An adult ear infection is typically treated by managing pain with over-the-counter medications and, if the infection is bacterial and severe, with prescription antibiotics.
While often associated with childhood, millions of adults experience the debilitating pain of an ear infection each year.
In fact, globally, there were over 391 million cases of otitis media in 2021, affecting all age groups.
Unlike in children, an adult ear infection can sometimes signal an underlying health issue, making proper diagnosis and treatment crucial.
This guide will walk you through everything you need to know, from identifying the type of infection to understanding effective treatments and preventive measures, empowering you to manage your health with confidence.
Keep reading to learn how to find relief and protect your hearing.
In This Article
What Exactly Is an Ear Infection in Adults?
An ear infection, medically known as otitis, is an inflammation of the ear, usually caused by bacteria or viruses.
The inflammation leads to fluid buildup and pressure, causing the characteristic pain.
While the term “ear infection” is used broadly, it’s crucial to understand that there are three main types, distinguished by which part of the ear is affected.
Each type has different causes, symptoms, and requires a distinct treatment approach.
- Outer Ear Infection (Otitis Externa): This affects the outer ear canal, the tube running from your ear opening to your eardrum. It’s often called “swimmer’s ear” because it’s commonly caused by water that remains in the ear after swimming, creating a moist environment for bacteria to grow.
- Middle Ear Infection (Otitis Media): This is an infection of the air-filled space behind the eardrum, which contains the tiny vibrating bones of the ear. This is the most common type of ear infection and often follows a cold, flu, or allergy that causes congestion and swelling of the nasal passages and throat.
- Inner Ear Infection (Labyrinthitis): This is an inflammation of the inner ear, which affects the parts of the ear responsible for balance and hearing. This type is less common and is almost always caused by a virus. It can cause severe dizziness (vertigo) and hearing loss.
Understanding which part of your ear is affected is the first step toward getting the right diagnosis and effective ear infection treatment.
Why Do Adults Get Ear Infections?
While ear infections are far more common in children, adults are not immune.
The reasons an adult develops an ear infection are often linked to anatomical differences and lifestyle or health factors that are less prevalent in childhood.
A primary culprit is the dysfunction of a small but critical structure: the Eustachian tube.
The Role of Eustachian Tube Dysfunction in Adults
The Eustachian tube is a narrow canal connecting the middle ear to the back of the throat.
Its job is to regulate air pressure and drain fluid from the middle ear.
In adults, these tubes are longer and more steeply angled than in children, which generally allows for better drainage.
However, when these tubes become blocked or swollen due to illness or allergies, they can’t do their job.
Fluid gets trapped in the middle ear, creating a perfect breeding ground for viruses and bacteria that have traveled up from the throat.
This is the primary mechanism behind a middle ear infection in adults.
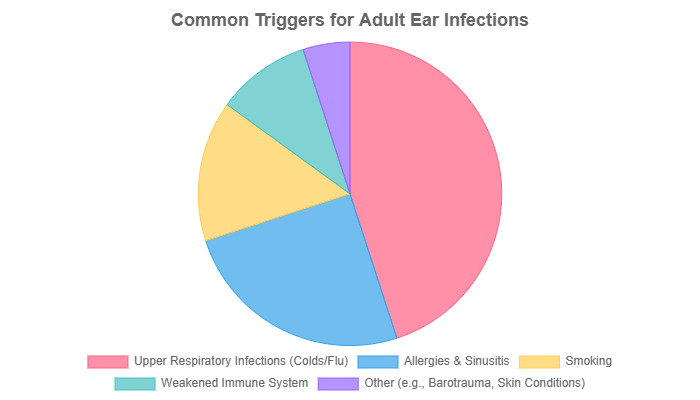
Common Triggers and Risk Factors
Several factors can increase an adult’s risk of developing an ear infection:
- Upper Respiratory Infections: The common cold and flu are the most frequent precursors to a middle ear infection. The inflammation and mucus production can easily block the Eustachian tubes.
- Allergies: Seasonal allergies or chronic sinus issues cause persistent inflammation that can lead to Eustachian tube dysfunction.
- Smoking and Secondhand Smoke: Tobacco smoke irritates the lining of the respiratory system, including the Eustachian tubes, impairing their function and increasing infection risk.
- Weakened Immune System: Chronic illnesses (like diabetes) or immunosuppressant medications can make adults more susceptible to all types of infections, including in the ear.
- Changes in Altitude: Flying or scuba diving can cause sudden pressure changes that strain the Eustachian tubes, a condition known as barotrauma, which can lead to fluid buildup.
- Skin Conditions: Eczema or psoriasis in or around the ear canal can compromise the skin’s protective barrier, making an outer ear infection more likely.
What Are the Telltale Symptoms of an Adult Ear Infection?
Recognizing the ear infection symptoms is the first step toward seeking appropriate care.
The experience can range from a mild annoyance to excruciating pain, and the specific symptoms often point to the type of infection you have.
Middle Ear Infection (Otitis Media) Symptoms
A middle ear infection often develops rapidly.
As described by many adults on forums like Reddit, the pain can be intense and radiating.
- Deep Ear Pain: A sharp, stabbing, or dull, throbbing ache deep inside the ear. Many adults report the pain worsens when lying down and may radiate to the jaw or neck.
- Feeling of Fullness or Pressure: A sensation that the ear is clogged or underwater, which is caused by fluid buildup behind the eardrum.
- Muffled Hearing: Sound may seem distant or muffled in the affected ear.
- Fluid Drainage: If the pressure becomes too great, the eardrum can rupture, leading to a sudden drainage of yellow, brown, or bloody fluid. Paradoxically, this often brings immediate pain relief.
- Fever: A low-grade fever may accompany the infection.
Outer Ear Infection (Otitis Externa) Symptoms
An outer ear infection, or swimmer’s ear, presents with symptoms localized to the ear canal.
- Itching and Redness: The infection often starts with itching in the ear canal, which progresses to redness and swelling.
- Pain on Touch: A key sign is severe pain when the outer ear (pinna) is pulled or when the small cartilage flap (tragus) in front of the ear opening is pushed.
- Clear, Watery Drainage: Initially, the drainage is usually clear, but it can become pus-like as the infection progresses.
- Feeling of Blockage: Swelling and debris can make the ear feel blocked, affecting hearing.
Less Common: Inner Ear Infection (Labyrinthitis) Symptoms
An inner ear infection is a more serious condition that affects your sense of balance and hearing.
- Vertigo: A sudden and severe sensation that you or your surroundings are spinning. This can cause nausea and vomiting.
- Hearing Loss: Sudden hearing loss in the affected ear.
- Tinnitus: A ringing or buzzing sound in the ear.
- Loss of Balance: Difficulty walking straight or feeling unsteady on your feet.
How Can I Tell the Difference Between a Middle and Outer Ear Infection?
Distinguishing between a middle and outer ear infection is key because their treatments differ.
While a doctor’s diagnosis is essential, this table can help you identify the likely culprit based on your symptoms.
This is a common area of confusion and a critical step in understanding your condition.
| Feature | Middle Ear Infection (Otitis Media) | Outer Ear Infection (Otitis Externa) |
|---|---|---|
| Primary Location of Pain | Deep, internal ache inside the ear. | Pain in the ear canal, sensitive to touch on the outer ear. |
| Key Differentiator | Pain is internal and often follows a cold/flu. Hearing is muffled. | Pain is triggered by pulling the earlobe or pressing the tragus. |
| Common Causes | Bacteria or viruses from a respiratory infection. | Bacteria (or sometimes fungi) from trapped moisture. |
| Fluid Drainage | Pus-like or bloody fluid, but only if the eardrum ruptures. | Often starts as clear, watery fluid, may become pus-like. |
| Hearing | Muffled, as if underwater, due to fluid behind the eardrum. | Blocked or reduced due to swelling and debris in the ear canal. |
| Typical Treatment | Often observation, oral antibiotics if bacterial and severe. | Antibiotic or antifungal ear drops are the primary treatment. |
When Should I See a Doctor for an Ear Infection?
While some mild ear infections may resolve on their own, it’s important not to underestimate them, especially in adults.
According to leading health institutions like the Mayo Clinic, an ear infection in an adult can sometimes indicate a more serious underlying problem.
You should seek medical attention if you experience any of the following:
- Severe Pain: Pain that is intense, unbearable, or doesn’t improve with over-the-counter pain relievers.
- Symptoms Lasting More Than 2-3 Days: If your symptoms persist or worsen after 48-72 hours, it’s time to see a doctor.
- High Fever: A fever above 102.2°F (39°C) is a sign of a significant infection that needs medical evaluation.
- Fluid, Pus or Blood Drainage: Any drainage from the ear canal warrants a visit to the doctor to check for a ruptured eardrum or severe outer ear infection.
- Sudden Hearing Loss or Changes: Any noticeable decrease in your ability to hear needs immediate attention.
- Symptoms of an Inner Ear Infection: Dizziness, vertigo, loss of balance, or ringing in the ears (tinnitus) are red flags for a more serious condition.
- Underlying Health Conditions: If you have diabetes, a compromised immune system, or other chronic health issues, you should see a doctor at the first sign of an ear infection.
How Are Adult Ear Infections Diagnosed?
A proper diagnosis is essential for effective ear infection treatment.
Your doctor will typically start with a thorough history of your symptoms and a physical examination.
The Physical Exam: What to Expect
Your doctor will use a special instrument called an otoscope, which has a light and a magnifying lens, to look inside your ear. This allows them to visualize the ear canal and the eardrum.
- For an Outer Ear Infection: The doctor will see a red, swollen ear canal, possibly with debris or pus.
- For a Middle Ear Infection: The doctor will look at the eardrum. A healthy eardrum is pinkish-gray and translucent. Signs of infection include a red, bulging eardrum, which indicates fluid and pressure behind it. They may also see fluid or air bubbles behind the eardrum.
A pneumatic otoscope, which puffs a small amount of air against the eardrum, is often used.
A healthy eardrum will move back and forth, but an eardrum with fluid behind it will barely move, confirming a middle ear infection.
Advanced Diagnostic Tools
If the diagnosis is unclear, the infection is chronic, or there are complications, your doctor might recommend further tests:
- Tympanometry: This test measures the movement of the eardrum and the pressure in the middle ear, providing a more objective measure of fluid buildup.
- Acoustic Reflectometry: This uses sound waves to determine if there is fluid in the middle ear.
- Tympanocentesis: In rare, severe, or recurrent cases, a specialist may use a needle to draw fluid from the middle ear. This fluid can then be tested to identify the specific bacteria causing the infection, which helps in choosing the most effective antibiotic.
What Are the Most Effective Ear Infection Treatments for Adults?
The treatment for an adult ear infection depends heavily on the type and severity.
The goal is to clear the infection, relieve pain and prevent complications.
Modern treatment guidelines often favor a conservative approach to avoid the overuse of antibiotics.
The “Watchful Waiting” Approach
Many middle ear infections are caused by viruses, which do not respond to antibiotics.
Even bacterial infections can often be cleared by the body’s immune system.
For this reason, especially for mild to moderate cases, doctors may recommend a “wait-and-see” approach for 48 to 72 hours.
This strategy, supported by organizations like the Cleveland Clinic, helps reduce antibiotic resistance.
During this period, the focus is on managing pain. If symptoms don’t improve or worsen, then prescription medication is considered.
Over-the-Counter (OTC) Pain Management
Pain is often the most distressing symptom. The following can provide significant relief:
- Pain Relievers: Ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) are effective at reducing pain and fever.
- Warm Compress: Applying a warm, moist cloth to the affected ear can help soothe the ache. Be careful not to use excessive heat.
- Anesthetic Ear Drops: Over-the-counter ear drops containing ingredients like benzocaine can temporarily numb the ear canal, but they should not be used if the eardrum has ruptured.
Prescription Medications: Antibiotics and Ear Drops
If the infection is determined to be bacterial and severe, or if it doesn’t improve, your doctor will prescribe medication.
- Oral Antibiotics: For a moderate to severe middle ear infection, a course of oral antibiotics is the standard treatment. High-dose amoxicillin is typically the first-line choice, as confirmed by recent research into its continued effectiveness. It’s crucial to complete the full course of antibiotics, even if you start feeling better, to ensure the infection is completely eradicated.
- Antibiotic Ear Drops: For an outer ear infection (swimmer’s ear), the primary treatment is prescription ear drops. These drops often contain a combination of an antibiotic to kill bacteria and a steroid to reduce inflammation and swelling. This localized treatment is highly effective and avoids the systemic side effects of oral antibiotics.
Are Home Remedies Safe and Effective?
Many people search for natural treatments.
While some can offer comfort, others are ineffective or even dangerous.
It’s vital to approach them with caution.
- Generally Safe for Comfort: A warm compress is a safe way to ease pain. Staying hydrated and resting helps your immune system fight the infection.
- Use with Caution: Some sources suggest garlic oil or tea tree oil drops. While these have some antimicrobial properties, their effectiveness in the ear is not well-supported by robust scientific evidence. Putting any oil in the ear can be risky, especially if the eardrum is perforated.
- Avoid: Never stick cotton swabs or any other objects into your ear canal. This can push blockages further in, damage the eardrum, and worsen an outer ear infection. Hydrogen peroxide can also be overly irritating to the delicate skin of the ear canal.
Always consult your doctor before trying any home remedy for an ear infection.
What Happens if an Ear Infection Is Left Untreated?
While most adult ear infections resolve without issue, ignoring a persistent or severe infection can lead to serious and sometimes permanent complications.
This is why seeking timely medical advice is so important.
Hearing Loss and Balance Issues
The most common complication is temporary hearing loss.
The fluid buildup in a middle ear infection (known as otitis media with effusion) can persist for weeks or even months after the infection clears, causing muffled hearing.
In most cases, hearing returns to normal once the fluid drains. However, recurrent or chronic infections can cause lasting damage.
Chronic inflammation can damage the delicate structures of the middle and inner ear, including the eardrum and the ossicles (hearing bones), potentially leading to permanent hearing loss.
If the inner ear is affected, long-term balance problems and dizziness can also occur.
Chronic Infections and Structural Damage
An infection that doesn’t heal or keeps coming back is considered chronic.
This can lead to several structural problems:
- Perforated Eardrum: While most eardrum ruptures from an acute infection heal on their own, chronic infections can create a persistent hole that may require surgical repair (a tympanoplasty).
- Cholesteatoma: This is a noncancerous skin growth that can develop in the middle ear behind the eardrum, often as a result of repeated infections. It can grow and destroy the surrounding bone structures, leading to hearing loss and other serious issues.
Rare but Serious Complications
In very rare instances, the infection can spread from the ear to other parts of the head.
These complications are medical emergencies.
- Mastoiditis: The infection can spread to the mastoid bone, the bony protrusion behind the ear. This causes redness, swelling, and pain behind the ear and requires immediate treatment with intravenous antibiotics. A 2023 study published in StatPearls highlights that while antibiotics are key, they are not always sufficient alone, sometimes requiring surgical drainage. (Source: StatPearls – Mastoiditis)
- Meningitis: If the infection spreads to the protective membranes surrounding the brain and spinal cord, it can cause bacterial meningitis, a life-threatening condition.
How Can I Prevent Future Ear Infections?
Taking proactive steps can significantly reduce your risk of developing another painful ear infection.
- Manage Colds and Allergies: Since upper respiratory issues are a primary trigger, managing them is key. Wash your hands frequently, avoid sick individuals, and work with your doctor to control seasonal allergies with antihistamines or nasal steroids.
- Keep Ears Dry: For preventing outer ear infections, thoroughly dry your ears after swimming or showering. Tilt your head to each side to let water drain. A hairdryer on a low, cool setting held at a distance can also help.
- Don’t Smoke: Quitting smoking is one of the best things you can do for your overall and ear health. Avoid exposure to secondhand smoke as well.
- Avoid Inserting Objects in Your Ears: Do not use cotton swabs, bobby pins, or other objects to clean your ears. They can cause trauma to the ear canal and push wax deeper, creating a blockage.
- Get Vaccinated: Staying up-to-date on vaccinations, such as the annual flu shot and the pneumococcal vaccine, can help prevent the illnesses that often lead to ear infections.
- Manage Underlying Conditions: If you have a chronic condition like diabetes or an autoimmune disorder, keeping it well-managed will help your body’s ability to fight off infections.
Conclusion
An ear infection in adults is more than just a painful nuisance, it’s a health signal that deserves attention.
By understanding the different types of infections, recognizing their specific symptoms and knowing when to seek medical help, you can ensure a swift and effective recovery.
From managing pain with simple home care to completing a full course of prescribed antibiotics, proper ear infection treatment is vital to prevent discomfort from escalating into serious complications like hearing loss.
Remember to prioritize prevention by managing allergies, keeping your ears dry, and maintaining a healthy lifestyle.
If you are experiencing severe pain, a high fever, or any symptoms that concern you, do not hesitate to consult a healthcare professional.
Taking proactive control of your ear health is the best way to protect your hearing and well-being for years to come.
Frequently Asked Questions (FAQ)
1. How long does an adult ear infection last?
A mild ear infection may improve within 2-3 days and resolve completely in 1-2 weeks. More severe bacterial infections treated with antibiotics should show significant improvement within 48-72 hours of starting medication. Fluid in the middle ear can persist for several weeks.
2. Can an ear infection go away on its own?
Yes, many viral and some mild bacterial ear infections can resolve without antibiotics as the body’s immune system fights them off. However, if symptoms are severe or persist beyond 2-3 days, medical evaluation is necessary to prevent complications.
3. Is an adult ear infection contagious?
The ear infection itself is not contagious. However, the underlying viruses or bacteria causing the cold or flu that led to the ear infection are contagious. You can’t “catch” an ear infection from someone, but you can catch the cold that might cause one.
4. Why is my ear infection pain worse at night?
When you lie down, the pressure in your middle ear can change, and fluid drainage from the Eustachian tubes becomes less efficient. This can increase pressure on the eardrum, leading to more intense pain compared to when you are upright.
5. Can I fly with an ear infection?
Flying with an active middle ear infection is generally not recommended. The changes in air pressure during takeoff and landing can cause severe pain, dizziness, and even eardrum rupture because the blocked Eustachian tube cannot equalize pressure properly.
6. What’s the difference between an ear infection and earwax blockage?
An ear infection causes sharp or dull pain, often with fever and fluid. An earwax blockage typically causes a feeling of fullness, muffled hearing and sometimes tinnitus or dizziness, but usually without the acute pain and signs of infection.
7. Do I need antibiotics for every ear infection?
No. Antibiotics are only effective for bacterial infections. Since many ear infections are viral, and some bacterial ones resolve on their own, doctors often recommend a “watchful waiting” period. Over-prescription of antibiotics contributes to antibiotic resistance.
8. What is the fastest way to get rid of an ear infection?
The fastest way is to get a proper diagnosis. For a bacterial infection, starting the correct antibiotic is key. For all types, managing pain with OTC relievers and a warm compress provides the quickest relief from the most severe symptoms.

