Treating thrush in adults primarily involves antifungal medications, such as nystatin or fluconazole, which eliminate the overgrowth of the Candida fungus.
The specific treatment and duration depend on the infection’s severity and the individual’s overall health.
While Candida is a normal inhabitant of the mouth, its overgrowth into thrush is a significant issue, affecting up to 31% of older adults and a majority of individuals with compromised immune systems, according to recent studies.
This condition, while often minor in healthy individuals, can cause significant discomfort and may signal a deeper, underlying health problem.
This definitive guide will walk you through everything you need to know about adult thrush.
We’ll explore the root causes, how to get a proper diagnosis, provide a deep dive into all available treatment options—from first-line medical therapies to supportive home care—and share expert strategies for preventing frustrating recurrences.
Continue reading to gain the knowledge you need to effectively manage and eliminate thrush.
In This Article
Understanding Thrush: The “Why” Behind the White Patches
Before diving into treatment, it’s crucial to understand what oral thrush is and why it appears. It’s not an infection you “catch” in the traditional sense but rather an internal imbalance.
Understanding this fundamental concept is the first step toward effective, long-term management.
What Exactly Is Thrush (Oral Candidiasis)?
Oral thrush, known in the medical community as oral candidiasis, is a fungal infection of the mouth. It is caused by an overgrowth of a type of yeast called Candida.
The most common culprit is a species named Candida albicans, which is responsible for over 80% of cases, as noted in research published by the National Center for Biotechnology Information (NCBI).
It’s important to realize that Candida is a normal, harmless resident of the oral microbiome in about 30-60% of healthy adults. It coexists peacefully with trillions of other microorganisms, including beneficial bacteria.
Think of your mouth as a complex garden: the beneficial bacteria are the healthy plants that keep the ecosystem in check.
Thrush occurs when this balance is disrupted—when the “good plants” are weakened or removed, allowing the opportunistic “weeds” (Candida) to grow out of control.
This overgrowth can manifest in several ways, including:
- Pseudomembranous Candidiasis: The classic form, presenting as the well-known creamy white, cottage cheese-like patches that can be wiped away.
- Erythematous (Atrophic) Candidiasis: A red, raw-looking form, often appearing on the palate or tongue after a course of antibiotics.
- Hyperplastic Candidiasis: A less common form with stubborn white plaques that cannot be easily scraped off.
Is adult thrush contagious? Generally, no. For healthy adults, passing thrush through kissing or sharing utensils is highly unlikely. The fungus is already present in most people. However, as the Cleveland Clinic explains, it can be transmitted in specific situations, such as from a mother to her baby during breastfeeding or between individuals who are both immunocompromised.
What Causes Thrush to Develop in Adults?
The development of thrush in an otherwise healthy adult is uncommon and often serves as a red flag for an underlying issue.
The triggers that disrupt the oral microbiome and allow Candida to flourish can be grouped into three main categories.
Medication-Induced Thrush
Many common medications are primary culprits in triggering a thrush outbreak.
They alter the body’s natural defenses, creating a perfect opportunity for yeast overgrowth.
- Antibiotics: Broad-spectrum antibiotics are a leading cause. While they are essential for fighting bacterial infections, they don’t distinguish between harmful and beneficial bacteria. By wiping out the good bacteria that keep Candida in check, they leave the door wide open for a fungal takeover.
- Corticosteroids: Both inhaled and oral corticosteroids can lead to thrush. Inhaled steroids (used for asthma or COPD) can suppress the local immune response in the mouth and throat. Oral steroids (like prednisone) suppress the entire immune system. An essential expert tip: The Mayo Clinic strongly advises rinsing your mouth with water or brushing your teeth immediately after using a corticosteroid inhaler to remove any residual medication.
- Birth Control Pills: Hormonal fluctuations, particularly those caused by oral contraceptives, can alter the environment in the mouth and other mucous membranes, potentially encouraging yeast growth.
Underlying Health Conditions
Your oral health is a mirror of your systemic health.
Several chronic conditions are strongly associated with an increased risk of developing thrush.
- Weakened Immune Systems: This is the most significant risk factor. Conditions like HIV/AIDS, which directly attack the immune system, make individuals highly susceptible. Similarly, treatments for cancer, such as chemotherapy and radiation, suppress immune function, making thrush a common side effect.
- Uncontrolled Diabetes: People with poorly managed diabetes often have high levels of sugar in their saliva. This excess sugar acts as a food source for Candida, fueling its rapid growth. For many, recurrent thrush is one of the first signs that their blood sugar is not under control.
- Dry Mouth (Xerostomia): Saliva is more than just water, it contains antifungal and antibacterial compounds and helps wash away debris. Conditions or medications that cause dry mouth reduce this natural protective mechanism, allowing yeast to adhere to tissues and multiply.
Lifestyle and Other Factors
- Dentures: Denture wearers, particularly those with ill-fitting upper dentures, are at high risk. The denture can trap moisture and food particles, creating a warm, dark, and moist environment where Candida thrives. This condition is specifically known as denture stomatitis.
- Smoking: Tobacco use damages the mucosal lining of the mouth, making it more vulnerable to infection. It also alters the oral microbiome, favoring the growth of pathogenic organisms like Candida.
From Symptoms to Diagnosis: Identifying and Confirming Thrush
Recognizing the signs of thrush early is key to getting prompt treatment and avoiding discomfort.
While the classic white patches are well-known, other, more subtle symptoms can also indicate an infection.
Understanding the full spectrum of symptoms and the diagnostic process empowers you to seek appropriate care.
What Are the Common Symptoms of Oral Thrush?
The presentation of oral thrush symptoms can vary from person to person, depending on the severity of the infection and the individual’s overall health. Here are the most common signs to watch for, which are ideal for quick identification:
- Classic Signs:
- Creamy white patches on the tongue, inner cheeks, gums, or tonsils, often described as looking like cottage cheese.
- Underlying tissue that is red, inflamed, and sore.
- Slight bleeding if the white patches are rubbed or scraped while brushing or eating.
- Subtle & Sensory Symptoms:
- A strange, cotton-like or dry feeling in the mouth.
- A partial or complete loss of taste (ageusia).
- Pain, burning, or general discomfort, especially when eating or swallowing.
- Advanced Symptoms:
- Cracking, redness, and soreness at the corners of the mouth, a condition known as angular cheilitis.
- If the infection spreads down the esophagus (Candida esophagitis), you may experience a feeling of food getting stuck in your throat or chest, along with pain upon swallowing. This is a serious complication that requires immediate medical attention.
How Do Doctors Diagnose Thrush?
If you suspect you have thrush, a visit to your doctor or dentist is essential for a proper diagnosis.
While it may seem obvious, other conditions can mimic its appearance, making professional evaluation critical.
The Initial Assessment
In most cases, a healthcare provider can diagnose thrush through a simple clinical examination.
They will look at the characteristic white lesions inside your mouth and ask about your symptoms and medical history, including any recent medication use (especially antibiotics or steroids) and underlying health conditions (like diabetes).
A key diagnostic clue is that the white plaques of pseudomembranous candidiasis can typically be scraped away, revealing a red, inflamed, and sometimes slightly bleeding base.
This helps distinguish it from other white lesions.
Confirmatory Tests
While a visual exam is often sufficient, your doctor may perform additional tests in certain situations, such as for recurrent infections, cases that don’t respond to initial treatment, or to rule out other conditions.
- KOH Smear: This is a simple, quick, and common test. The provider will gently scrape a small sample from a lesion onto a microscope slide, add a drop of potassium hydroxide (KOH), and examine it under a microscope. The KOH solution dissolves human cells, making the characteristic yeast cells and hyphae (branching filaments) of Candida clearly visible.
- Fungal Culture: If an infection is persistent or severe, a culture may be necessary. A swab from the mouth is sent to a lab to grow the fungus. This can identify the specific species of Candida causing the infection (e.g., C. albicans vs. a more resistant species like C. glabrata) and can be used to test which antifungal medications will be most effective.
- Endoscopy: If there are symptoms suggesting the infection has spread to the esophagus (like pain with swallowing), your doctor will refer you for an endoscopy. A thin, flexible tube with a camera is passed down your throat to visualize the esophagus and take tissue samples if needed.
Differential Diagnosis: Why a Professional Opinion Matters. It’s crucial not to self-diagnose because several other conditions can cause white patches or soreness in the mouth. A professional can differentiate thrush from conditions like leukoplakia (a precancerous condition), lichen planus (an inflammatory condition) or even simple food debris. An accurate diagnosis ensures you receive the correct and most effective thrush treatment.
The Definitive Guide to Thrush Treatment
This section forms the core of our guide, providing a comprehensive overview of every effective thrush treatment available for adults.
The goal of treatment is twofold: first, to eliminate the fungal overgrowth, and second, to address the underlying cause to prevent it from returning.
We will cover first-line medical therapies, evidence-based supportive care, and specialized protocols for different patient groups.
What Are the Main Medical Treatments for Thrush?
Antifungal medications are the cornerstone of treating oral thrush. They work by killing the Candida fungus or stopping its growth.
The choice of medication depends on the severity of the infection and the patient’s overall health.
According to the Centers for Disease Control and Prevention (CDC), treatment typically lasts for 7 to 14 days.
Topical Antifungals (First-Line for Mild to Moderate Cases)
Topical treatments are applied directly to the affected area in the mouth.
They have fewer side effects than systemic drugs because they are minimally absorbed into the bloodstream. They are the preferred choice for uncomplicated thrush.
- Nystatin (Liquid Suspension): This is a classic “swish and swallow” or “swish and spit” medication. You hold the liquid in your mouth, swishing it thoroughly to coat all surfaces for several minutes before swallowing or spitting it out as directed by your doctor.
- Clotrimazole (Troches/Lozenges): These are small tablets designed to be dissolved slowly in the mouth over 15-30 minutes. This prolonged contact time allows the medication to work effectively on the oral tissues.
- Miconazole (Buccal Tablet): This is a modern, convenient option. It’s a tablet that you place on your upper gum once a day. It adheres to the gum and slowly releases medication over several hours, providing continuous antifungal action.
Systemic Antifungals (Oral Pills for More Severe Cases)
For moderate-to-severe infections, cases that don’t respond to topical therapy, or for individuals with weakened immune systems, a doctor will prescribe an oral antifungal pill.
These medications are absorbed into the bloodstream and fight the infection systemically.
- Fluconazole (Diflucan): This is the most commonly prescribed and highly effective oral medication for thrush. It is usually taken once daily. A comparative efficacy study published in PMC found fluconazole to be one of the most effective agents for achieving a clinical cure.
- Itraconazole (Sporanox): This is another oral azole antifungal used as an alternative, particularly if the Candida species is resistant to fluconazole. Its absorption can be more variable than fluconazole’s.
Comparison of Common Thrush Medications
To help you understand the options, here is a comparative table of the most common antifungal treatments for oral thrush.
| Medication Name | Type | How It’s Used | Best For | Key Considerations |
|---|---|---|---|---|
| Nystatin | Topical (Liquid) | Swish in mouth for several minutes, 4-5 times daily. | Mild to moderate thrush, especially in infants. | Can have an unpleasant taste. High sugar content may be a concern for diabetics. Requires frequent dosing. |
| Clotrimazole | Topical (Lozenge) | Dissolve slowly in mouth, 5 times daily. | Mild to moderate thrush. | Provides prolonged contact time. Also contains sugar. Multiple daily doses can be inconvenient. |
| Miconazole | Topical (Buccal Tablet) | Apply one tablet to the upper gum once daily. | Mild to moderate thrush. | Very convenient (once-daily). May interact with other drugs like warfarin. |
| Fluconazole | Systemic (Oral Pill) | Take one pill by mouth, once daily. | Moderate to severe thrush, recurrent infections, immunocompromised patients. | Highly effective and convenient. Can have drug interactions and, rarely, liver side effects. The go-to for serious cases. |
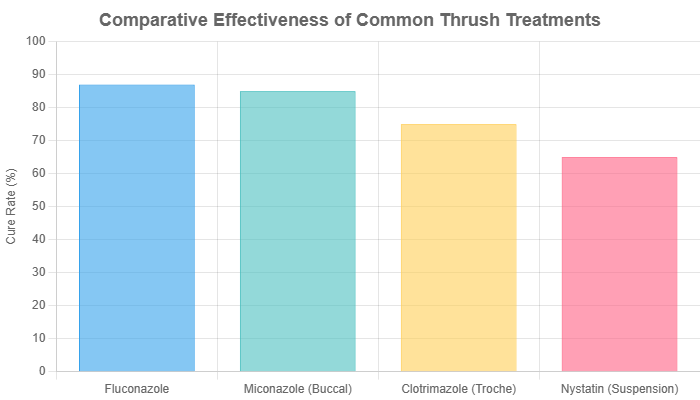
Figure 1: Estimated clinical cure rates for oropharyngeal candidiasis based on a meta-analysis. Data adapted from studies like Rajadurai et al. (2021) in PMC. Rates are illustrative of general effectiveness.
Are There Evidence-Based Home Remedies for Thrush?
Crucial Disclaimer: The following home remedies should be considered supportive care only. They can help soothe symptoms and support oral health but are not a substitute for prescribed antifungal medication, which is necessary to cure the infection. Always consult your doctor before trying any home remedies.
While medication is essential, certain home practices can help manage discomfort and create a less hospitable environment for Candida.
Effective Supportive Rinses
- Salt Water Rinse: This is a time-tested remedy for oral discomfort. Mix 1/2 teaspoon of salt in 1 cup of warm water and swish gently for 30-60 seconds before spitting it out. As Healthline notes, salt has antiseptic properties that can help cleanse the mouth and soothe inflamed tissues.
- Baking Soda Rinse: Mix 1/2 teaspoon of baking soda (sodium bicarbonate) in 1 cup of warm water. Research has shown that baking soda can inhibit the growth of Candida albicans and may help restore a healthy pH balance in the mouth.
Probiotics
The theory behind using probiotics is to help restore the population of “good” bacteria in your oral microbiome, which can then compete with Candida. You can incorporate probiotics by:
- Eating unsweetened yogurt with live and active cultures. Choose plain varieties, as sugar feeds yeast.
- Taking a probiotic supplement. Look for supplements containing strains like Lactobacillus.
What to Be Cautious About
Many other remedies are popularly discussed online, but they should be approached with caution.
Rinses with apple cider vinegar or diluted essential oils (like tea tree or oregano oil) may have antifungal properties in a lab setting, but they can also be highly acidic or irritating to the already-sore tissues in your mouth.
Never apply anything acidic or undiluted essential oils directly to thrush lesions, as this can cause significant pain and burning.
How Is Thrush Treated in Special Populations?
Effective thrush treatment requires a tailored approach, as what works for a healthy adult may not be appropriate for someone with other health considerations.
This nuanced understanding is a hallmark of expert care.
Denture Wearers (Denture Stomatitis)
For those with dentures, the protocol is clear: “treat the patient, treat the denture”.
Simply treating the mouth is not enough, as the denture can act as a reservoir for the fungus, leading to immediate reinfection.
- Treat the Mouth: Use prescribed antifungal medication as directed.
- Treat the Denture: The denture must be disinfected. Remove it at night (for at least 6-8 hours) and soak it in an appropriate solution. Options include chlorhexidine gluconate (with a dentist’s recommendation) or other commercial denture cleansers.
- Improve Fit: See a dentist to ensure the denture fits properly, as poor fit can cause irritation and create spaces for yeast to grow.
Immunocompromised Patients (e.g., HIV/Cancer)
These individuals are at high risk for severe and recurrent thrush. Treatment is often more aggressive.
- Systemic Therapy is Key: Oral fluconazole is typically the first-line treatment, as topical agents may not be sufficient.
- Longer Duration: Treatment courses are often longer than the standard 7-14 days.
- Suppressive Therapy: For those with frequent, debilitating recurrences, a doctor may prescribe a low, long-term maintenance dose of an antifungal (prophylactic therapy) to prevent future outbreaks. This is a decision made carefully, balancing the benefits against the risk of developing drug resistance.
The Elderly
Treating older adults presents unique challenges due to comorbidities, polypharmacy (the use of multiple medications) and potential physical limitations.
A doctor will need to check for drug interactions between antifungals and other medications.
Furthermore, if a patient has difficulty with “swish and swallow” techniques due to cognitive or motor issues, an oral pill like fluconazole may be a much more practical and effective option.
Pregnancy
During pregnancy, especially the first trimester, systemic azole antifungals like fluconazole are generally avoided due to potential risks to the developing fetus.
Therefore, as outlined in the StatPearls guide on Oral Candidiasis, topical treatments like clotrimazole troches or nystatin suspension are the preferred and safer choice.
Preventing Recurrence and Long-Term Management
Curing a single episode of thrush is one thing, preventing it from coming back is another.
For many, the frustration lies in recurrent infections.
Long-term management focuses on shifting from reactive treatment to proactive prevention by addressing the root causes.
How Can I Stop Thrush from Coming Back?
Preventing recurrent thrush is not about finding a magic pill but about restoring and maintaining balance in your body.
This requires a multi-faceted, sustainable strategy.
1. Address the Root Cause (The Most Critical Step)
This is the absolute cornerstone of prevention.
If you don’t fix the underlying issue that allowed the yeast to overgrow in the first place, thrush will almost certainly return. This means working with your healthcare provider to:
- Control Blood Sugar: If you have diabetes, consistently maintaining your blood glucose levels within the target range is paramount.
- Review Medications: Discuss with your doctor if any of your medications (like antibiotics or steroids) could be contributing. Sometimes, an alternative medication or a different delivery method (e.g., using a spacer with an inhaler) can help.
- Manage Immune Conditions: If you have a condition that weakens your immune system, adhering to your overall treatment plan is crucial for preventing opportunistic infections like thrush.
2. Optimize Oral Hygiene
Excellent oral hygiene creates an environment where it’s harder for Candida to thrive.
- Brush and Floss: Brush your teeth at least twice a day with a soft-bristled brush and floss daily.
- Replace Your Toothbrush: It’s a wise practice to get a new toothbrush after you’ve recovered from a thrush infection to avoid reintroducing a high concentration of the fungus into your mouth.
- Regular Dental Visits: See your dentist for regular check-ups and cleanings. They can spot early signs of trouble and provide professional advice on oral care and denture hygiene.
3. Dietary Considerations
While the evidence for a strict “anti-Candida diet” is limited and debated, some general dietary principles may be helpful.
Since yeast feeds on sugar, it is logical that limiting your intake of certain foods could be beneficial.
- Limit Sugar and Refined Carbs: Reducing your intake of sugary drinks, sweets, and highly processed foods with refined flour is good for your overall health and may help by not providing an easy food source for yeast.
- Incorporate Probiotic Foods: As mentioned earlier, unsweetened yogurt and other fermented foods can help support a healthy gut and oral microbiome.
4. Prophylactic (Preventive) Therapy
In very specific cases, such as for severely immunocompromised individuals who suffer from constant, severe thrush, a doctor might prescribe a long-term, low-dose antifungal.
This is not a standard approach and is reserved for high-risk patients due to concerns about cost, side effects, and the potential for developing drug-resistant strains of Candida.
What Should I Eat and Drink During a Thrush Outbreak?
When your mouth is sore and inflamed from a thrush outbreak, eating can be a painful experience.
Choosing the right foods can help you stay nourished without causing further irritation.
Foods to Eat
Focus on soft, cool, and non-acidic foods that are easy to swallow:
- Smoothies and protein shakes
- Unsweetened yogurt and kefir
- Scrambled eggs
- Mashed potatoes, sweet potatoes, or squash
- Lukewarm soups and broths
- Oatmeal and other soft-cooked cereals
Foods to Avoid
Steer clear of anything that could scrape or burn your sensitive mouth tissues:
- Hard or crunchy foods: Chips, nuts, crusty bread, raw vegetables.
- Spicy foods: Anything with chili, hot sauce or strong spices.
- Highly acidic foods: Citrus fruits (oranges, lemons), tomatoes and vinegar-based dressings.
- Sugary foods and drinks: Soda, candy and pastries can feed the yeast and may worsen the infection.
When to Seek Professional Help
While mild thrush can sometimes be managed with simple measures, it’s a condition that warrants professional attention, especially in adults.
Knowing when to see a doctor can prevent complications and help identify potentially serious underlying health issues.
When Should I See a Doctor or Specialist for Thrush?
Use this list of “red flags” as a guide for when to schedule an appointment without delay.
You should see a doctor if:
- This is your first time suspecting thrush. An episode of thrush in a healthy adult can be the first sign of an undiagnosed condition like diabetes or an immune issue. A proper diagnosis is essential.
- Symptoms are severe, widespread, or you have difficulty swallowing. This could indicate the infection is spreading to your esophagus, which requires immediate and more aggressive treatment.
- The infection does not improve after a week of treatment. If over-the-counter measures or even prescribed medication isn’t working, you may have a resistant strain of Candida or an incorrect diagnosis.
- The infection recurs frequently. If you experience three or more thrush infections in a year, this is considered recurrent and points to an unresolved underlying cause that needs investigation.
- You develop a fever, chills, or feel generally unwell along with the oral symptoms. This could be a sign that the infection is becoming systemic, a rare but serious complication.
Which Professional Should You See?
- Primary Care Physician (PCP): Your family doctor is the best starting point for an initial diagnosis, prescription for medication, and ordering tests for underlying conditions like diabetes.
- Dentist: A dentist is an excellent resource, especially if you wear dentures or if the diagnosis is uncertain. They are experts in oral pathology and can provide guidance on oral hygiene and denture care.
- Infectious Disease Specialist: For complex, treatment-resistant, or recurrent cases, particularly in immunocompromised patients, a referral to an infectious disease specialist may be necessary. They have expertise in managing difficult fungal infections.
Frequently Asked Questions (FAQ)
Here are concise answers to some of the most common questions about oral thrush in adults.
1. How long does it take for thrush treatment to work?
With appropriate antifungal medication, symptoms usually begin to improve within a few days. A full course of treatment typically lasts 7 to 14 days to ensure the infection is completely cleared and prevent immediate recurrence.
2. Can I get rid of thrush without medication?
It is highly unlikely for a significant thrush infection in an adult to resolve without antifungal medication. Home remedies can help soothe symptoms, but they do not cure the infection. Medical treatment is necessary to eliminate the fungal overgrowth.
3. Is oral thrush a sign of HIV?
While oral thrush is a very common opportunistic infection in people with untreated HIV, it is not exclusively a sign of it. Many other conditions, like diabetes, steroid use, or taking antibiotics, are far more common causes in the general population.
4. Does using mouthwash help or hurt thrush?
Most commercial, alcohol-based mouthwashes can hurt more than help. They can disrupt the natural oral microbiome and cause burning and irritation. A simple saltwater or baking soda rinse is a much safer and more soothing option during an outbreak.
5. Can stress cause oral thrush?
While not a direct cause, chronic stress can weaken the immune system. A suppressed immune system is less effective at keeping Candida in check, so high levels of stress could be a contributing factor to an outbreak in susceptible individuals.
6. Why do I keep getting thrush?
Recurrent thrush is almost always a sign of an unaddressed underlying cause. This could be uncontrolled blood sugar, a medication you’re taking, an ill-fitting denture, or an undiagnosed immune system issue. Work with your doctor to investigate the root cause.
7. Should I throw away my toothbrush after having thrush?
Yes, it is a good practice to replace your toothbrush once the infection has cleared. This helps prevent reintroducing a high concentration of the fungus back into your mouth and reduces the risk of a new infection starting.
8. Can I pass thrush to my partner through kissing?
For healthy individuals, this is extremely unlikely, as their immune systems can easily control the fungus. However, if your partner is also immunocompromised or has other risk factors, transmission is theoretically possible, though still not common.
9. What’s the difference between thrush and a white tongue from dehydration?
A white coating from dehydration is usually a thin, uniform film on the tongue’s surface that resolves with hydration. Thrush typically presents as distinct, raised, clumpy patches (like cottage cheese) that, when scraped, reveal a red, sore base.
Conclusion
Navigating an oral thrush infection can be uncomfortable and concerning, but it is a manageable and treatable condition.
The key to success lies in understanding that adult thrush is rarely a standalone issue, it is a sign of an internal imbalance.
Effective management, therefore, requires a two-pronged approach: using the correct antifungal medication to clear the current infection and, just as importantly, working with a healthcare professional to identify and address the underlying cause.
By taking control of contributing factors—be it managing blood sugar, adjusting medications, or optimizing oral and denture hygiene—you can move from simply treating outbreaks to preventing them altogether.
This guide has equipped you with the knowledge to recognize symptoms, understand your treatment options and implement long-term preventive strategies.
If you are experiencing the symptoms discussed in this guide, schedule an appointment with your healthcare provider. An accurate diagnosis is the first step toward fast relief and preventing future infections.
Have you successfully treated recurrent thrush? Share your experience or ask a question in the comments below to help our community.
Reference
[1] What is the best treatment for oral candidiasis (thrush)?
https://www.droracle.ai/articles/68832/best-treatment-for-thrush-
[2] Treatment of Candidiasis
https://www.cdc.gov/candidiasis/treatment/index.html
[3] https://www.mayoclinic.org/diseases-conditions/oral-thrush/symptoms-causes/syc-20353533
[4] Oral Candidiasis – StatPearls
https://www.ncbi.nlm.nih.gov/books/NBK545282
[5] https://my.clevelandclinic.org/health/diseases/10956-thrush
[6] 9 Home Remedies for Oral Thrush
https://www.healthline.com/health/home-remedies-for-thrush
[7] What Medications Treat Oral Thrush?
[8] Therapeutic tools for oral candidiasis: Current and new …

