The most effective treatments for nail fungus (onychomycosis) are prescription oral antifungal medications like terbinafine and itraconazole, which offer the highest cure rates.
Affecting up to 10% of the global population and over 1 in 5 people aged 40-60, this stubborn infection requires a targeted, evidence-based approach.
This definitive guide, based on dermatologist insights and scientific evidence, will walk you through everything you need to know—from identifying the first signs and understanding the different types of infection to a deep dive into the most effective medical treatments, in-office procedures, and proven prevention strategies.
Read on to find the best path to clear, healthy nails.
In This Article
What Exactly Is Nail Fungus (Onychomycosis)?
Nail fungus, known medically as onychomycosis, is a common infection that affects the nail plate, the nail bed (the skin under the nail), or the matrix from which the nail grows.
It is caused by an overgrowth of microscopic fungi that find an ideal home in warm, dark, and moist environments—like the inside of a shoe.
These organisms are not just passive residents, they actively thrive by feeding on keratin, the very protein that provides structure and hardness to our nails, hair, and skin.
The primary culprits behind this persistent condition belong to a group of fungi called dermatophytes.
Among them, Trichophyton rubrum is the most frequently identified pathogen in clinical settings, responsible for a majority of cases.
However, they are not the only offenders.
Other fungal organisms, including yeasts (such as Candida albicans) and various non-dermatophyte molds (like Aspergillus or Fusarium), can also invade the nail unit and cause infection, sometimes leading to different clinical presentations and treatment challenges.
While onychomycosis can develop on both fingernails and toenails, it has a strong predilection for the feet.
The MSD Manuals state that toenails are infected up to 10 times more often than fingernails.
This disparity is largely due to the environment: toes are frequently confined within shoes, creating a warm, sweaty, and dark space that is perfect for fungal proliferation. In contrast, hands are typically exposed to air and light, making them less hospitable for these organisms.
A crucial point often overlooked by patients is the intimate connection between nail fungus and athlete’s foot, medically termed tinea pedis.
As the Mayo Clinic explains, the same dermatophyte fungi are responsible for both conditions.
An untreated athlete’s foot infection on the skin between the toes or on the sole can easily migrate and invade a nearby toenail, establishing a new, more fortified infection.
Conversely, a chronic nail fungus infection can act as a persistent reservoir, shedding fungi and causing recurrent bouts of athlete’s foot.
This bidirectional relationship underscores the importance of treating both conditions comprehensively to achieve a lasting cure and prevent reinfection.
How to Identify Nail Fungus: Key Symptoms and Types
Recognizing the signs of nail fungus early is critical, as prompt intervention can lead to a more straightforward and successful treatment.
The infection often begins subtly, as a small white or yellowish spot under the tip of the nail, which can be easily dismissed.
However, as the fungus penetrates deeper into the nail plate, the signs become more pronounced and unmistakable.
Common Symptoms of Nail Fungus
A dermatologist will look for a combination of the following signs.
You can use this list for self-assessment, but a professional diagnosis is always necessary. The most common symptoms include:
- Discoloration: The nail may lose its healthy, translucent appearance, turning opaque. It can develop shades of white, yellow, brown, or in some cases of bacterial co-infection, even green or black .
- Thickening (Onychauxis): The nail becomes thicker than normal, making it difficult to cut with standard clippers.
- Brittleness and Crumbling: The nail loses its integrity, becoming fragile, crumbly, or ragged at the edges. Pieces may break off easily.
- Distortion of Shape: The nail can become misshapen, losing its smooth surface and developing ridges or a warped appearance.
- Separation from Nail Bed (Onycholysis): The infected portion of the nail may lift away from the underlying skin, creating a space where debris can accumulate.
- Subungual Debris: A buildup of keratin, skin cells, and fungal matter can collect under the nail, contributing to its thickened and discolored look.
- Odor: In some cases, the accumulated debris and infection can produce a slightly foul or musty smell.
A Deeper Dive: The Four Main Types of Onychomycosis
Understanding the specific type of onychomycosis is not just an academic exercise, it can inform the most effective treatment strategy.
Dermatologists classify the infection into four primary patterns based on how the fungus invades the nail unit.
1. Distal and Lateral Subungual Onychomycosis (DLSO)
This is by far the most common form of nail fungus, affecting both toenails and fingernails.
The infection begins at the distal (far) edge or the lateral (side) edges of the nail.
From there, the fungus invades the nail bed and the underside of the nail plate, progressing slowly toward the cuticle.
Visually, it often presents as yellowish or brownish streaks, accompanied by thickening and the separation of the nail from the nail bed .
2. White Superficial Onychomycosis (WSO)
Less common than DLSO, this type involves a direct invasion of the superficial (top) layers of the nail plate.
It appears as distinct, well-defined “chalky” white patches or spots on the surface of the nail.
Over time, these patches can spread to cover the entire nail, giving it a rough, soft, and crumbly texture.
A key feature of WSO is that the infected white areas can often be scraped away.
This type is almost exclusively found on toenails and may respond better to topical treatments because the infection is more accessible.
3. Proximal Subungual Onychomycosis (PSO)
This is the least common pattern in the general population but is a significant clinical marker.
In PSO, the fungus invades from the cuticle (the proximal end) and spreads down the nail toward the tip. It appears as a white or yellowish area near the base of the nail.
The presence of PSO is often considered a red flag, as it is strongly associated with a compromised immune system.
It is seen with much higher frequency in patients with conditions like HIV/AIDS, making it a potentially important diagnostic clue for underlying systemic disease.
4. Candida Onychomycosis
Caused by yeast species, primarily Candida albicans, this type of infection often affects fingernails more than toenails.
It frequently occurs in individuals whose hands are often submerged in water (e.g., cleaners, dishwashers) or in nails that have been previously damaged.
The infection can begin at the cuticle, causing swelling, redness, and tenderness of the surrounding skin (a condition called paronychia).
The nail plate itself may then become infected, leading to discoloration and separation from the nail bed.
The Importance of a Professional Diagnosis: It is crucial to understand that not all abnormal-looking nails are caused by fungus. Conditions like nail psoriasis, lichen planus, repeated trauma (e.g., from running), or even, rarely, skin cancers like melanoma can mimic the symptoms of onychomycosis. An incorrect self-diagnosis can lead to ineffective treatments and delay care for a more serious condition. A dermatologist can provide a definitive diagnosis by taking a small sample of the nail for laboratory analysis, such as a microscopic examination with potassium hydroxide (KOH prep) or a fungal culture, to confirm the presence and type of fungus .
Why Me? Uncovering the Causes and Top Risk Factors
A fungal nail infection doesn’t happen by chance.
It results from an encounter with fungal spores in an environment that allows them to take hold and multiply.
While anyone can develop nail fungus, certain factors dramatically increase your susceptibility.
Understanding these risk factors is the first step toward effective prevention.
The core cause is an overgrowth of fungi that enter through tiny, often invisible, cracks in the nail or the surrounding skin.
These fungi are ubiquitous in our environment, but they only cause an infection when conditions are right.
Top Risk Factors for Nail Fungus
Dermatologists point to a combination of physiological, environmental, and lifestyle factors that create the perfect storm for onychomycosis.
- Advancing Age: This is the single most significant risk factor. As we age, blood circulation to the extremities diminishes, and nails grow more slowly and thicken. This slow turnover gives fungi more time to establish an infection. It’s estimated that onychomycosis affects approximately 40% of the elderly population.
- Underlying Health Conditions:
- Diabetes: People with diabetes are at a much higher risk due to a trifecta of issues: compromised circulation, reduced immune response, and potential nerve damage (neuropathy), which can make them less aware of minor foot injuries. Nail fungus in a diabetic patient is a serious concern that can lead to severe complications .
- Poor Circulation: Any condition that impairs blood flow to the feet, such as peripheral artery disease (PAD), makes it harder for the body’s immune system to reach and fight off the infection.
- Weakened Immune System: Conditions like HIV, or the use of immunosuppressant medications (e.g., for organ transplant recipients or autoimmune diseases), lower the body’s natural defenses against fungal invaders.
- Lifestyle and Environment:
- History of Athlete’s Foot (Tinea Pedis): Having a fungal infection on the skin of your feet creates a ready reservoir of fungi that can easily spread to the nails.
- Heavy Sweating (Hyperhidrosis): Perspiring heavily creates a constantly moist environment inside socks and shoes, which is ideal for fungal growth.
- Damp Public Spaces: Walking barefoot in communal areas like gym showers, locker rooms, and swimming pool decks exposes your feet directly to fungi shed by others .
- Occlusive Footwear: Regularly wearing tight, closed-toe shoes (like work boots or athletic sneakers) that don’t allow feet to breathe traps heat and moisture.
- Nail Salons with Poor Hygiene: The use of improperly sterilized or shared tools like clippers, files, and foot baths is a common route of transmission from one client to another.
- Nail Trauma or Injury: A minor injury to the nail or surrounding skin—whether from dropping something on your foot, repetitive trauma from sports (like a runner’s toe), or an overly aggressive pedicure—can create an entry point for fungi to invade .
The Best Nail Fungus Treatments Recommended by Dermatologists
Treating nail fungus is notoriously challenging and requires both patience and a medically sound strategy.
It’s a marathon, not a sprint.
The ultimate goal is not just to kill the existing fungus but to allow a completely new, healthy nail to grow out and replace the damaged one.
This process can take 12 to 18 months for a toenail to grow from base to tip.
A dermatologist will tailor the treatment plan based on the severity of the infection, the type of fungus involved, and the patient’s overall health.
Part 1: Prescription Oral Antifungal Medications (The Gold Standard)
For moderate to severe infections, cases involving multiple nails, or when topical treatments have failed, oral antifungal medications are the most effective option and are considered the gold standard by dermatologists.
These drugs work systemically, traveling through the bloodstream to reach the nail bed and matrix, attacking the fungus from within.
Terbinafine (Lamisil)
Terbinafine is widely regarded as the first-line treatment for dermatophyte-induced onychomycosis due to its high efficacy and favorable safety profile.
It is fungicidal, meaning it actively kills the fungus.
- Efficacy: Clinical studies have shown that terbinafine achieves complete cure rates (both a clear nail and negative lab tests) in a significant number of patients. It is generally considered the most effective oral agent available .
- Treatment Course: The standard regimen for toenail fungus is one 250 mg pill daily for 12 weeks. For fingernails, the duration is typically 6 weeks.
- Key Considerations: While generally safe, terbinafine can, in rare cases, affect the liver. Therefore, dermatologists will typically order a baseline blood test to check liver function before starting the medication and may repeat it during treatment. It is not recommended for patients with chronic liver disease .
Itraconazole (Sporanox)
Itraconazole is another powerful oral antifungal that is effective against both dermatophytes and other fungi like Candida.
It is fungistatic, meaning it stops the fungus from reproducing.
- Treatment Course: Itraconazole can be prescribed in two ways: continuous therapy (one pill daily for 12 weeks) or “pulse” therapy. Pulse dosing involves taking the medication for one week, followed by three weeks off, and repeating this cycle for 3 to 4 months. This method can reduce the total drug exposure and may lower the risk of side effects.
- Key Considerations: Itraconazole has a broader spectrum of potential drug interactions compared to terbinafine and should not be taken with certain medications like some statins. It also requires liver function monitoring and is contraindicated in patients with a history of congestive heart failure or during pregnancy.
Part 2: Prescription Topical Treatments (Applied Directly to the Nail)
Topical treatments are applied directly to the surface of the infected nail.
They are best suited for mild to moderate cases, particularly White Superficial Onychomycosis (WSO) or early-stage DLSO affecting less than 50% of the nail.
They are also a primary option for patients who cannot or prefer not to take oral medications due to potential side effects or drug interactions.
Efinaconazole 10% solution (Jublia)
A newer generation of topical antifungal, efinaconazole was specifically designed for better penetration through the dense keratin of the nail plate.
- Application: It is a solution applied with a brush to the entire nail, the surrounding skin, and under the nail tip once daily for 48 weeks. No nail filing or debridement is required by the patient .
- Efficacy: While cure rates are lower than with oral terbinafine, they represent a significant improvement over older topical agents.
Tavaborole 5% solution (Kerydin)
Tavaborole is another modern topical solution that works by a different mechanism, inhibiting a key fungal enzyme needed for protein synthesis.
- Application: Similar to efinaconazole, it is applied daily to the affected nail for 48 weeks.
Ciclopirox 8% nail lacquer (Penlac)
This is an older, medicated nail polish that has been available for many years.
- Application: The regimen is more demanding. It must be applied daily to the affected nails. Once a week, the accumulated layers of lacquer must be removed with rubbing alcohol, and the nail should be trimmed or debrided . This complexity can affect patient compliance.
Part 3: In-Office Dermatological Procedures (To Boost Treatment Success)
Dermatologists can perform several in-office procedures, often in combination with medication, to increase the likelihood of a cure.
Nail Debridement/Abrasion
This is a simple but effective mechanical procedure where the dermatologist uses a special tool to file or grind down the thickened, infected parts of the nail.
This has two main benefits: it physically removes a large portion of the fungal load, and it thins the nail plate, allowing topical medications to penetrate much more effectively.
Chemical or Surgical Nail Avulsion (Removal)
For severe, painful, or highly resistant infections, removing the nail entirely may be the best option.
This can be done surgically under local anesthesia or chemically, by applying a high-concentration urea ointment to soften the nail over several days until it can be easily lifted off.
Removing the nail eliminates the source of the infection and allows a new, healthy nail to grow in its place, often while the patient is also on an oral or topical antifungal to protect the new growth.
Microdrilling
A relatively new technique, microdrilling involves using a specialized, pen-like drill to create tiny, invisible holes in the nail plate.
These micro-holes act as channels, dramatically increasing the penetration of topical antifungal medications to the nail bed where the infection resides.
Studies have shown this can significantly improve the clearance rates of topical therapies .
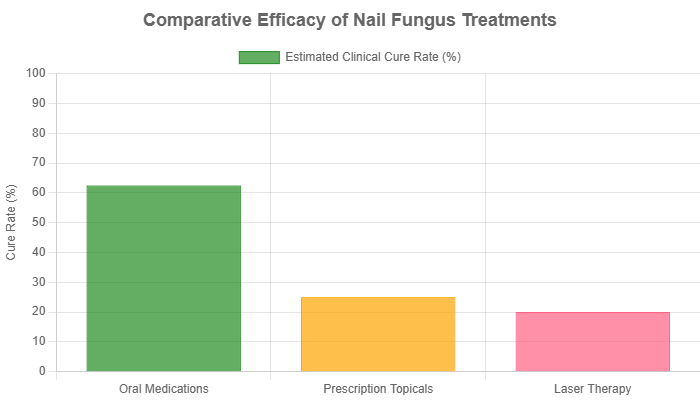
Treatment Comparison: Oral vs. Topical vs. Laser Therapy
Choosing the right treatment for nail fungus can be confusing.
This table provides a clear comparison of the main therapeutic categories to help you understand the options a dermatologist might discuss with you.
| Treatment Type | Efficacy (Clinical Cure Rate) | Typical Duration | Best For | Key Considerations |
|---|---|---|---|---|
| Oral Medications (e.g., Terbinafine) | Highest (50-75%+) | 3-6 months of medication | Moderate to severe infections; multiple nails affected; when a fast and effective cure is prioritized. | Systemic side effects (rare but possible); requires liver function monitoring; potential for drug interactions. Considered the most effective treatment. |
| Prescription Topicals (e.g., Jublia) | Moderate (15-35%) | Up to 12 months of daily application | Mild to moderate infections; single nail involvement; patients who cannot take or wish to avoid oral medications. | Very long treatment duration; requires strict daily compliance; significantly lower cure rates than oral meds; minimal side effects. |
| Laser Therapy | Variable (Evidence is mixed and often weak) | Multiple sessions over 3-6 months | Patients seeking non-drug options or for cosmetic improvement. Often used in combination with other treatments. | High out-of-pocket cost; not typically covered by insurance. The FDA has cleared lasers for temporary cosmetic improvement of nail appearance, not as a definitive “cure” for the fungus itself. |
Home Remedies for Nail Fungus: What Does the Science Say?
The internet is filled with anecdotal claims about home remedies for nail fungus.
While the appeal of a simple, “natural” solution is understandable, it’s crucial to approach these with a healthy dose of skepticism and an understanding of the science.
Dermatologists overwhelmingly agree that for a confirmed onychomycosis infection, home remedies are not a substitute for medical treatment.

Tea Tree Oil
The Claim: Tea tree oil (melaleuca oil) is perhaps the most widely touted natural remedy, praised for its inherent antifungal properties.
The Evidence: While some laboratory (in vitro) studies have shown that tea tree oil can inhibit the growth of dermatophytes, the clinical evidence in humans is very weak.
The primary challenge is penetration; the oil is not effective at getting through the dense nail plate to reach the fungus in the nail bed.
A few small, older studies exist, but their results are not comparable to the efficacy of prescription medications.
Some users on forums like Reddit report trying it, but success stories are rare and often unverified .
Vinegar Soaks (Apple Cider or White)
The Claim: The theory is that the acidic nature of vinegar creates an inhospitable environment for fungus.
The Evidence: This is purely anecdotal.
There are no scientific studies to support the use of vinegar soaks for curing onychomycosis.
Like tea tree oil, vinegar cannot effectively penetrate the nail plate to eradicate the established infection underneath.
It may help with surface issues or odor, but it will not cure the underlying problem.
Vicks VapoRub
The Claim: An unconventional but surprisingly popular remedy.
The active ingredients—camphor, eucalyptus oil, and menthol—are thought to have some antifungal or antiseptic effects.
The Evidence: One very small, preliminary study published in the Journal of the American Board of Family Medicine showed some positive results in a handful of patients.
However, this is far from robust scientific proof. It is not a treatment recommended by dermatologists due to the lack of strong evidence.
The Dermatologist’s Verdict: While these remedies are unlikely to cause significant harm, their main danger lies in delaying proper medical care. Relying on them allows the fungal infection to progress, potentially becoming more severe, spreading to other nails, and making it much harder to treat successfully when you finally seek professional help. For a confirmed infection, evidence-based medical treatment is the only proven path to a cure.
How to Prevent Nail Fungus: A Dermatologist’s Action Plan
Prevention is the best medicine, especially with nail fungus, as reinfection is frustratingly common even after successful treatment.
Adopting a few key habits can significantly reduce your risk of developing a primary infection or experiencing a recurrence.
- Keep Your Feet Meticulously Clean and Dry: Wash your feet with soap and water daily. Afterwards, dry them thoroughly, paying special attention to the spaces between your toes where moisture can linger. Consider using an antifungal foot powder to absorb excess sweat .
- Trim Nails Correctly and Carefully: Keep your toenails trimmed short, cutting them straight across. Smooth the edges with a file. This prevents debris from collecting under the nail and reduces the risk of trauma. Disinfect your clippers with alcohol after each use.
- Choose Breathable Footwear: Opt for shoes made of natural, breathable materials like leather or canvas. Avoid synthetic materials that trap heat and moisture.
- Rotate Your Shoes Daily: Give your shoes at least 24 hours to air out and dry completely before wearing them again. This prevents the buildup of a damp, fungus-friendly environment.
- Treat Your Shoes: Discard old, heavily worn athletic shoes. For other shoes, consider treating them with disinfectant sprays or antifungal powders to kill any lingering fungal spores.
- Wear Protective Footwear in Public Wet Areas: This is non-negotiable. Always wear flip-flops, sandals, or shower shoes in communal showers, gym locker rooms, and around swimming pools.
- Be Smart at the Nail Salon: Choose a salon that visibly uses sterilized tools for each customer (look for instruments coming out of an autoclave pouch). Better yet, bring your own set of clippers and files to prevent cross-contamination .
- Treat Athlete’s Foot Immediately: If you notice any signs of athlete’s foot (itching, scaling, redness between toes), treat it promptly with an over-the-counter antifungal cream. Don’t give the skin infection a chance to spread to your nails.
Frequently Asked Questions (FAQ) About Nail Fungus
Can nail fungus go away on its own?
No. Onychomycosis is a progressive infection that will not resolve without treatment. Fungi are resilient organisms that establish themselves deep within the nail structure. Left untreated, the infection will likely worsen, spread to other nails or the surrounding skin, and become more difficult to cure .
What happens if I leave nail fungus untreated?
Untreated nail fungus can lead to permanent nail damage, thickening that causes pain and difficulty walking, and a distorted appearance. In individuals with diabetes or a weakened immune system, it can create cracks in the skin that allow bacteria to enter, leading to serious secondary infections like cellulitis .
Is nail fungus contagious?
Yes, the fungi that cause onychomycosis are contagious. They can be spread through direct person-to-person contact or, more commonly, through indirect contact with contaminated surfaces like shower floors, towels, socks, or shared nail clippers. It can also spread from one of your own infected nails to your other healthy nails.
Can I wear nail polish to hide the fungus during treatment?
You must ask your dermatologist. It is generally not recommended when using topical treatments, as the polish can create a barrier that prevents the medication from penetrating the nail. It may be permissible when taking oral medications, but it’s always best to get clearance from your doctor .
What is the fastest way to get rid of nail fungus?
The fastest and most effective proven treatments are prescription oral antifungal medications like terbinafine. However, “fast”; is a relative term. While the medication may kill the fungus in 3 months, it still takes 12 to 18 months for the new, healthy nail to fully grow out and replace the damaged nail .
Why does my nail fungus keep coming back?
Reinfection is a common problem. It can occur if the initial treatment course was not completed, if you have not successfully eliminated the fungus from your shoes or home environment (e.g., shower floor), or if you have persistent underlying risk factors like poor circulation or a weakened immune system.
Should I see a dermatologist or a podiatrist for nail fungus?
Both are highly qualified to diagnose and treat nail fungus. Dermatologists are medical doctors who specialize in all diseases of the skin, hair, and nails. Podiatrists are doctors who specialize exclusively in conditions affecting the foot and ankle. Either is an excellent choice for expert care.
Does having diabetes make nail fungus more dangerous?
Absolutely. For people with diabetes, nail fungus is not just a cosmetic issue; it’s a significant health risk. Due to poor circulation, nerve damage, and a compromised immune system, a simple fungal infection can escalate into non-healing foot ulcers and dangerous secondary bacterial infections, potentially leading to amputation. Prompt and aggressive treatment is critical .
Conclusion
Nail fungus is a persistent and often frustrating medical condition, not merely a cosmetic flaw.
While it can be challenging to treat, a definitive cure is achievable for most people.
The key lies in abandoning ineffective home remedies and embracing a scientifically-backed approach guided by a medical professional.
A combination of an accurate diagnosis and dermatologist-prescribed therapies, such as powerful oral medications or advanced topical solutions, offers the highest chance of success.
Remember that patience is a critical component of the treatment, as the true sign of a cure is the slow, steady growth of a new, clear, and healthy nail.
Don’t ignore changes in your nails or allow the infection to progress.
If you suspect you have nail fungus, the single most important step you can take is to schedule an appointment with a board-certified dermatologist.
They can provide a definitive diagnosis, rule out other serious conditions, and create a personalized treatment plan that is both safe and effective for your specific situation.
Taking action today is your best move toward reclaiming the health and appearance of your nails.
Have you successfully treated nail fungus? Share your experience or ask a question in the comments below to help others in the community.

