The best over-the-counter (OTC) treatments for athlete’s foot are antifungal products with active ingredients like terbinafine, clotrimazole and miconazole.
Terbinafine-based creams often work fastest, but the ideal choice depends on your specific symptoms and preferences for creams, sprays or powders.
This persistent, itching, and often frustrating condition, known medically as tinea pedis, is far more common than its name suggests.
It’s not just for athletes. In fact, studies suggest that fungal foot infections affect up to 25% of the global population at any given time, making it one of the most widespread skin infections.
The global market for its treatment was valued at nearly $1.5 billion in 2024, underscoring its prevalence and the demand for effective solutions.
Navigating the pharmacy aisle can be overwhelming, with a dizzying array of options all promising relief.
This guide moves beyond basic definitions to provide a deep, evidence-based analysis of the most effective active ingredients.
We will dissect the science, compare different treatment formats, and offer a step-by-step strategy for choosing the right product and using it for maximum success.
Read on to find a clear path to relieving the itch and curing your athlete’s foot infection for good.
In This Article
Part 1: Understanding the Fungal Foe: Athlete’s Foot Essentials
Before diving into treatments, it’s crucial to understand the adversary.
A clear diagnosis is the first step toward effective treatment.
This section provides the foundational knowledge needed to identify the condition and understand its nature, setting the stage for a targeted therapeutic approach.
What Exactly Is Athlete’s Foot (Tinea Pedis)?
Athlete’s foot is a common fungal infection of the skin on the feet. Its medical name, tinea pedis, reveals its true nature: “tinea” is the classification for a group of fungal skin diseases and “pedis” is Latin for foot.
The condition is caused by a group of fungi called dermatophytes, the same culprits responsible for related infections like ringworm (tinea corporis) and jock itch (tinea cruris).
These microscopic organisms are not a sign of poor hygiene. They are ubiquitous in our environment and thrive in warm, dark, and moist conditions.
This preference explains why the condition is so frequently associated with athletes, who often have sweaty feet confined in tight-fitting shoes for extended periods. However, anyone can contract it.
The infection is contagious and spreads through two primary routes:
- Direct contact: Skin-to-skin contact with an infected person.
- Indirect contact: Walking barefoot on contaminated surfaces, such as locker room floors, public showers, and pool decks. It can also spread by sharing towels, socks, or shoes with someone who has the infection.
Once the fungus takes hold on the skin, it feeds on keratin, a protein found in your skin, hair, and nails, leading to the characteristic symptoms of the infection.
How Do You Know If You Have Athlete’s Foot?
While symptoms can vary from person to person, athlete’s foot typically presents with a distinct set of signs.
Recognizing them early is key to starting treatment promptly and preventing the infection from worsening or spreading.
The infection can affect one or both feet.
Expert Tip: The most common location for athlete’s foot to begin is the moist, tight space between the fourth and fifth (pinky) toes. Always check this area first if you suspect an infection.
Look for the following primary symptoms, which are ideal for self-assessment:
- Intense Itching, Stinging or Burning: This is often the most prominent and bothersome symptom. The sensation is typically most severe right after removing shoes and socks.
- Scaly, Peeling or Cracked Skin: The skin, particularly between the toes, may look flaky and begin to peel away. In more severe cases, painful cracks or fissures can develop.
- Inflamed Skin: The affected area may appear red, purplish, or grayish, depending on your natural skin tone. This inflammation is a direct result of the body’s response to the fungal invasion.
- Blisters: Some types of athlete’s foot can cause small, painful blisters (vesicles), which may sometimes break and ooze fluid.
- Dry, Scaly Skin on the Sole (Moccasin-type): A less common form of the infection presents as chronic dryness and scaling that covers the bottom of the foot and may extend up the sides, resembling a moccasin. This type can be mistaken for simple dry skin but is often more persistent.
If your symptoms align with this profile, it is highly likely you are dealing with athlete’s foot and can proceed with an over-the-counter treatment plan.
However, as we will discuss later, certain conditions warrant a visit to a healthcare professional.
Part 2: The Ultimate Guide to OTC Athlete’s Foot Treatments
This is the heart of our guide. Here, we move from identifying the problem to actively solving it.
We will dissect the active ingredients in popular OTC products, compare their mechanisms of action, and provide a clear framework for selecting the best treatment for your specific needs.
This evidence-based approach is designed to empower you to make an informed decision in the pharmacy aisle.
What Are the Most Effective OTC Active Ingredients for Athlete’s Foot?
Not all antifungal creams are created equal. The active ingredient is the single most important factor determining a product’s effectiveness and treatment duration.
OTC antifungals primarily fall into two major classes: allylamines and azoles.
Understanding the difference is key to choosing the most powerful weapon against your fungal infection.
The Allylamines: The Fungus Killers (Terbinafine, Butenafine)
Allylamine antifungals are considered the gold standard by many dermatologists for a simple reason: they are fungicidal.
This means they actively kill the fungal cells by inhibiting an enzyme called squalene epoxidase, which is essential for the fungus to create its cell membrane.
Without a stable cell membrane, the fungus dies.
Terbinafine 1% (found in Lamisil AT): Terbinafine is arguably the most well-researched and effective OTC ingredient for athlete’s foot treatment. Its key advantage is its ability to achieve a cure in a significantly shorter time frame.
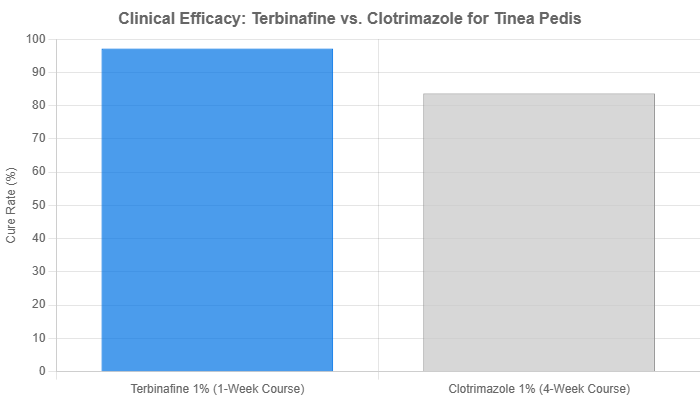
A landmark multicenter study published in the British Medical Journal directly compared a one-week course of terbinafine cream with a four-week course of clotrimazole cream (an azole).
The results were definitive. At the six-week follow-up, the mycological cure rate (meaning no fungus was detectable by microscope or culture) was 97.2% for the terbinafine group compared to 83.7% for the clotrimazole group.
This demonstrates that not only is terbinafine highly effective, but it can achieve superior results with a much shorter treatment duration.
Butenafine 1% (found in Lotrimin Ultra): Butenafine is another powerful fungicidal allylamine. It functions similarly to terbinafine and is also known for its rapid action and high cure rates.
Some studies suggest it may have a longer-lasting effect in the skin after application, providing a sustained antifungal action. It is an excellent alternative to terbinafine and is often recommended for stubborn or persistent infections.
The Azoles: The Fungus Stoppers (Clotrimazole, Miconazole)
Azole antifungals are fungistatic.
This means they don’t directly kill the fungus but instead inhibit its growth and reproduction.
They work by disrupting the production of ergosterol, another critical component of the fungal cell membrane.
By halting the fungus’s ability to multiply, azoles give your body’s immune system the upper hand to clear the existing infection.
Clotrimazole 1% (found in Lotrimin AF, many generic brands): Clotrimazole is one of the most widely used and trusted OTC antifungals. It has a long track record of safety and effectiveness for treating athlete’s foot, jock itch and ringworm.
While highly effective, its fungistatic nature means it typically requires a longer treatment course—usually two to four weeks—to ensure the infection is fully eradicated.
Miconazole 2% (found in Micatin, Desenex, various store brands): Miconazole is another veteran azole antifungal, very similar in function and efficacy to clotrimazole.
It is a reliable and cost-effective choice that has been a mainstay of OTC fungal treatment for decades. Like clotrimazole, consistent application over a four-week period is generally recommended for best results.
Other Key Ingredients (Tolnaftate)
Tolnaftate 1% (found in Tinactin, Lamisil AF Defense): Tolnaftate is in a different chemical class (thiocarbamates) but functions similarly to azoles in that it is primarily fungistatic. While it is effective at curing most cases of athlete’s foot, it is particularly well-regarded for its role in prevention.
Its formulation in powders and sprays makes it an excellent choice for daily use to keep feet dry and prevent the fungus from taking hold again after an active infection has been cleared.
Key Takeaway: For the fastest cure, choose a fungicidal allylamine like terbinafine or butenafine. For a reliable, time-tested treatment, or if cost is a primary concern, a fungistatic azole like clotrimazole or miconazole is an excellent choice, provided you commit to the full treatment duration.
Creams, Sprays, or Powders: Which Athlete’s Foot Treatment Form Is Right for You?
Once you’ve chosen an active ingredient, the next decision is the application format.
This choice is not just about personal preference, the right format can enhance the treatment’s effectiveness based on your specific symptoms and lifestyle.
This is where the “Experience” aspect of E-E-A-T comes into play—understanding the practical nuances of treatment.
Antifungal Creams: For Targeted, Potent Application
Best for: Active, symptomatic infections, especially those with significant scaling, cracking or inflammation.
Creams are the workhorses of athlete’s foot treatment. They deliver a concentrated dose of the active ingredient directly to the affected skin.
Their emollient base also provides a secondary benefit: it helps to moisturize and soften the dry, cracked skin associated with the infection, which can reduce discomfort and help the medication penetrate more effectively.
This makes them the top choice for treating the most common interdigital (between the toes) type of athlete’s foot.
Antifungal Sprays: For Quick, No-Touch Coverage
Best for: Covering large areas (like the entire sole in moccasin-type infections), hard-to-reach spots, and for individuals who prefer a no-mess, quick-drying application.
Sprays offer convenience and speed. A quick spray can cover the entire foot in seconds without you ever having to touch the infected area, which can help prevent spreading the fungus to your hands. They are also excellent for treating the inside of shoes, a critical step in preventing reinfection. Both liquid and powder sprays are available.
Antifungal Powders: For Keeping Feet Dry and Preventing Recurrence
Best for: Very mild cases, managing moisture during and after treatment and ongoing daily prevention.
The primary strength of antifungal powder is its ability to absorb moisture. Since dermatophytes thrive in damp environments, keeping your feet and the inside of your shoes dry is a cornerstone of both treatment and prevention. While a powder alone may not be potent enough to clear a moderate to severe infection, it is an indispensable tool for preventing recurrence.
After you’ve cured an infection with a cream or spray, daily use of an antifungal powder in your socks and shoes is your best long-term strategy.
How Do the Top OTC Athlete’s Foot Brands Compare?
To synthesize this information into a practical, actionable tool, here is a comparative table of the leading OTC athlete’s foot treatments.
This table is designed to be a quick-reference guide to help you make a confident choice at the store.
| Brand Name | Active Ingredient | Class (Mechanism) | Typical Treatment Duration | Best For… |
|---|---|---|---|---|
| Lamisil AT Cream | Terbinafine 1% | Fungicidal (Allylamine) | 1-2 weeks | Fastest-acting relief for itching and burning, especially for infections between the toes. The clinical evidence leader. |
| Lotrimin Ultra Cream | Butenafine 1% | Fungicidal (Allylamine) | 2 weeks | A potent, fast-acting alternative to terbinafine, excellent for stubborn or persistent cases of athlete’s foot. |
| Lotrimin AF Cream | Clotrimazole 1% | Fungistatic (Azole) | 2-4 weeks | A reliable, all-purpose, and often more affordable treatment for most common cases. The time-tested standard. |
| Micatin / Generic Miconazole | Miconazole 2% | Fungistatic (Azole) | 4 weeks | A highly effective and widely available azole treatment. A dependable choice requiring full 4-week commitment. |
| Tinactin Powder/Spray | Tolnaftate 1% | Fungistatic | 4 weeks | Curing most athlete’s foot and is particularly excellent for daily use in shoes and socks for moisture control and prevention of recurrence. |
Part 3: Maximizing Your Treatment and Preventing Recurrence
Choosing the right product is only half the battle. Proper application and a commitment to preventative care are what separate a temporary fix from a permanent cure.
This section provides the practical, actionable advice needed to ensure your treatment is successful and the infection doesn’t return.
How Do You Apply Athlete’s Foot Treatment for Maximum Success?
Following a precise application protocol is critical for eradicating the fungus.
Skipping steps or stopping treatment too early is the number one reason for treatment failure and recurrence.
Follow this five-step process for maximum success.
- Start with Clean, Dry Feet: Before every application, wash your feet with soap and warm water. Afterward, dry them thoroughly. Use a separate, clean towel and pay special attention to drying the spaces between your toes, as this is where moisture loves to hide.
- Apply a Thin, Even Layer: You don’t need to glob on the cream. Squeeze out a small amount (about the size of a pea for one foot) and gently massage it into the affected skin until it is absorbed. A thin layer is all that’s needed.
- Extend Beyond the Visible Rash: This is a crucial expert tip. The fungus often extends beyond the visible signs of the rash. To ensure you are targeting the entire infected zone, apply the treatment to the rash itself and to about a one-inch border of the surrounding healthy-looking skin.
- Do Not Stop Early: This cannot be overemphasized. You must continue using the medication for the full duration recommended on the product packaging, even if your symptoms (like itching and redness) disappear within a few days. The fungus can linger on the skin long after symptoms have subsided. Stopping early almost guarantees a relapse.
- Treat Your Environment: After applying the medication, wash your hands thoroughly with soap and water to avoid spreading the fungus. To prevent reinfecting yourself, treat your shoes with an antifungal spray or powder and allow them to air out.
Can Home Remedies Actually Cure Athlete’s Foot?
A quick search online reveals dozens of purported home remedies for athlete’s foot, from vinegar soaks to essential oils.
But do they actually work? Here, we look at the science to provide a balanced and trustworthy perspective.
What the Science Says About Tea Tree Oil and Vinegar Soaks
It’s true that some natural compounds have antifungal properties.
Tea tree oil, in particular, has been the subject of several studies.
As noted by sources like GoodRx Health, some research suggests that solutions with 25-50% tea tree oil can improve symptoms.
However, a comprehensive systematic review from the Cochrane Database, a highly respected source for medical evidence, found that tea tree oil was not statistically more effective than a placebo for achieving a mycological cure.
Similarly, vinegar soaks (using apple cider or white vinegar) are thought to work by creating an acidic environment that is inhospitable to fungus.
While they may help to dry out the skin and reduce symptoms, there is no robust clinical evidence to support their use as a standalone cure.
The Verdict: Home remedies like tea tree oil and vinegar soaks are best viewed as supplementary therapies. They may help soothe symptoms and can be used alongside a proven OTC antifungal, but they are not a reliable substitute for FDA-approved medications for curing a moderate to severe athlete’s foot infection.
Why Prevention is Your Best Long-Term Strategy
Ultimately, the most effective “cure” for athlete’s foot is to create an environment where it can’t survive.
This means adopting a consistent foot hygiene routine.
These preventative measures are your best defense against recurrence.
- Keep Your Feet Dry: Dry your feet thoroughly after every shower, bath, or swim. Use antifungal powder daily.
- Change Your Socks Daily: Put on a fresh pair of socks every day, or more often if your feet get sweaty. Choose moisture-wicking materials like merino wool or synthetic blends over cotton.
- Alternate Your Shoes: Avoid wearing the same pair of shoes two days in a row. This gives them at least 24 hours to dry out completely.
- Protect Your Feet in Public: Always wear waterproof sandals or shower shoes in public locker rooms, showers, and around swimming pools.
- Don’t Share: Never share towels, socks, or shoes with others.
- Let Your Feet Breathe: Whenever possible at home, go barefoot to allow your feet to air out.
Part 4: When OTC Treatments Aren’t Enough
Over-the-counter treatments are highly effective for the vast majority of athlete’s foot cases.
However, there are specific situations where self-treatment is not appropriate and professional medical advice is necessary.
Recognizing these red flags is critical for your health and safety, a cornerstone of building Trustworthiness.
When Should You See a Doctor for Athlete’s Foot?
Consult a physician, podiatrist, or dermatologist if you encounter any of the following situations.
Do not delay seeking care, especially if you have underlying health conditions.
- No Improvement After Treatment: If you have been using an OTC product consistently and correctly for the recommended duration (typically 2-4 weeks) and see no improvement, it’s time to see a doctor. The infection may be caused by a resistant strain of fungus or it may not be a fungal infection at all (conditions like psoriasis or eczema can mimic athlete’s foot).
- The Infection is Severe or Worsening: If the rash is spreading rapidly, covers a large area of your foot, or is causing extreme pain and discomfort, professional intervention is needed.
- Signs of a Secondary Bacterial Infection: Scratching the itchy rash can create breaks in the skin, allowing bacteria to enter and cause a secondary infection. Signs include excessive redness, swelling, warmth, the formation of pus, or a fever. This requires antibiotics and must be treated by a doctor.
- You Have a Compromising Medical Condition: If you have diabetes, a compromised immune system (due to HIV/AIDS, chemotherapy, or immunosuppressant drugs), or poor circulation, you should see a doctor at the first sign of any foot problem. For these individuals, even a minor infection like athlete’s foot can lead to serious complications.
- The Infection Spreads to Your Toenails: If you notice your toenails becoming thick, discolored (yellow or brown), and brittle, the fungus has likely spread to the nail bed. This condition, called onychomycosis, is notoriously difficult to treat and almost always requires prescription-strength oral or topical medications. OTC products are not effective for nail fungus.
Part 5: Frequently Asked Questions (FAQ)
This section provides quick, direct answers to the most common questions people have about athlete’s foot and its treatment.
These are optimized to provide immediate value and capture long-tail search queries.
Frequently Asked Questions About Athlete’s Foot Treatment
1. Is athlete’s foot contagious?
Yes, athlete’s foot is highly contagious. It spreads easily through direct skin-to-skin contact or by touching contaminated surfaces like floors, towels, and shoes. It’s important to avoid sharing personal items and to protect your feet in public wet areas.
2. How long does it take for athlete’s foot treatment to work?
Symptom improvement, such as reduced itching, can often be felt within a few days of starting treatment. However, a complete mycological cure takes longer. Expect to treat for 1-2 weeks with a terbinafine product or 2-4 weeks with an azole product like clotrimazole.
3. What’s the difference between Lotrimin AF and Lotrimin Ultra?
The key difference is the active ingredient. Lotrimin AF contains clotrimazole, a fungistatic azole. Lotrimin Ultra contains butenafine, a more potent, fungicidal allylamine that often works faster. Both are effective, but Ultra is designed for a quicker cure.
4. Can I use athlete’s foot cream for jock itch or ringworm?
Often, yes. These infections are caused by the same family of fungi (dermatophytes). Most products containing terbinafine, clotrimazole, or miconazole are approved for all three conditions. However, always check the product label to confirm its intended uses before applying.
5. Can athlete’s foot come back after treatment?
Yes, recurrence is very common. This usually happens if you don’t complete the full treatment course or if you don’t eliminate the fungus from your environment. Diligently treating your shoes and socks and practicing good preventative foot hygiene is essential to keep it from returning.
6. Should I wear socks to bed with athlete’s foot?
Yes, wearing clean, breathable cotton socks to bed is a good idea. It can help absorb moisture overnight and, more importantly, can help prevent you from spreading the fungal spores to your bedding, which could otherwise become a source of reinfection for you or your partner.
7. How do I clean my shoes to prevent reinfection?
Use a dedicated antifungal spray or powder inside your shoes after each wear. Allow them to air dry completely for at least 24 hours before wearing them again. Alternating between two or more pairs of shoes is the most effective strategy to ensure they are always dry.
8. Is terbinafine (Lamisil) really better than clotrimazole (Lotrimin)?
Clinical studies, like the one cited from the British Medical Journal, suggest terbinafine is often faster and achieves a slightly higher cure rate in a shorter time. However, both are proven, FDA-approved, and highly effective treatments when used as directed.
Conclusion
Conquering athlete’s foot is an achievable goal when armed with the right knowledge and tools.
We’ve established that while the condition is common, effective relief is readily available over-the-counter.
The most critical takeaway is that the active ingredient dictates the treatment’s speed and mechanism.
For faster, fungicidal action, allylamines like terbinafine (Lamisil AT) and butenafine (Lotrimin Ultra) are clinically proven top choices.
For a reliable and cost-effective approach, fungistatic azoles like clotrimazole (Lotrimin AF) and miconazole remain excellent options.
The choice between a cream, spray, or powder should be guided by your specific symptoms—creams for targeted treatment of cracked skin, sprays for convenient coverage, and powders for essential moisture control and prevention.
Remember, success hinges on two non-negotiable principles: completing the full treatment course even after symptoms fade, and embracing a long-term preventative strategy centered on keeping your feet clean, dry, and protected.
Stop the itch and reclaim your comfort. Use this guide to confidently select the right OTC treatment and take the first step toward healthy, fungus-free feet today.
Have you had success with a particular treatment? Do you have more questions? Share your experiences and thoughts in the comments section below to help our community.
Reference
[1] https://www.webmd.com/skin-problems-and-treatments/understanding-athletes-foot-basics
[2] https://www.mayoclinic.org/diseases-conditions/athletes-foot/symptoms-causes/syc-20353841

