Effective trigeminal neuralgia treatment involves a range of options from medications to advanced surgical procedures designed to manage the severe, shock-like facial pain it causes.
The primary goal is to block or reduce the pain signals sent to your brain. With an estimated 150.000 new cases diagnosed in the U.S. each year, understanding the full spectrum of available therapies is crucial for finding relief.
This condition, while not life-threatening, can be physically and emotionally devastating, profoundly impacting quality of life.
This comprehensive guide will walk you through every aspect of managing trigeminal neuralgia. We will explore the causes and symptoms, detail the diagnostic process, and provide an in-depth comparison of all major non-surgical and surgical treatments.
By the end, you will have a clear, authoritative understanding of the pathways to managing this challenging condition and reclaiming your life from pain.
In This Article
What Is Trigeminal Neuralgia (TN)?
Trigeminal neuralgia (TN), also known as tic douloureux, is a chronic pain condition characterized by sudden, severe and debilitating facial pain.
The pain is often described as an intense, stabbing, or electric shock-like sensation on one side of the face. It affects the trigeminal nerve, the fifth cranial nerve, which is responsible for carrying sensation from your face to your brain.
According to the National Institute of Neurological Disorders and Stroke (NINDS), these pain attacks are abrupt, typically lasting from a few seconds to as long as two minutes, but they can occur in rapid succession.
The intensity of the pain can be physically and emotionally overwhelming. Trigeminal neuralgia is a form of neuropathic pain, meaning it originates from nerve injury or a nerve lesion, rather than an external stimulus.
While the condition can occur at any age, it is most common in people over 50 and affects women more often than men.
The attacks can go into remission for weeks, months, or even years, but the typical pattern is for them to become more frequent and intense over time, making effective trigeminal neuralgia treatment essential for long-term quality of life.
Understanding the Trigeminal Nerve: The Source of the Pain
To understand trigeminal neuralgia, it’s essential to understand the nerve it affects. The trigeminal nerves are a pair of cranial nerves, one on each side of the head, that originate in the brainstem.
As the name suggests (from the Latin “tria” for three and “geminus” for twin), each nerve divides into three main branches that provide sensation to different parts of the face.
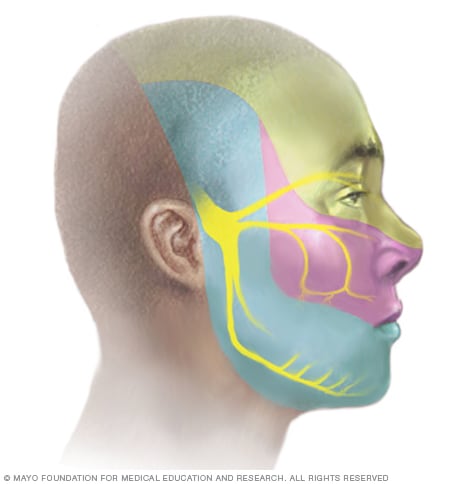
The three branches of the trigeminal nerve (V1, V2, and V3) supply sensation to the upper, middle and lower parts of the face.
The three branches are:
- The Ophthalmic Nerve (V1): This upper branch supplies sensation to the scalp, forehead, front of the head, upper eyelid, and eye.
- The Maxillary Nerve (V2): The middle branch is responsible for sensation in the cheek, side of the nose, upper jaw, top lip, and upper teeth and gums.
- The Mandibular Nerve (V3): This lower branch supplies nerves to the lower jaw, bottom lip, and lower teeth and gums. It also controls some of the muscles used for chewing.
Trigeminal neuralgia can affect one or more of these branches. The maxillary (V2) and mandibular (V3) branches are the most commonly affected.
Pain isolated to the ophthalmic (V1) branch is rare, occurring in less than 5% of cases. In very rare instances, a condition called bilateral TN can affect both sides of the face, though usually not at the same time.
What Are the Symptoms of Trigeminal Neuralgia?
The symptoms of trigeminal neuralgia are distinctive and can vary in pattern and intensity.
While initial episodes may be short and mild, the condition is often progressive, with attacks becoming longer and more frequent over time.
Recognizing these symptoms is the first step toward a correct diagnosis and effective treatment.
Types of Trigeminal Neuralgia Pain
Pain from trigeminal neuralgia is generally classified into two types, as described by the American Association of Neurological Surgeons (AANS):
- Type 1 (TN1): This is the “classic” form, characterized by intense, sharp, stabbing, or shock-like facial pain that is sporadic. These attacks are severe but are followed by pain-free periods.
- Type 2 (TN2): This form involves a more constant, persistent pain described as aching, burning, or throbbing. People with TN2 may also experience the stabbing pains of TN1, but they are typically less intense.
A person can have both TN1 and TN2, and the condition can evolve from one type to another over time.
Common Symptom Patterns
Based on information from leading institutions like the Mayo Clinic, patients with trigeminal neuralgia may experience one or more of the following:
- Sudden, Severe Pain: Episodes of excruciating, shooting, or jabbing pain that feel like an electric shock.
- Triggered Attacks: Pain that is suddenly brought on by light touch or vibration.
- Short Duration: Attacks typically last from a few seconds to a couple of minutes.
- Facial Spasms: The pain can be accompanied by an uncontrollable twitching of the face (a “tic”).
- Cyclical Episodes: Periods of frequent attacks lasting days, weeks, or months, followed by periods of remission with no pain.
- Specific Locations: Pain is concentrated in areas supplied by the trigeminal nerve, such as the cheek, jaw, teeth, gums or lips. The eye and forehead are less commonly affected.
- Unilateral Pain: The pain almost always affects only one side of the face at a time.
- Rare During Sleep: Pain attacks seldom occur while sleeping.
- Progressive Nature: Over time, the attacks can become more frequent and intense, and the pain-free intervals may shorten.
What Causes Trigeminal Neuralgia and What Are the Triggers?
The underlying cause of trigeminal neuralgia is the irritation or disruption of the trigeminal nerve’s function.
This disruption leads the nerve to misfire, sending abnormal pain signals to the brain.
The causes are categorized based on their origin.
Types of Trigeminal Neuralgia by Cause
Medical experts classify trigeminal neuralgia into three main types based on the cause:
- Classic Trigeminal Neuralgia: This is the most common form. It is caused by a blood vessel—most often the superior cerebellar artery—compressing the trigeminal nerve root where it exits the brainstem. This constant pulsation puts pressure on the nerve, which can wear away its protective myelin sheath, leading to erratic pain signals.
- Secondary Trigeminal Neuralgia: In these cases, the pain is a symptom of another underlying medical condition. According to NINDS, this accounts for about 15% of cases. Common causes include:
- Multiple Sclerosis (MS): MS causes demyelination (damage to the myelin sheath) throughout the central nervous system, which can affect the trigeminal nerve. The prevalence of TN in patients with MS is significantly higher than in the general population.
- Tumor or Cyst: A benign or malignant growth can press on the trigeminal nerve.
- Arteriovenous Malformation (AVM): A tangle of abnormal blood vessels can compress the nerve.
- Facial Injury or Stroke: Trauma or a brain lesion can damage the nerve.
- Idiopathic Trigeminal Neuralgia: When extensive diagnostic evaluation, including high-resolution imaging, fails to identify a clear cause, the condition is considered idiopathic. This is the least common type.
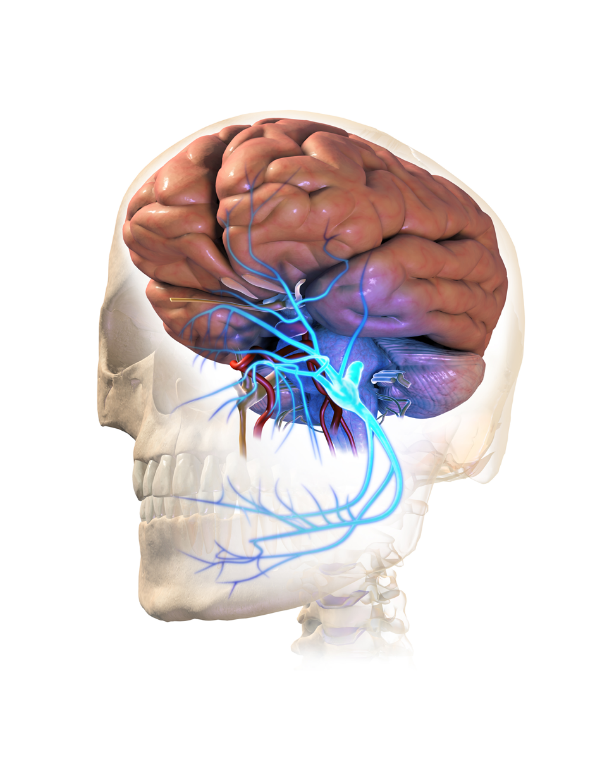
Classic trigeminal neuralgia is often caused by a blood vessel compressing the trigeminal nerve root.
Common Pain Triggers
A hallmark of trigeminal neuralgia is that the severe pain attacks can be triggered by innocuous, everyday stimuli.
Patients often learn to avoid these triggers to prevent an attack. Common triggers include:
- Touching the face (even lightly)
- Washing the face or applying makeup
- Shaving
- Brushing teeth
- Eating or drinking
- Talking or smiling
- A breeze or wind blowing on the face
- Blowing the nose
The fear of triggering an attack can lead to significant lifestyle changes, causing some individuals to avoid eating, talking, or even going outside. This highlights the profound impact trigeminal neuralgia has on a person’s quality of life.
How Is Trigeminal Neuralgia Diagnosed?
Diagnosing trigeminal neuralgia can be challenging because there is no single definitive test for the condition, and its symptoms can mimic other facial pain disorders, such as dental problems or temporomandibular joint (TMJ) syndrome.
A diagnosis is primarily based on a thorough clinical evaluation.
The Diagnostic Process
A healthcare provider, often a neurologist, will use a multi-step process to diagnose trigeminal neuralgia:
- Detailed Medical History: The most crucial part of the diagnosis is your description of the pain. Your doctor will ask about:
- Type of Pain: Is it sharp, shooting, stabbing or electric shock-like?
- Location: Where exactly on your face do you feel the pain?
- Triggers: What activities or stimuli bring on the pain?
- Duration and Frequency: How long do attacks last, and how often do they occur?
- Physical and Neurological Examination: The doctor will examine your face, mouth and teeth. They will perform a neurological exam to test your reflexes, strength and sensation in different parts of your face. This helps pinpoint which branch of the trigeminal nerve is affected and can help rule out other conditions. The presence of a “trigger zone” on the face is a strong indicator of TN.
- Magnetic Resonance Imaging (MRI): An MRI of the brain is essential. As noted by the AANS, a high-resolution MRI (often called a FIESTA or CISS sequence) can achieve two primary goals:
- Identify Secondary Causes: It can detect if a tumor, cyst, or multiple sclerosis lesion is the cause of the pain.
- Visualize Neurovascular Compression: It can show if a blood vessel is compressing the trigeminal nerve root, which is the hallmark of classic trigeminal neuralgia.
Ruling Out Other Conditions (Differential Diagnosis)
Because facial pain can have many causes, your doctor will work to rule out other disorders that can mimic trigeminal neuralgia, including:
- Dental issues (like a tooth abscess)
- Temporomandibular Joint (TMJ) disorder
- Post-herpetic neuralgia (pain after a shingles outbreak)
- Cluster headaches or migraines
- Sinus infections
- Glossopharyngeal neuralgia (a similar condition affecting a different nerve)
A correct diagnosis is vital, as the treatment for trigeminal neuralgia is very different from treatments for other types of facial pain.
What Are the Non-Surgical Treatment Options for Trigeminal Neuralgia?
For most people diagnosed with trigeminal neuralgia, non-surgical treatments are the first line of defense.
The goal is to reduce the frequency and severity of pain attacks and improve quality of life.
This approach primarily involves medication, but can also include complementary therapies.
Medications for Trigeminal Neuralgia
Standard over-the-counter pain relievers like ibuprofen and aspirin, as well as opioid medications, are generally not effective for the nerve pain of trigeminal neuralgia. Instead, doctors prescribe specific medications that calm overactive nerve signals.
According to guidelines from the American Academy of Neurology (AAN) and European Federation of Neurological Societies (EFNS), the primary medications are anticonvulsants.
First-Line Medications
- Carbamazepine: This anticonvulsant is the most common and often most effective initial treatment. It works by blocking pain signals from the nerves. However, its effectiveness can decrease over time, and it has side effects like dizziness, drowsiness and nausea.
- Oxcarbazepine: Structurally related to carbamazepine, this medication is often preferred because it tends to have fewer side effects and drug interactions. A real-world study showed it was better tolerated than carbamazepine.
Second-Line and Other Medications
If first-line drugs are ineffective or cause intolerable side effects, other options may be tried:
- Baclofen: A muscle relaxant that can be used alone or in combination with carbamazepine.
- Gabapentin and Pregabalin: Other anticonvulsants that can help manage nerve pain.
- Lamotrigine: Another anticonvulsant, often added if a single drug isn’t providing enough relief.
- Botulinum Toxin A (Botox) Injections: Some smaller studies have shown that Botox injections can reduce pain for people who no longer respond to oral medications, though more research is needed for this to become a standard trigeminal neuralgia treatment.
Medications are typically started at a low dose and gradually increased until pain relief is achieved. This helps minimize side effects.
However, long-term use can be challenging due to decreasing effectiveness and side effects like fatigue, memory issues or dizziness.
Complementary and Alternative Therapies
Some people find relief by combining medical treatment with complementary approaches.
While the success of these therapies varies widely among individuals, they can be a valuable part of a holistic pain management plan.
Options mentioned by NINDS and other sources include:
- Acupuncture: Some studies suggest acupuncture can help reduce pain and improve quality of life for TN patients.
- Biofeedback: A technique to help you gain control over involuntary bodily functions, which may help in managing pain responses.
- Yoga and Meditation: These practices can help manage the stress and anxiety associated with chronic pain.
- Nutritional Therapy: While not a direct cure, a healthy diet can support overall nerve health.
- Low-impact exercise: Gentle physical activity can improve mood and overall well-being.
It is crucial to discuss any complementary therapies with your doctor to ensure they are safe and do not interfere with your primary medical treatment for trigeminal neuralgia.
What Are the Surgical Treatment Options for Trigeminal Neuralgia?
When medications fail to control the pain of trigeminal neuralgia or their side effects become unbearable, surgery becomes a critical consideration.
Surgical treatments aim to either stop a blood vessel from compressing the nerve or intentionally damage the nerve to block pain signals.
The choice of procedure depends on the patient’s health, the specific cause of their TN and personal preference.
Surgical options are broadly divided into two categories: open cranial surgery (MVD) and less invasive lesioning procedures.
Microvascular Decompression (MVD)
Microvascular Decompression (MVD) is considered the most effective long-term surgical treatment for classic trigeminal neuralgia.
It is the only procedure that addresses the root cause of the problem—neurovascular compression—rather than just treating the symptoms by damaging the nerve.
- How it works: A neurosurgeon makes a small incision behind the ear and creates a small opening in the skull (a craniotomy). Using a microscope, the surgeon identifies the blood vessel(s) compressing the trigeminal nerve and gently moves it away. A tiny, soft cushion, typically made of Teflon, is placed between the nerve and the artery to prevent future contact.
- Effectiveness: MVD has a high success rate. Studies, such as a landmark paper in the New England Journal of Medicine, show that it provides complete, long-term pain relief in a majority of patients (around 70-80%). A recent 5-year prospective study published in 2025 confirmed MVD’s superiority, with 59% of patients being pain-free without medication compared to 19% in a medically managed group.
- Risks: As the most invasive option, it carries risks associated with brain surgery, including infection, hearing loss, facial numbness, and, in rare cases, stroke or death. However, in the hands of an experienced neurosurgeon, the risk of major complications is very low (around 1-2%).
Rhizotomy (Nerve Lesioning Procedures)
A rhizotomy is a procedure that intentionally damages nerve fibers to prevent them from sending pain signals.
These procedures are less invasive than MVD but are also generally less durable, with pain often returning after a few years.
A common side effect of all rhizotomies is some degree of permanent facial numbness.
Types of Rhizotomy:
- Balloon Compression: A surgeon inserts a hollow needle through the cheek to the trigeminal nerve. A small balloon is passed through a catheter and inflated to compress the nerve, injuring the pain-causing fibers. It is then deflated and removed.
- Glycerol Injection: A thin needle is guided to the area where the nerve divides into its three branches. A small amount of sterile glycerol is injected, which damages the nerve fibers and blocks pain signals.
- Radiofrequency Thermal Lesioning: Also known as RF ablation, this procedure uses a needle to deliver a heating current to a specific part of the trigeminal nerve. The heat destroys the nerve fibers responsible for the pain. The surgeon can control the extent of the lesion to target the pain area precisely.
Stereotactic Radiosurgery (Gamma Knife or CyberKnife)
This is a non-invasive procedure that uses highly focused beams of radiation to create a lesion on the trigeminal nerve root.
It does not require any incisions or general anesthesia.
- How it works: Hundreds of small radiation beams are precisely targeted at the trigeminal nerve where it enters the brainstem. The radiation exposure slowly damages the nerve over several weeks to months, eventually interrupting the transmission of pain signals.
- Effectiveness: Pain relief is not immediate and can take over a month to develop. It is effective for many patients, but the pain relief may not be as long-lasting as MVD.
- Risks: The primary risk is the gradual onset of facial numbness. Other risks of radiation are minimal due to the precise targeting. It is a good option for patients who are not candidates for open surgery.
Comparative Table of Surgical Treatments
Choosing the right surgery is a significant decision. This table compares the main surgical options for trigeminal neuralgia to help you understand the differences.
| Procedure | How It Works | Invasiveness | Initial Success Rate | Long-Term Durability | Key Risks & Side Effects |
|---|---|---|---|---|---|
| Microvascular Decompression (MVD) | Separates compressing blood vessel from the nerve with a cushion. | High (Open cranial surgery) | ~90% | High (~70-80% pain-free at 10 years) | Surgical risks (infection, CSF leak), hearing loss, facial weakness. Numbness is not the goal. |
| Balloon Compression | Injures nerve fibers by inflating a balloon against them. | Minimally Invasive (Needle-based) | ~80-90% | Moderate (Pain often returns in 2-5 years) | Facial numbness, weakness in chewing muscles, bleeding. |
| Glycerol Injection | Chemically damages nerve fibers with glycerol. | Minimally Invasive (Needle-based) | ~70-90% | Moderate to Low (Pain often returns in 1-4 years) | Facial numbness/tingling, risk of glycerol spreading. |
| Radiofrequency Lesioning | Destroys nerve fibers with a heated electrode. | Minimally Invasive (Needle-based) | ~90% | Moderate (Pain often returns in 2-5 years) | Facial numbness, painful numbness (anesthesia dolorosa), weakness in chewing muscles. |
| Stereotactic Radiosurgery | Damages the nerve root with focused radiation. | Non-Invasive | ~60-80% | Moderate (Pain may return after 3-5 years) | Delayed facial numbness (can take months to appear), delayed pain relief. |
What Is Life Like with Trigeminal Neuralgia?
Living with trigeminal neuralgia extends far beyond the physical pain. The unpredictable and excruciating nature of the attacks can have a profound psychological and social impact, significantly eroding a person’s quality of life.
Many who suffer from this condition describe it as living in constant fear of the next attack.
“The intensity of pain can be physically and emotionally devastating”, states NINDS. This sentiment is echoed by countless patients who experience the condition firsthand.
Research published in the journal Pain found unequivocal evidence that trigeminal neuralgia causes disability, with up to 45% of patients being absent from their usual daily activities for 15 days or more in a six-month period.
The study also highlighted the mental health toll:
- Over 50% of patients experienced significant anxiety.
- Nearly 36% had mild-to-severe depression.
- 78% reported considerable negative thoughts related to their pain.
The fear of triggering pain can lead to social isolation, as individuals may avoid talking, eating in public or even smiling.
This can strain relationships and lead to feelings of loneliness. Some patients experience weight loss due to difficulty eating.
The constant threat of pain, combined with the side effects of medications like drowsiness and confusion, can make it difficult to work, parent, or engage in hobbies, further contributing to a diminished sense of self and purpose.
However, it’s important to remember that a diagnosis of trigeminal neuralgia is not a life sentence of pain.
With a proper diagnosis and a comprehensive treatment plan developed with a multidisciplinary team, most people can achieve significant pain control and restore their quality of life.
What Is the Latest Research on Trigeminal Neuralgia?
The medical community is actively researching trigeminal neuralgia to better understand its underlying mechanisms and develop more effective, better-tolerated treatments. This research offers hope for the future of TN care.
Organizations like the National Institute of Neurological Disorders and Stroke (NINDS) and the Facial Pain Research Foundation are at the forefront of funding and promoting these efforts.
Key Areas of Current Research:
- Genetics and Molecular Mechanisms: Scientists are amassing large DNA collections from TN patients to identify potential genetic predispositions. As reported by UF Health in early 2025, this research aims to unlock genetic clues that could lead to a cure. Other studies are exploring the molecular changes and channelopathies (problems with ion channels in nerve cells) that lead to the hyperexcitability of the trigeminal nerve.
- Novel Drug Therapies: Recognizing the limitations and side effects of current medications, researchers are investigating new pharmacological targets. This includes non-opioid treatments like immunomodulatory therapy, which alters the body’s immune response to reduce nerve inflammation and pain. Modified forms of botulinum toxin (Botox) are also being tested as a way to block pain transmission more effectively.
- Advanced Imaging Techniques: Researchers are developing more sophisticated MRI techniques to better diagnose trigeminal neuralgia. These methods aim to not only visualize neurovascular compression but also to detect microstructural abnormalities and demyelination within the nerve itself, which could help distinguish between classic, secondary and idiopathic forms of TN.
- Neuromodulation: For patients who don’t respond to other treatments, neuromodulation offers a promising frontier. Techniques like Transcranial Magnetic Stimulation (TMS) are being studied in clinical trials, such as one at UCSF, to see if non-invasively stimulating the brain can modulate pain pathways and provide relief.
- Improving Surgical Outcomes: Neurosurgeons continue to refine surgical techniques. For example, Mayo Clinic has reported on an innovative MVD technique using fibrin glue instead of Teflon to secure the blood vessel, potentially reducing the risk of pain recurrence.
Patients interested in participating in cutting-edge research can search for active studies on websites like ClinicalTrials.gov.
Participation in these trials is vital for advancing the science and improving care for everyone affected by trigeminal neuralgia.
Frequently Asked Questions (FAQ)
Can trigeminal neuralgia be cured?
While there is no definitive cure, treatments like Microvascular Decompression (MVD) surgery can provide long-term, complete pain relief for many people by addressing the root cause. Other treatments effectively manage symptoms, allowing for a high quality of life.
Does trigeminal neuralgia shorten your life?
No, trigeminal neuralgia itself is not a fatal condition and does not reduce life expectancy. However, the severe pain can significantly impact mental health and quality of life, making effective management crucial for overall well-being.
What is the best medication for trigeminal neuralgia?
Carbamazepine and oxcarbazepine are considered the first-line and most effective medications for controlling the nerve pain of trigeminal neuralgia. They are anticonvulsant drugs that work by blocking erratic pain signals from the nerve to the brain.
Can stress make trigeminal neuralgia worse?
While stress is not a direct cause, it can lower your pain threshold and exacerbate symptoms. Many patients report that their attacks are more frequent or severe during periods of high stress, making stress management an important part of a holistic treatment plan.
Is trigeminal neuralgia a sign of MS?
It can be. While most cases of TN are not related to Multiple Sclerosis (MS), the incidence of trigeminal neuralgia is much higher in people with MS. The development of TN in a younger person, especially with bilateral pain, raises suspicion for MS.
Can dental work cause trigeminal neuralgia?
It’s unlikely that dental work directly causes TN. More often, an underlying, pre-existing trigeminal neuralgia is triggered or first noticed during or after a dental procedure, leading patients to initially believe the pain is from a dental issue.
What is the difference between TN1 and TN2?
TN1 (classic) involves sharp, stabbing, shock-like pain with pain-free intervals. TN2 (atypical) is characterized by a more constant, persistent aching, burning, or throbbing pain, though it can also include some sharp attacks.
Why are regular painkillers ineffective for trigeminal neuralgia?
Regular painkillers like NSAIDs or opioids target pain from inflammation or tissue damage. Trigeminal neuralgia is neuropathic pain, caused by nerve dysfunction. It requires medications that calm nerve hyperexcitability, like anticonvulsants.
Conclusion
Trigeminal neuralgia is a complex and painful condition, but it is manageable. From highly effective first-line medications like carbamazepine to definitive surgical solutions like microvascular decompression, there are more pathways to relief available today than ever before.
The key is a prompt and accurate diagnosis, followed by a personalized treatment plan developed in partnership with a multidisciplinary medical team, including neurologists and neurosurgeons.
Understanding your symptoms, knowing the potential causes, and exploring the full range of treatment options empowers you to make informed decisions about your health.
While the journey can be challenging, ongoing research continues to bring new hope and improved therapies. You do not have to live a life defined by pain.
If you are experiencing symptoms of facial nerve pain, take the first step and consult with your healthcare provider. Discuss the treatment options outlined in this guide to find the best approach for you.
Have you or a loved one been affected by trigeminal neuralgia? Share your experience or questions in the comments below to connect with others and contribute to our community of support.
Medical Disclaimer
The information provided in this article is for educational and informational purposes only and is not intended as medical advice. It should not be used to diagnose or treat any health problems or illnesses. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition. Do not disregard professional medical advice or delay in seeking it because of something you have read in this article.

