keeps our bodies fueled and functioning.
What Exactly Happens in the Body with Type 2 Diabetes?
At its core, type 2 diabetes is a story of cellular communication gone wrong. It involves two main characters: glucose and insulin.
The Role of Glucose and Insulin
Think of your body as a bustling city and your cells as the homes and businesses that need power to operate.
Glucose, a simple sugar derived from the carbohydrates you eat, is the primary fuel source—the electricity—for this city.
After you eat, glucose enters your bloodstream, ready to be delivered where it’s needed.
However, glucose can’t just enter the cells on its own. It needs a key. That key is insulin, a hormone produced by the beta cells in your pancreas.
When your blood sugar rises after a meal, your pancreas releases insulin into the bloodstream.
Insulin travels to your cells and attaches to receptors on their surface, effectively “unlocking the door” to allow glucose to enter and be used for energy.
This process lowers the amount of glucose in your blood, keeping it in a healthy range.
The “Twin Problems”: Insulin Resistance and Insulin Deficiency
In type 2 diabetes, this elegant system breaks down due to two interconnected issues, often referred to as the “twin problems”:
- Insulin Resistance: This is typically the first problem to arise. For reasons often linked to genetics, excess body weight (especially around the abdomen), and physical inactivity, the body’s cells—particularly in the muscle, fat, and liver—stop responding properly to insulin’s signal. It’s as if the locks on the cell doors have become rusty. The key (insulin) is there, but it can’t open the door efficiently. As a result, glucose has trouble entering the cells and starts to build up in the bloodstream.
- Relative Insulin Deficiency: In the early stages of insulin resistance, the pancreas works overtime, pumping out more and more insulin to force the stubborn cells to take in glucose. For a while, this compensation works, and blood sugar levels may remain normal. However, over years, the hardworking beta cells in the pancreas can become exhausted and damaged. They gradually lose their ability to produce enough insulin to overcome the resistance. This isn’t a complete absence of insulin (as seen in type 1 diabetes), but a relative deficiency—the supply of insulin can no longer meet the body’s heightened demand.
This combination of insulin resistance and declining insulin production creates a vicious cycle.
High blood sugar (hyperglycemia) further damages the pancreas and worsens insulin resistance, causing blood sugar levels to climb even higher.
If left unmanaged, this chronic high blood sugar is what leads to the serious long-term complications of the disease.
How is Type 2 Diabetes Different from Type 1 and Gestational Diabetes?
While all forms of diabetes involve high blood sugar, their underlying causes and typical onset are distinct.
Understanding these differences is crucial for proper diagnosis and management. The following table provides a clear comparison.
| Feature | Type 1 Diabetes | Type 2 Diabetes | Gestational Diabetes |
|---|---|---|---|
| Primary Cause | Autoimmune disease. The body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. | Insulin resistance and relative insulin deficiency. A combination of genetic and lifestyle factors (like obesity and inactivity). | Hormonal changes during pregnancy cause insulin resistance. The pancreas cannot produce enough extra insulin to compensate. |
| Insulin Production | Little to no insulin is produced. | The pancreas produces insulin, but the body doesn’t use it effectively. Production may decrease over time. | Insulin production is insufficient to overcome the insulin resistance of pregnancy. |
| Typical Onset | Often diagnosed in childhood, adolescence, or young adulthood, but can occur at any age. Onset is usually rapid. | Most often diagnosed in adults over 45, but increasingly seen in younger adults, teens, and children. Onset is gradual. | Occurs during pregnancy (usually diagnosed between 24-28 weeks) and typically resolves after delivery. |
| Primary Treatment | Mandatory insulin therapy (via injections or an insulin pump) for life. | Lifestyle management (diet, exercise, weight loss) is foundational. May require oral medications and/or injectable medications, including insulin. | Lifestyle management (diet, exercise). Sometimes requires medication (like metformin or insulin) to control blood sugar during pregnancy. |
| Prevention | Currently cannot be prevented. | Can often be prevented or delayed with healthy lifestyle changes. | Risk can be reduced by achieving a healthy weight before pregnancy and staying active. |
Part 3: Causes and Who Is at Risk?
Type 2 diabetes is not caused by a single factor but rather a complex tapestry woven from threads of genetics, lifestyle choices, and environmental influences.
While some people are genetically more susceptible, it is often the interaction with modifiable lifestyle factors that “activates” the disease.
What Are the Main Causes of Type 2 Diabetes?
The development of type 2 diabetes is a multifactorial process.
It’s rarely a case of “one thing” but rather a convergence of influences that disrupt the body’s glucose management system over time.
The Interplay of Genetics and Lifestyle
Genetics play a significant role. If you have a parent or sibling with type 2 diabetes, your risk is substantially higher.
Researchers have identified numerous gene variants that can increase a person’s susceptibility.
However, having a genetic predisposition does not guarantee you will develop the disease.
As the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) explains, lifestyle acts as a powerful modulator of this genetic risk.
An unhealthy lifestyle can trigger the disease in someone who is genetically vulnerable, while a healthy lifestyle can often keep it at bay.
Key Lifestyle Drivers
Three lifestyle factors are the primary drivers behind the global rise of type 2 diabetes:
- Overweight and Obesity: This is the single most important predictor of type 2 diabetes. Excess body fat, particularly visceral fat that accumulates around the abdominal organs, releases inflammatory chemicals and fatty acids that directly interfere with insulin signaling, promoting insulin resistance.
- Physical Inactivity: Muscle is a major site for glucose uptake. During physical activity, muscles use glucose for energy, a process that helps lower blood sugar levels and can even occur without the need for insulin. A sedentary lifestyle means this powerful glucose-clearing mechanism is underutilized, contributing to both weight gain and insulin resistance.
- Unhealthy Diet: A diet high in processed foods, sugary beverages, unhealthy fats (saturated and trans fats), and refined carbohydrates can overwhelm the body’s metabolic system. These foods cause rapid spikes in blood sugar and insulin, contributing to weight gain and placing a continuous strain on the pancreas over time.
Who is Most at Risk for Developing Type 2 Diabetes?
Risk factors can be divided into two categories: those you cannot change (unmodifiable) and those you can influence through your choices (modifiable).
Unmodifiable Risk Factors
These are aspects of your biology and history that increase your baseline risk:
- Family History: Having a first-degree relative (parent or sibling) with type 2 diabetes significantly increases your risk.
- Race and Ethnicity: For reasons that are complex and not fully understood but involve genetic, social, and environmental factors, certain groups have a higher prevalence. According to CDC data, this includes people who are African American, Hispanic/Latino, American Indian, Asian American, and Pacific Islander.
- Age: The risk of developing type 2 diabetes increases as you get older, particularly after age 45. This is likely due to a tendency to exercise less, lose muscle mass, and gain weight with age.
- History of Gestational Diabetes: If you developed gestational diabetes during pregnancy, your risk of developing type 2 diabetes later in life is much higher. Having given birth to a baby weighing more than 9 pounds is also a risk factor.
Modifiable Risk Factors
This is where you have the power to make a difference. These factors are direct targets for prevention:
- Prediabetes: Having prediabetes is the number one modifiable risk factor. It’s a clear warning sign that your body is already struggling with glucose control.
- Overweight or Obesity: A Body Mass Index (BMI) of 25 or higher increases risk. Waist circumference is also a key indicator, a waist size over 40 inches for men and 35 inches for women suggests excess visceral fat and higher risk.
- Physical Inactivity: Getting less than 150 minutes of moderate physical activity per week is a major risk factor.
- High Blood Pressure (Hypertension): Having blood pressure over 140/90 mmHg is associated with an increased risk of type 2 diabetes.
- Abnormal Cholesterol Levels: Low levels of “good” cholesterol (HDL) and high levels of triglycerides are part of a metabolic profile that increases diabetes risk.
- Polycystic Ovary Syndrome (PCOS): This hormonal disorder in women is a common condition linked to insulin resistance and a higher risk of developing type 2 diabetes.
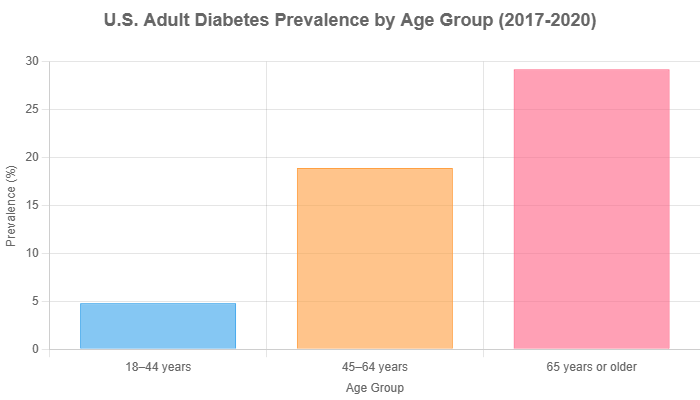
Data Source: CDC National Diabetes Statistics Report, 2017-2020 data.
Recognizing the Symptoms and Getting Diagnosed
One of the most insidious aspects of type 2 diabetes is its stealthy onset.
Unlike type 1 diabetes, where symptoms can appear suddenly and dramatically, type 2 often develops so slowly that it can go unnoticed for years.
This makes recognizing the subtle signs and understanding the diagnostic process critically important for early intervention.
What Are the Common (and Hidden) Symptoms of Type 2 Diabetes?
The Slow and Silent Onset
Many people with type 2 diabetes have no symptoms at all in the early stages.
The gradual rise in blood sugar may not be severe enough to trigger obvious signs of illness.
As the Mayo Clinic notes, it’s possible to live with the condition for years without knowing it.
Often, a person only discovers they have diabetes when they develop long-term complications like heart trouble or vision problems.
Classic Symptoms
When symptoms do appear, they are caused by high blood sugar levels and the body’s attempt to manage them. These classic signs include:
- Frequent urination (polyuria): When there’s excess glucose in the blood, the kidneys work to filter it out. This process pulls extra water into the urine, leading to more frequent trips to the bathroom, especially at night.
- Increased thirst (polydipsia): The frequent urination causes dehydration, which in turn triggers a strong sensation of thirst.
- Increased hunger (polyphagia): Because the body’s cells aren’t getting the glucose they need for energy (due to insulin resistance), the brain receives signals of starvation, leading to persistent hunger even after eating.
- Unexplained weight loss: Despite increased hunger, some people may lose weight. This happens because the body, unable to use glucose for fuel, starts breaking down muscle and fat for energy.
- Fatigue: A profound sense of tiredness is common, as the body’s cells are deprived of their main energy source.
Less Obvious Warning Signs
Beyond the classic symptoms, there are other, more subtle clues that your blood sugar may be elevated:
- Blurred vision: High blood sugar can pull fluid from the lenses of your eyes, affecting your ability to focus. This can be temporary and may resolve as blood sugar levels stabilize.
- Slow-healing sores or frequent infections: High glucose levels can impair immune function and circulation, making it harder for the body to heal from cuts and bruises. It can also lead to more frequent skin, gum, or bladder infections.
- Numbness or tingling in hands or feet (neuropathy): Over time, high blood sugar can damage nerves, often starting with the longest nerves that extend to the feet and hands.
- Areas of darkened skin (acanthosis nigricans): This condition, which causes dark, velvety patches of skin, typically in the armpits, neck, and groin, is a strong indicator of insulin resistance.
How Do Doctors Diagnose Type 2 Diabetes?
If you experience any of the symptoms above or have risk factors for the disease, it’s essential to see a healthcare professional.
Diagnosis is straightforward and is made using simple blood tests that measure glucose levels.
The Key Blood Tests
The American Diabetes Association (ADA) recommends the following tests for diagnosis:
- A1C (Glycated Hemoglobin) Test: This is the most common diagnostic test. It measures your average blood glucose level over the past two to three months. It works by measuring the percentage of hemoglobin (a protein in red blood cells that carries oxygen) that is “glycated”, or coated with sugar. A higher A1C percentage corresponds to higher average blood sugar levels. A major advantage is that you don’t need to fast for this test.
- Fasting Plasma Glucose (FPG) Test: This test measures your blood glucose level at a single point in time after you have fasted (not eaten or drunk anything but water) for at least 8 hours.
- Oral Glucose Tolerance Test (OGTT): This test measures how your body processes glucose. You’ll have a fasting blood sugar level taken, then drink a specific sugary liquid. Your blood sugar is then tested periodically for the next two hours. The OGTT is more sensitive than the FPG test and is often used to diagnose prediabetes or gestational diabetes.
Understanding Your Results
Your test results will place you into one of three categories: normal, prediabetes, or diabetes.
The diagnostic criteria are standardized and shown in the table below.
| Test | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| A1C | Below 5.7% | 5.7% to 6.4% | 6.5% or higher |
| Fasting Plasma Glucose (FPG) | Below 100 mg/dL | 100 to 125 mg/dL | 126 mg/dL or higher |
| Oral Glucose Tolerance Test (OGTT) (2-hour blood glucose) | Below 140 mg/dL | 140 to 199 mg/dL | 200 mg/dL or higher |
Source: American Diabetes Association (ADA) Standards of Care.
A diagnosis of diabetes generally requires two abnormal test results, either from the same sample or from two separate tests.
This confirmation helps ensure an accurate diagnosis before starting a treatment plan.
The Core of the Guide: Comprehensive Management of Type 2 Diabetes
A diagnosis of type 2 diabetes can feel overwhelming, but it’s also the starting point for taking decisive action.
Modern diabetes care is not about deprivation, it’s about empowerment.
The goal is to manage blood glucose, blood pressure, and cholesterol to prevent complications and live a long, healthy life.
Management is a multi-faceted approach, with lifestyle as the undeniable foundation.
How Can I Effectively Manage My Type 2 Diabetes?
Effective management is a partnership between you and your healthcare team.
It revolves around a core set of strategies that work together to keep your body’s systems in balance.
The Cornerstone: Lifestyle Modification
Medications can be powerful tools, but no pill can replace the profound impact of daily habits.
Lifestyle modification is, and always will be, the cornerstone of type 2 diabetes management.
Nutrition and Diet: Fueling Your Body Wisely
The goal of a diabetes-friendly diet is not to eliminate foods but to create balance.
The focus is on nutrient-dense, whole foods that help stabilize blood sugar.
A highly effective and simple strategy recommended by the ADA is the Diabetes Plate Method.
The Diabetes Plate Method:
- Fill half your plate with non-starchy vegetables. Examples include broccoli, spinach, salad greens, green beans, peppers, and tomatoes. These are low in calories and carbohydrates but high in vitamins, minerals, and fiber.
- Fill one quarter of your plate with lean protein. Examples include chicken or turkey without the skin, fish, beans, tofu, and eggs. Protein helps you feel full and has minimal impact on blood sugar.
- Fill the final quarter of your plate with carbohydrate foods. This includes whole grains (brown rice, quinoa, whole-wheat pasta), starchy vegetables (potatoes, corn, peas), fruits, and dairy. These foods have the biggest impact on blood sugar, so portion control is key.
Other important dietary concepts include basic carbohydrate counting to manage intake, understanding the glycemic index (GI)—a measure of how quickly a food raises blood sugar—and prioritizing high-fiber foods, which slow digestion and help prevent sharp blood sugar spikes.
For personalized advice, working with a Registered Dietitian (RD) or Certified Diabetes Care and Education Specialist (CDCES) is invaluable.
Physical Activity and Exercise: Putting Your Muscles to Work
Exercise is medicine for type 2 diabetes. It improves insulin sensitivity, meaning your cells become better at using available insulin to take up glucose from the blood.
The ADA recommends a combination of activities:
- Aerobic Activity: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, spread over at least 3 days. This could be 30 minutes, 5 days a week. Examples include brisk walking, cycling, swimming, or dancing.
- Strength Training: Include 2-3 sessions of resistance training per week on non-consecutive days. This builds muscle mass, and more muscle means more places for your body to store glucose. Examples include lifting weights, using resistance bands, or bodyweight exercises like push-ups and squats.
Weight Management: The 5-7% Solution
For those who are overweight, weight loss is one of the most powerful interventions. You don’t need to lose a dramatic amount of weight to see significant benefits.
The landmark Diabetes Prevention Program (DPP) study showed that losing just 5% to 7% of body weight (e.g., 10-14 pounds for a 200-pound person) and exercising regularly reduced the risk of developing type 2 diabetes by an incredible 58% in people with prediabetes.
This same principle applies to managing existing diabetes, often leading to better blood sugar control and a reduced need for medication.
What Medications Are Used to Treat Type 2 Diabetes?
When lifestyle changes alone are not enough to reach blood sugar targets, medication is added to the plan.
There is a wide array of options available today, allowing for a more personalized approach to treatment.
Oral Medications
These are often the first step in medical treatment.
- Metformin: This is almost always the first-line medication prescribed for type 2 diabetes. It is safe, effective, and inexpensive. Metformin primarily works by reducing the amount of glucose your liver produces and by improving your body’s sensitivity to insulin.
- Other Classes: There are many other classes of oral medications that work in different ways. Your doctor may prescribe them alone or in combination with metformin.
Injectable Medications
For some, oral medications are not enough, or other options may be preferred for their additional benefits.
- GLP-1 Receptor Agonists: This powerful class of non-insulin injectables (and some oral versions) has become a cornerstone of modern diabetes care. They mimic a natural hormone to stimulate insulin release when blood sugar is high, suppress the release of glucose from the liver, slow digestion, and reduce appetite, often leading to weight loss. Many have also been shown to provide significant protection against heart disease. Examples include liraglutide (Victoza), semaglutide (Ozempic, Rybelsus), and dulaglutide (Trulicity).
- Insulin Therapy: Many people with type 2 diabetes will eventually need insulin as their pancreas’s ability to produce it declines over many years. This is a normal progression of the disease, not a sign of failure. There are different types of insulin, including long-acting (basal) insulin to provide background coverage and rapid-acting (bolus) insulin to cover meals.
Why is Blood Sugar Monitoring So Important?
You can’t manage what you don’t measure.
Monitoring blood sugar provides real-time feedback on how your diet, exercise, and medications are affecting your body.
It empowers you and your healthcare team to make timely adjustments to your treatment plan.
Self-Monitoring of Blood Glucose (SMBG)
This traditional method involves using a small device called a glucometer to test a drop of blood from your fingertip.
Your doctor will advise you on how often to test—it might be once a day or multiple times, especially when starting new medications or insulin.
The results help you see immediate cause-and-effect, like how a specific meal or workout impacts your levels.
Continuous Glucose Monitoring (CGM)
This technology represents a major leap forward in diabetes management.
A CGM uses a tiny sensor inserted just under the skin (usually on the arm or abdomen) to measure glucose in the interstitial fluid continuously, 24/7.
A transmitter sends the readings to a smartphone or a dedicated receiver.
CGMs provide a wealth of data, including trend arrows showing if your glucose is rising or falling, and alerts for high and low blood sugar.
This allows for proactive management and provides a more complete picture of your glucose patterns, including overnight levels.
What About the Mental and Emotional Side of Diabetes?
Living with a chronic illness is not just a physical challenge, it’s an emotional and mental one, too.
This is a crucial aspect of care that is often overlooked.
Addressing Diabetes Distress and Burnout
The constant demands of managing type 2 diabetes—the monitoring, medication schedules, dietary choices, and worry about complications—can lead to what’s known as diabetes distress.
It’s a state of feeling frustrated, defeated, or overwhelmed by the burden of self-management. It’s different from depression but can be just as debilitating.
Acknowledging these feelings is the first step. If you’re experiencing burnout, it’s vital to speak with your healthcare provider.
They can help simplify your regimen, set more realistic goals, or connect you with mental health support.
Building a Support System
You are not alone in this journey. A strong support system is essential. This includes:
- Your Healthcare Team: This is your core support, including your primary doctor, an endocrinologist (diabetes specialist), a registered dietitian, and a diabetes educator (CDCES).
- Family and Friends: Educate your loved ones about your condition so they can provide encouragement and practical support.
- Peer Support: Connecting with others who have diabetes can be incredibly validating and helpful. Look for local or online support groups.
Potential Complications and Prevention
The primary goal of managing type 2 diabetes is to prevent or delay its long-term complications.
Chronic high blood sugar is toxic to the body, acting like a slow poison that damages blood vessels and nerves over time.
The good news is that with proactive management and lifestyle changes, the risk of these complications can be dramatically reduced.
What Health Problems Can Unmanaged Type 2 Diabetes Cause?
Complications are generally divided into two categories based on the size of the blood vessels affected.
Macrovascular Complications (Large Blood Vessels)
These complications affect the large arteries that supply blood to the heart, brain, and legs.
- Cardiovascular Disease: This is the number one cause of death and disability for people with type 2 diabetes. According to the American Heart Association, adults with diabetes are two to four times more likely to die from heart disease than adults without diabetes. The condition accelerates atherosclerosis (the hardening and narrowing of arteries), leading to a significantly increased risk of:
- Heart Attack
- Stroke
- High Blood Pressure
- Peripheral Artery Disease (PAD), which reduces blood flow to the legs and feet.
Microvascular Complications (Small Blood Vessels)
These complications result from damage to the tiny blood vessels throughout the body.
- Neuropathy (Nerve Damage): This is one of the most common complications. High blood sugar damages the delicate nerve fibers. It most often affects the feet and hands (peripheral neuropathy), causing symptoms like tingling, numbness, burning, or sharp pains. It can also affect nerves controlling digestion, heart rate, and sexual function.
- Nephropathy (Kidney Disease): Diabetes is the leading cause of chronic kidney disease and kidney failure. The kidneys contain millions of tiny blood vessel clusters that filter waste from the blood. High blood sugar overworks and damages this filtering system, leading to a progressive loss of kidney function that may eventually require dialysis or a kidney transplant.
- Retinopathy (Eye Damage): Diabetes is also a leading cause of new cases of blindness in adults. High blood sugar damages the light-sensitive tissue at the back of the eye (the retina). This condition, called diabetic retinopathy, can lead to vision loss and, if untreated, blindness. Regular eye exams are crucial for early detection and treatment.
Other Related Health Issues
The impact of diabetes extends to other body systems, increasing the risk for foot problems (due to poor circulation and nerve damage, which can lead to amputation), skin conditions, hearing impairment, sleep apnea, and even a higher risk of developing dementia and certain types of cancer.
Can Type 2 Diabetes Be Prevented or Delayed?
Absolutely. This is perhaps the most hopeful message in the entire discussion of type 2 diabetes.
For the millions of people with prediabetes, the future is not set in stone.
Prediabetes should be viewed as a critical fork in the road—a powerful opportunity to make changes that can prevent or significantly delay the onset of the full-blown disease.
Evidence-Based Prevention Strategies
The research is clear and consistent. The strategies for preventing type 2 diabetes are the same ones used to manage it.
The Diabetes Prevention Program (DPP) and other major studies have proven the effectiveness of the following steps:
- Achieve and Maintain a Healthy Weight. This is the most effective prevention strategy. As shown in the DPP, losing just 5-7% of your body weight can reduce your risk of developing type 2 diabetes by 58%. This modest weight loss improves the body’s ability to use insulin dramatically.
- Engage in Regular Physical Activity. Aim for at least 150 minutes of moderate-intensity activity, like brisk walking, each week. Exercise makes your muscles more sensitive to insulin and helps your body use glucose more effectively.
- Adopt a Healthy Eating Pattern. Focus on a diet rich in whole foods. Prioritize non-starchy vegetables, fruits, whole grains, and lean sources of protein. Significantly reduce or eliminate sugary drinks and highly processed foods.
- Don’t Smoke and Manage Stress. Smoking increases insulin resistance, and chronic stress can raise blood sugar levels. Addressing these factors contributes to overall metabolic health.
“We conclude that T2D is preventable by changing lifestyle and the risk reduction is sustained for many years after the active intervention. This is a message of hope for the millions of people at risk.” – Uusitupa M, et al. Prevention of Type 2 Diabetes by Lifestyle Changes.
The Future of Diabetes Care & Research
The landscape of type 2 diabetes treatment is evolving at a rapid pace.
While lifestyle remains the foundation, scientific advancements are paving the way for more personalized, precise, and effective management strategies that were unimaginable just a decade ago.
What’s on the Horizon for Type 2 Diabetes Treatment?
The future is moving away from a one-size-fits-all approach and toward therapies tailored to the individual.
Precision Medicine
Researchers are beginning to understand that type 2 diabetes is not a single disease but a collection of subtypes with different underlying causes.
Precision medicine aims to leverage this understanding by tailoring treatment based on an individual’s unique genetic makeup, metabolic profile, environment, and lifestyle.
For example, one person’s diabetes might be primarily driven by severe insulin resistance, while another’s might be due to a more rapid decline in insulin production.
In the future, a simple blood test might help a doctor select the medication class (e.g., an SGLT2 inhibitor vs. a GLP-1 agonist) that is most likely to be effective for that specific patient, minimizing trial and error.
The Role of the Gut Microbiome
One of the most exciting frontiers in medical research is the gut microbiome—the trillions of bacteria living in our digestive tracts.
Emerging research, such as a 2025 perspective in the journal Signal Transduction and Targeted Therapy, highlights how the composition of these bacteria can profoundly influence metabolism.
Studies show that people with type 2 diabetes often have a different balance of gut bacteria compared to those without.
These microbes produce metabolites that can affect insulin sensitivity, inflammation, and even appetite.
This research opens the door to novel therapies, such as targeted probiotics or dietary interventions designed to cultivate a healthier gut environment to help manage or prevent diabetes.
Technological Advances
Technology continues to revolutionize daily diabetes management.
Continuous Glucose Monitors (CGMs) are becoming smaller, more accurate, and longer-lasting.
The data they provide is being integrated into “smart” insulin pens and insulin pumps, creating hybrid closed-loop systems often called an “artificial pancreas”.
These systems can automatically adjust insulin delivery in response to real-time glucose readings, reducing the mental burden on the user and improving glycemic control.
Alongside this, new drug developments continue to offer more options with fewer side effects and added benefits like weight loss and cardiovascular protection.
Frequently Asked Questions (FAQ)
1. Can type 2 diabetes be cured?
There is currently no “cure” for type 2 diabetes. However, it can be put into remission through significant lifestyle changes, particularly substantial weight loss. Remission means blood sugar levels return to the normal range without needing medication, but ongoing healthy habits are required to maintain it.
2. Can you reverse type 2 diabetes?
The term “reversal” is often used interchangeably with remission. Through intensive lifestyle management (diet, exercise, and significant weight loss), many people can achieve normal blood sugar levels without medication. This is most achievable for those who are newly diagnosed.
3. What is a normal A1C level?
A normal A1C level for someone without diabetes is below 5.7%. For someone diagnosed with diabetes, a common treatment target is an A1C below 7.0%, but your individual goal should be set with your healthcare provider.
4. What foods should I avoid with type 2 diabetes?
It’s best to limit or avoid sugary drinks (soda, sweet tea, juice), highly processed carbohydrates (white bread, pastries), and foods high in trans fats. These foods can cause rapid spikes in blood sugar and offer little nutritional value.
5. Is fruit bad for people with diabetes?
No, whole fruits are not bad. They contain fiber, vitamins, and minerals. While they do contain natural sugar, the fiber slows its absorption. Portion control is key, it’s better to eat a whole apple than to drink apple juice.
6. Do I have to take medication for type 2 diabetes forever?
Not necessarily. If you achieve significant weight loss and maintain a healthy lifestyle, you may be able to reduce or even stop your medications, in consultation with your doctor. However, for many, medication is a long-term tool to manage the progressive nature of the disease.
7. Can stress raise my blood sugar?
Yes. When you’re stressed, your body releases hormones like cortisol and adrenaline, which can cause your liver to release more glucose into the bloodstream. Managing stress through techniques like exercise, meditation, or mindfulness is an important part of diabetes care.
8. How much does diabetes cost in the US?
The economic burden is immense. The total estimated cost of diagnosed diabetes in the U.S. in 2022 was $412.9 billion, including direct medical costs and indirect costs from lost productivity, according to a study in Diabetes Care.
9. Is type 2 diabetes a genetic disease?
It has a strong genetic component, meaning risk can be inherited. However, it is not purely genetic. Lifestyle factors like diet and exercise play a critical role in determining whether someone with a genetic predisposition will actually develop the disease.
10. What is the first sign of type 2 diabetes?
Often, there are no signs. The disease can be silent for years. When symptoms do appear, some of the earliest can be increased thirst, frequent urination, and unexplained fatigue. This is why regular screening for those at risk is so important.
Conclusion
Type 2 diabetes is a complex and serious health condition, but it is far from a hopeless diagnosis.
As we’ve explored, it is a manageable disease, and in many cases, a preventable one.
Knowledge is the most critical tool in your arsenal—understanding what is happening in your body, why it’s happening, and what you can do about it.
Key Takeaways
- It’s a Manageable Condition: Type 2 diabetes is a chronic illness defined by insulin resistance and a relative lack of insulin, but it is not a life sentence. Modern treatments and lifestyle strategies can lead to excellent long-term health.
- Lifestyle is the Foundation: No medication can substitute for the power of a healthy diet, regular physical activity, and weight management. These are the cornerstones of both prevention and control.
- Early Action is Critical: The prediabetes stage is a crucial window of opportunity. By making lifestyle changes at this point, you can dramatically reduce your risk of progressing to full-blown diabetes.
- Management is Comprehensive: Effective control goes beyond just blood sugar. It involves managing blood pressure and cholesterol, regular medical check-ups, and paying attention to your mental and emotional well-being.
The journey with type 2 diabetes is a marathon, not a sprint. It requires consistency, patience, and a partnership with a trusted healthcare team.
But the message of this guide is ultimately one of empowerment.
A diagnosis can be the catalyst for profound and positive changes, leading you toward a more mindful, active, and healthier life than ever before.
Your health is in your hands. Take the information you’ve learned here and use it to start a conversation.
Talk to your healthcare provider to assess your personal risk or to create a personalized management plan that works for you.
What are your biggest questions or concerns about managing type 2 diabetes? Share your thoughts or experiences in the comments below to help and learn from others in the community.

