A diabetic diet is a healthy-eating plan focused on nutrient-dense whole foods, moderate portions and regular mealtimes to help you control blood sugar and feel your best.
It’s not about deprivation, but about empowerment—making conscious choices that nourish your body and support your long-term health.
With over 38.4 million Americans living with diabetes, a number that continues to grow, understanding the profound impact of diet is more critical than ever.
According to the Centers for Disease Control and Prevention (CDC), managing what you eat is a cornerstone of diabetes care, capable of transforming your health trajectory.
This guide is designed to be your definitive resource. We will move beyond simple lists to explain the *why* behind each food choice.
You will gain comprehensive “eat this” and “avoid that” lists, a clear explanation of how food affects your blood sugar, a simple 7-day meal plan to get you started, and practical, real-world tips to make this transition seamless and sustainable.
Let’s dive into the foods that will form the foundation of your new, healthier lifestyle.
In This Article
What Is a Diabetic Diet and Why Is It So Important?
The term “diabetic diet” can be misleading. It suggests a single, rigid set of rules, but the reality is far more personalized and flexible.
It’s less of a “diet” in the restrictive sense and more of a structured, evidence-based eating pattern tailored to your individual needs.
The American Diabetes Association (ADA), in its 2024 Standards of Care, emphasizes that there is no single ideal dietary pattern for all people with diabetes. Instead, it advocates for Medical Nutrition Therapy (MNT), a personalized approach developed with a registered dietitian or healthcare provider.
This approach focuses on nutrient-dense eating patterns that are proven to help manage diabetes.
The core goal is simple yet profound: to maintain your blood glucose (sugar) levels within a target range, preventing the dangerous highs and lows that characterize unmanaged diabetes.
The Core Goal: Blood Sugar Control
When you eat, your body breaks down carbohydrates from foods like bread, rice, fruits and vegetables into glucose. This glucose enters your bloodstream, providing energy to your cells.
The hormone insulin acts like a key, allowing this glucose to move from your blood into your cells. In people with diabetes, this process is impaired.
- Hyperglycemia (High Blood Sugar): Occurs when there’s not enough insulin, or the body can’t use it effectively, causing glucose to build up in the blood. A well-structured diabetic diet limits foods that cause rapid glucose spikes.
- Hypoglycemia (Low Blood Sugar): Can occur if you take certain diabetes medications (like insulin) and don’t eat enough, or if you eat at inconsistent times. A diabetic diet emphasizes regular, balanced meals to prevent these drops.
By carefully selecting the types and amounts of carbohydrates and balancing them with protein and healthy fats, you can slow down glucose absorption and provide your body with a steady supply of energy, preventing these harmful fluctuations.
Beyond Blood Sugar: The Systemic Benefits
The importance of a diabetic diet extends far beyond immediate glucose readings. It is a powerful tool for preventing the serious long-term complications associated with the disease.
As the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) highlights, uncontrolled diabetes can damage your heart, blood vessels, kidneys, nerves and eyes.
A well-managed diabetic diet directly addresses these risks by helping you:
- Manage Weight: The focus on whole foods and portion control naturally supports achieving and maintaining a healthy weight, which can dramatically improve insulin sensitivity.
- Control Blood Pressure and Cholesterol: By limiting sodium, unhealthy fats, and processed foods, the diet helps manage hypertension and high cholesterol—two major risk factors for heart disease and stroke, which are significantly elevated in people with diabetes.
- Reduce Long-Term Complication Risk: Consistent blood sugar control is the single most effective strategy for protecting your vital organs. Every healthy meal is an investment in your future, reducing the likelihood of developing neuropathy (nerve damage), nephropathy (kidney disease) and retinopathy (eye damage).
In essence, a diabetic diet is not a punishment, it is your primary strategy for taking control, feeling better, and living a longer, healthier life with diabetes.
What Foods Can I Eat on a Diabetic Diet?
Navigating the grocery store can feel overwhelming when you’re newly diagnosed. The key is to focus on whole, unprocessed foods.
This section provides your “Green Light” list—foods you can confidently build your meals around.
Think of these as the building blocks of your healthy eating plan.
Non-Starchy Vegetables: The Foundation of Your Plate
Why they’re great: These are your nutritional superstars. They are incredibly low in carbohydrates and calories but packed with fiber, vitamins and minerals. Fiber is crucial as it slows digestion, preventing rapid blood sugar spikes, and helps you feel full and satisfied.
Serving Ideas: Aim to fill half your plate with these at every meal. Roast them with olive oil, steam them, add them to stir-fries, or eat them raw in salads.
- Artichoke
- Asparagus
- Beets
- Bell Peppers (all colors)
- Broccoli
- Brussels Sprouts
- Cabbage
- Carrots
- Cauliflower
- Celery
- Cucumbers
- Eggplant
- Green Beans
- Jicama
- Leafy Greens (Spinach, Kale, Arugula, Romaine)
- Mushrooms
- Onions
- Radishes
- Spaghetti Squash
- Tomatoes
- Zucchini
Lean Proteins: For Muscle Health and Satiety
Why they’re great: Protein has a minimal effect on blood sugar levels and is essential for building and repairing tissues. Including a source of lean protein with your meals promotes satiety, helping to prevent overeating and keeping you full between meals.
Serving Ideas: Aim for a portion about the size of your palm (a quarter of your plate). Choose baked, grilled, roasted or broiled methods over frying.
- Poultry: Skinless chicken or turkey breast
- Fish: Especially fatty fish rich in omega-3s like salmon, mackerel, herring, sardines, and tuna. Other good choices include cod, tilapia and haddock.
- Eggs: A versatile and affordable option.
- Plant-Based: Tofu, tempeh and edamame.
- Dairy: Plain Greek yogurt and cottage cheese.
Heart-Healthy Fats: Your Allies Against Complications
Why they’re great: Gone are the days of fearing all fats. Monounsaturated and polyunsaturated fats are vital for health. They help lower LDL (“bad”) cholesterol, reduce inflammation, and protect your heart—a critical benefit, as diabetes increases cardiovascular risk. Fats also aid in the absorption of certain vitamins and contribute to feeling full.
Serving Ideas: Use these in moderation, as they are calorie-dense. Add a quarter of an avocado to your salad, snack on a small handful of nuts or use olive oil for cooking and dressings.
- Oils: Extra virgin olive oil, avocado oil, canola oil
- Nuts: Almonds, walnuts, pecans, pistachios (unsalted)
- Seeds: Chia seeds, flaxseeds, pumpkin seeds, sunflower seeds
- Avocado: A creamy source of monounsaturated fat and fiber.
- Nut Butters: Natural peanut, almond or cashew butter (check for no added sugar).
Complex Carbohydrates & Whole Grains: The Right Kind of Energy
Why they’re great: Unlike refined carbs, complex carbohydrates are digested slowly because they contain all parts of the grain—the bran, germ and endosperm. This means they are rich in fiber, B vitamins and minerals. The fiber content is key, as it leads to a more gradual rise in blood sugar.
Serving Ideas: Limit portions to about one cup cooked, or a quarter of your plate. Swap white rice for quinoa and white bread for 100% whole-wheat bread.
- Quinoa
- Brown Rice
- Oats (Rolled or Steel-Cut)
- Barley
- Farro
- Bulgur
- 100% Whole-Wheat Bread, Pasta, and Crackers
- Wild Rice
Fruits: Nature’s Candy in Moderation
Why they’re great: Fruits provide essential vitamins, antioxidants and fiber. While they do contain natural sugar (fructose), their fiber content helps buffer its impact on blood sugar compared to processed sweets. Always choose whole fruits over juice, which has been stripped of its beneficial fiber.
Serving Ideas: A small piece of whole fruit or about one cup of berries is a typical serving. Pair fruit with a protein or fat source, like an apple with a handful of almonds, to further slow glucose absorption.
- Berries: Strawberries, blueberries, raspberries, blackberries (highest in fiber, lowest in sugar)
- Apples and Pears: Leave the skin on for extra fiber.
- Citrus Fruits: Oranges, grapefruit, clementines
- Stone Fruits: Peaches, plums, apricots, cherries
- Melon: Cantaloupe, honeydew (in moderation)
Legumes: The Fiber and Protein Powerhouses
Why they’re great: Legumes are a unique food group, offering a powerful combination of high-quality plant-based protein and fiber-rich complex carbohydrates. This duo makes them incredibly effective at promoting stable blood sugar and long-lasting fullness.
Serving Ideas: Add them to soups, salads, and stews, or use them as a primary protein source in vegetarian meals. A serving is typically about ½ to 1 cup cooked.
- Lentils (brown, green, red)
- Chickpeas (Garbanzo Beans)
- Black Beans
- Kidney Beans
- Pinto Beans
- Navy Beans
Dairy and Dairy Alternatives: Calcium and Protein Sources
Why they’re great: Dairy products provide calcium for bone health, as well as protein. The key is to choose options that are low in fat and free from added sugars.
Serving Ideas: Opt for plain Greek yogurt and add your own berries for sweetness. Use low-fat milk in your coffee or with whole-grain cereal.
- Plain, non-fat or low-fat Greek Yogurt
- Low-fat (1%) or skim milk
- Low-fat Cottage Cheese
- Unsweetened fortified milk alternatives (almond, soy, oat)
What Foods Should I Avoid or Limit with Diabetes?
Just as important as knowing what to eat is understanding which foods can sabotage your blood sugar control and increase your risk for complications.
This isn’t about making foods “forbidden” forever, but about recognizing their impact and significantly limiting their place in your regular diabetic diet.
The focus is on reduction and replacement with healthier alternatives.
Sugary Beverages: The #1 Enemy of Blood Sugar Control
Why they’re bad: This is the single most important category to eliminate. Liquid sugar is absorbed almost instantly into your bloodstream, causing a dramatic and rapid spike in blood glucose. These drinks offer zero nutritional value—only empty calories and a metabolic challenge your body doesn’t need.
What to avoid:
- Regular Soda
- Fruit Juice (even 100% juice)
- Sweetened Iced Tea and Lemonade
- Sports and Energy Drinks
- Sweetened Coffee and Tea Drinks (lattes, frappuccinos)
What to choose instead: Water, sparkling water, unsweetened tea and black coffee.
Refined Grains and Processed Carbs
Why they’re bad: These foods have been stripped of their fiber and nutrients during processing. Without fiber to slow them down, your body digests them almost as quickly as pure sugar, leading to sharp blood sugar increases. A review in the Journal of Education and Health Promotion confirms that dietary patterns high in refined grains are associated with an increased risk of Type 2 Diabetes.
What to limit or avoid:
- White Bread, Bagels and Rolls
- White Rice
- Most Packaged Cereals (especially frosted or “puffed” varieties)
- Crackers, Pretzels, and Rice Cakes
- Pastries, Doughnuts, Croissants and Muffins
What to choose instead: 100% whole-grain versions of bread and pasta, brown rice, quinoa and oats.
Saturated and Trans Fats
Why they’re bad: While healthy fats are your friends, saturated and trans fats are not. They raise LDL (“bad”) cholesterol levels, contributing to the buildup of plaque in your arteries (atherosclerosis). This significantly increases the risk of heart attack and stroke, a danger that is already heightened for individuals with diabetes, as noted by the Mayo Clinic.
What to limit or avoid:
- Trans Fats: Found in stick margarine, shortening, some packaged baked goods, and many fried fast foods. Avoid any product with “partially hydrogenated oil” in the ingredients list.
- Saturated Fats: Fatty cuts of red meat (ribeye, T-bone), processed meats, poultry with skin, full-fat dairy products (butter, cream, cheese, whole milk), and tropical oils like coconut and palm oil.
What to choose instead: Lean proteins, low-fat dairy and plant-based fats like olive oil and avocado.
Processed Meats and High-Sodium Foods
Why they’re bad: Processed meats are often high in both saturated fat and sodium. High sodium intake is a primary driver of high blood pressure (hypertension), another major risk factor for heart disease. Many other processed and packaged foods are loaded with sodium as a preservative and flavor enhancer.
What to limit or avoid:
- Bacon and Sausage
- Hot Dogs and Bratwurst
- Deli Meats (salami, bologna)
- Canned Soups and Vegetables (unless labeled “low sodium”)
- Frozen Dinners and Packaged Meal Kits
- Salty Snacks (chips, salted nuts)
What to choose instead: Freshly cooked lean meats, low-sodium canned goods, and flavoring food with herbs and spices instead of salt.
Hidden Sugars in “Healthy” Foods
Why they’re bad: This is where label-reading becomes a crucial skill. Many foods marketed as “healthy” or “natural” are loaded with added sugars that can derail your blood sugar management. Food manufacturers use dozens of different names for sugar, making it easy to overlook.
What to watch out for:
- Flavored Yogurts: A single serving can have as much sugar as a candy bar.
- Granola and Granola Bars: Often held together with syrups and sugars.
- Salad Dressings: Especially “light” or “fat-free” versions often compensate with extra sugar.
- Condiments: Ketchup, barbecue sauce and teriyaki sauce are major sources of hidden sugar.
- Pasta Sauces: Many jarred sauces contain significant amounts of added sugar to balance acidity.
What to choose instead: Plain yogurt (add your own fruit), homemade granola, oil-and-vinegar based dressings and sauces with no added sugar on the label.
How Do I Create a Diabetic Diet Plan That Works for Me?
Knowing which foods to eat and avoid is the first step. The next is learning how to combine them into balanced, satisfying meals. There are several effective strategies for building a personal diabetic diet plan.
The best method is the one you can stick with consistently. Here, we explore the most common and effective approaches.
The Plate Method: Your Simple Visual Guide
Endorsed by both the NIDDK and the ADA, the Plate Method is the easiest way to start building healthy meals without any counting or measuring. It’s a simple, visual way to ensure proper portion control and nutrient balance.
How it works:
- Start with a 9-inch plate. Using a smaller plate than a typical large dinner plate can help manage portions automatically.
- Fill half your plate with non-starchy vegetables. This is the foundation. Load up on spinach, broccoli, salad greens, green beans or bell peppers. This ensures you get plenty of fiber and nutrients with minimal carbs.
- Fill one quarter of your plate with lean protein. This could be a piece of grilled chicken, a salmon fillet, or a serving of tofu.
- Fill the final quarter with complex carbohydrates. This is your energy source. Choose foods like quinoa, brown rice, a small sweet potato or whole-wheat pasta.
You can complete your meal with a glass of water or unsweetened tea and, if your plan allows, a serving of fruit or low-fat dairy.
Introduction to Carbohydrate Counting
Carbohydrate counting, or “carb counting,” is a more advanced meal planning method that is particularly useful for people who take mealtime insulin.
It involves tracking the number of grams of carbohydrates you eat and drink to match your insulin dose to your food intake more precisely.
The basic concept:
- Carbohydrates are the main nutrient that affects blood glucose levels.
- Foods are measured in “servings” of carbohydrates. One serving is typically equal to 15 grams of carbs.
- Your healthcare provider or a registered dietitian will help you determine a target number of carb servings for each meal and snack.
For example, a meal target might be 3-4 carb servings (45-60 grams). You would then choose foods to meet that target, such as 1 cup of whole-wheat pasta (3 servings) and a side of non-starchy vegetables (negligible carbs).
Important: Carb counting requires careful label reading and portion measurement. It is essential to work with a diabetes educator or dietitian to learn this method correctly and establish your personal carb targets.
Understanding Glycemic Index (GI) and Glycemic Load (GL)
The Glycemic Index is another tool that can help you make smart food choices.
It’s a ranking of carbohydrate-containing foods based on how quickly they raise blood glucose levels after being eaten.
- Low-GI foods (55 or less): Cause a slower, smaller rise in blood sugar. Examples include whole grains, legumes, nuts and most fruits and vegetables.
- High-GI foods (70 or more): Cause a rapid spike in blood sugar. Examples include white bread, potatoes and sugary snacks.
Glycemic Load (GL) takes it a step further by considering the portion size.
It gives a more accurate picture of a food’s real-world impact on your blood sugar.
While useful, most experts agree that focusing on the Plate Method and overall healthy eating patterns is a more practical and sustainable approach for most people than strictly tracking GI or GL.
Meal Planning Methods at a Glance
| Method | Best For | Pros | Cons |
|---|---|---|---|
| The Plate Method | Beginners and those looking for a simple, visual approach. | Easy to understand, no counting or measuring required, promotes balanced meals. | Less precise, may not be suitable for those on complex insulin regimens. |
| Carbohydrate Counting | Individuals on mealtime insulin or those who want more flexibility and precision. | Allows for precise insulin dosing, offers more food choice flexibility. | Requires significant education, diligence in measuring and tracking, can be time-consuming. |
A Sample 7-Day Diabetic Meal Plan for Beginners
This sample plan uses the principles of the Plate Method and focuses on whole foods.
Portions should be adjusted based on your individual needs, activity level and healthcare provider’s recommendations.
- Day 1
- Breakfast: ½ cup rolled oats cooked with water or low-fat milk, topped with ½ cup berries and 1 tbsp chopped walnuts.
- Lunch: Large salad with mixed greens, cucumber, tomatoes, grilled chicken breast (4 oz) and a light vinaigrette. 1 small whole-wheat pita.
- Dinner: Baked salmon (4 oz), 1 cup steamed broccoli, and ½ cup quinoa.
- Snack: An apple with 1 tbsp of natural almond butter.
- Day 2
- Breakfast: 2 scrambled eggs with spinach and a side of ½ avocado. 1 slice of 100% whole-wheat toast.
- Lunch: Leftover baked salmon and quinoa from dinner.
- Dinner: Turkey and black bean chili (using lean ground turkey), topped with a dollop of plain Greek yogurt.
- Snack: Small handful of almonds.
- Day 3
- Breakfast: ¾ cup plain Greek yogurt with ½ cup sliced peaches and 1 tbsp chia seeds.
- Lunch: Leftover turkey and black bean chili.
- Dinner: Chicken stir-fry (4 oz chicken) with a large portion of mixed vegetables (broccoli, bell peppers, snap peas) and a light, low-sodium soy sauce. Served with ½ cup brown rice.
- Snack: Baby carrots with 2 tbsp hummus.
- Day 4
- Breakfast: Smoothie made with 1 cup unsweetened almond milk, a handful of spinach, ½ cup frozen berries and 1 scoop of protein powder.
- Lunch: Quinoa salad with chickpeas, diced cucumber, tomatoes, parsley and a lemon-olive oil dressing.
- Dinner: Lean pork chop (4 oz), roasted asparagus and a small baked sweet potato.
- Snack: A pear.
- Day 5
- Breakfast: 2 scrambled eggs with a side of sautéed mushrooms and onions.
- Lunch: Leftover pork chop and asparagus.
- Dinner: Whole-wheat pasta (1 cup cooked) with a lean ground turkey marinara sauce (check for no added sugar) and a large side salad.
- Snack: Low-fat cottage cheese.
- Day 6
- Breakfast: ½ cup rolled oats cooked with water, topped with a sliced small banana and a sprinkle of cinnamon.
- Lunch: Leftover whole-wheat pasta and meat sauce.
- Dinner: Tofu and vegetable skewers (bell peppers, zucchini, onions) grilled or baked, served with ½ cup farro.
- Snack: Celery sticks with 1 tbsp natural peanut butter.
- Day 7
- Breakfast: ¾ cup plain Greek yogurt with a handful of raspberries and 1 tbsp flax seeds.
- Lunch: Large salad topped with a can of tuna (in water, drained), mixed with 1 tbsp of plain yogurt and herbs.
- Dinner: Homemade lentil soup packed with vegetables (carrots, celery, onions). 1 slice of whole-wheat bread on the side.
- Snack: A small orange.
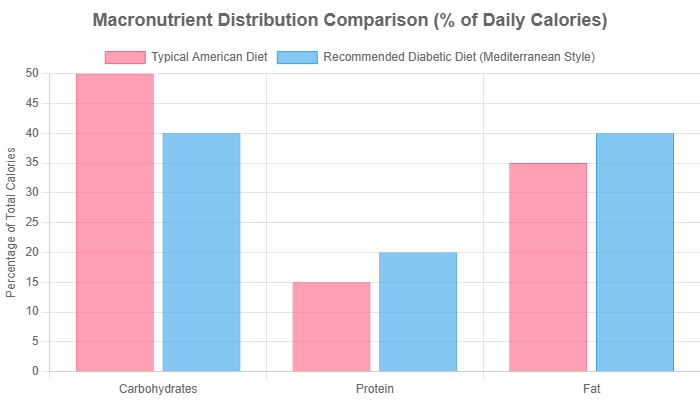
Chart illustrates a shift from higher carbohydrate intake to a balance with more protein and healthy fats, typical of a Mediterranean-style eating pattern recommended for diabetes management. Actual percentages should be personalized.
How Can I Make My Diabetic Diet Easier and More Sustainable?
A diet is only effective if you can stick with it long-term.
The key to success is building healthy habits that fit into your real life.
This section provides practical, experience-based tips to overcome common challenges and make your diabetic diet a sustainable lifestyle.
Smart Grocery Shopping & Reading Nutrition Labels
Success starts at the grocery store. What you bring into your house determines what you’ll eat.
- Shop the Perimeter: The outer aisles of most stores are where you’ll find fresh produce, lean meats, fish and dairy—the core of your diet. Venture into the center aisles with a specific list for items like whole grains, beans and healthy oils.
- Never Shop Hungry: Shopping on an empty stomach leads to impulse buys, which are rarely healthy choices.
- Become a Label Detective: Reading the Nutrition Facts panel is a non-negotiable skill. Focus on these key areas:
- Serving Size: All the numbers on the label apply to this amount. If you eat double the serving size, you must double all the numbers.
- Total Carbohydrates: This is your primary number for blood sugar management.
- Dietary Fiber: A higher fiber content is better. It helps slow sugar absorption.
- Added Sugars: Aim for this number to be as low as possible, ideally zero.
- Sodium: Compare brands and choose the option with the lowest sodium content.
Meal Prepping for a Week of Healthy Eating
Meal prepping is your secret weapon against last-minute unhealthy choices.
Dedicating a few hours on the weekend can set you up for a week of success.
- Cook Grains in Batches: Cook a large pot of quinoa, brown rice, or farro. Store it in the fridge to easily add to meals throughout the week.
- Chop Veggies Ahead of Time: Wash and chop carrots, bell peppers, celery, and broccoli. Store them in containers for quick snacks or to toss into stir-fries and salads.
- Portion Out Snacks: Instead of eating from a large bag, portion out nuts, seeds, or whole-grain crackers into small, single-serving bags.
- Prepare Proteins: Grill several chicken breasts or hard-boil a dozen eggs to have ready-to-go protein for salads and lunches.
Navigating Restaurants and Social Gatherings
A diabetes diagnosis doesn’t mean you can’t enjoy eating out. It just requires a little planning.
- Be a Menu Scout: Look up the restaurant’s menu online before you go. Decide on a healthy option in advance to avoid being tempted by less-healthy choices in the moment.
- Control the Preparation: Don’t be afraid to make special requests. Ask for sauces, dressings, and gravies on the side. Request that your food be grilled, baked, or steamed instead of fried.
- Start with a Salad: Begin your meal with a large green salad (with a light vinaigrette on the side). This helps fill you up with fiber, so you’re less likely to overeat the main course.
- Watch Your Portions: Restaurant portions are often two to three times a normal serving size. Plan to eat only half and take the rest home for another meal.
- At Parties: Don’t arrive starving. Have a small, healthy snack before you go. Position yourself away from the food table to avoid mindless grazing.
Budget-Friendly Tips for a Diabetic Diet
Eating healthy doesn’t have to be expensive. With a few smart strategies, you can manage your blood sugar without breaking the bank.
- Embrace Plant-Based Proteins: Dried beans, lentils, and chickpeas are incredibly inexpensive, nutritious, and shelf-stable. Make them a staple.
- Buy Frozen Produce: Frozen fruits and vegetables are just as nutritious as fresh (sometimes more so, as they’re frozen at peak ripeness) and are often much cheaper, especially for out-of-season items.
- Shop In-Season: Fresh produce is cheapest and most flavorful when it’s in season. Plan your meals around what’s currently available.
- Buy in Bulk: Items like oats, brown rice, and quinoa are often cheaper per unit when purchased from the bulk bins.
- Cook at Home: The single biggest way to save money is to cook your own meals instead of eating out or buying pre-packaged foods.
Your Top Questions About the Diabetic Diet Answered
Here are direct, concise answers to some of the most common questions people have when starting a diabetic diet.
1. Can I still eat dessert on a diabetic diet?
Yes, in moderation. The key is portion control and planning. A small portion of a dessert after a balanced meal will have less impact than eating it on an empty stomach. Opt for fruit-based desserts or share a small treat.
2. What are the best snacks for a diabetic?
The best snacks combine protein, healthy fat, and fiber. Think a small apple with almond butter, plain Greek yogurt with berries, a handful of nuts, or veggie sticks with hummus. These combinations help stabilize blood sugar between meals.
3. How do artificial sweeteners affect diabetes?
FDA-approved artificial sweeteners don’t raise blood sugar levels. However, their long-term health effects are still debated. They can be a useful tool for reducing sugar intake, but the focus should always be on consuming whole, naturally unsweetened foods and drinks.
4. Can I drink alcohol if I have diabetes?
Consult your doctor first. If you do drink, do so in moderation (one drink/day for women, two for men) and always with food. Alcohol can cause hypoglycemia (low blood sugar), especially if you take insulin or certain medications.
5. Is the keto diet good for diabetics?
While a very-low-carb ketogenic diet can lower blood sugar, it’s highly restrictive and its long-term safety and sustainability are debated. The Mediterranean and DASH diets have more robust, long-term evidence for diabetes management and overall health.
6. How much fruit can a diabetic eat per day?
Most people can include 2-3 servings of fruit per day. A serving is a small piece of whole fruit or about 1 cup of berries. It’s best to spread fruit intake throughout the day rather than eating it all at once.
7. Do I need to eat special “diabetic” foods?
No. Most foods marketed as “diabetic” are expensive and unnecessary. A healthy diabetic diet consists of the same whole foods recommended for everyone. These special products can also sometimes contain sugar alcohols, which may cause digestive issues.
8. How often should I eat to manage my blood sugar?
Most people benefit from eating three balanced meals per day, spaced about 4-5 hours apart. Some individuals, especially those at risk for hypoglycemia, may also need one or two small snacks. Consistency is key to keeping blood sugar stable.
9. What is the best breakfast for a diabetic?
A great diabetic breakfast includes protein, fiber, and healthy fats. Examples are scrambled eggs with spinach and avocado, plain Greek yogurt with berries and nuts, or oatmeal (not instant) with a sprinkle of chia seeds and walnuts.
10. Can a diabetic diet reverse type 2 diabetes?
For some people, particularly those newly diagnosed and who achieve significant weight loss, it is possible to achieve diabetes remission. This means blood sugar levels return to a non-diabetic range without medication. A healthy diet is the cornerstone of this approach.
Conclusion
Embarking on a diabetic diet is one of the most powerful and positive actions you can take for your health.
It’s a journey that moves away from a mindset of restriction and toward one of mindful, nourishing choices.
As we’ve explored, this eating pattern is not about deprivation, it’s about balance, nutrient-density and portion control.
By filling your plate with vibrant vegetables, lean proteins, healthy fats, and high-fiber carbohydrates, you are not just managing a condition—you are actively investing in a future with more energy, fewer complications and a greater sense of well-being.
Every healthy meal is a step toward taking control of your diabetes, rather than letting it control you.
Frame these changes as a sustainable and empowering lifestyle choice. You have the knowledge and the tools to build a healthier, more vibrant life.
Medical Disclaimer: The information in this article is for educational purposes only and is not intended as a substitute for professional medical advice, diagnosis or treatment. Your health journey is unique.
We strongly recommend you consult with a registered dietitian (RDN) or your healthcare provider to create a personalized diabetic diet plan that fits your specific medical needs, lifestyle and goals.
We’d love to hear from you! Share your favorite diabetic-friendly meal or a helpful tip in the comments below!
References
- Centers for Disease Control and Prevention (CDC). (2024). National Diabetes Statistics Report. https://www.cdc.gov/diabetes/php/data-research/index.html
- American Diabetes Association. (2023). American Diabetes Association Releases Standards of Care in Diabetes—2024. https://diabetes.org/newsroom/press-releases/american-diabetes-association-releases-standards-care-diabetes-2024
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (2023). Healthy Living with Diabetes. https://www.niddk.nih.gov/health-information/diabetes/overview/diet-eating-physical-activity
- Mayo Clinic Staff. (2024). Diabetes diet: Create your healthy-eating plan. https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-diet/art-20044295
- Reynolds, A. N., & Venn, B. J. (2024). Dietary Advice For Individuals with Diabetes. In K. R. Feingold et al. (Eds.), Endotext. MDText.com, Inc. https://www.ncbi.nlm.nih.gov/books/NBK279012/
- Sami, W., et al. (2017). Effect of diet on type 2 diabetes mellitus: A review. Journal of Education and Health Promotion, 6, 109. https://pmc.ncbi.nlm.nih.gov/articles/PMC5426415/
- Centers for Disease Control and Prevention (CDC). (2024). Diabetes Meal Planning. https://www.cdc.gov/diabetes/healthy-eating/diabetes-meal-planning.html

