The most common early sign of testicular cancer is a painless lump or swelling on either testicle.
Early detection is crucial as this cancer is highly treatable, with a 5-year survival rate of over 95%.
While the diagnosis can be frightening, understanding the signs and acting quickly are the most powerful steps you can take toward a positive outcome.
This disease presents a paradox: it is the most common cancer diagnosed in American men between the ages of 15 and 35, yet it remains relatively rare overall.
According to the American Cancer Society, about 1 in every 250 males will develop testicular cancer in their lifetime. However, thanks to highly effective treatments, the lifetime risk of dying from it is remarkably low—about 1 in 5.000.
This incredible success story is built on a foundation of awareness and early intervention.
This comprehensive guide is designed to empower you with knowledge.
We will delve into the specific signs and symptoms of testicular cancer, providing detailed descriptions of what to look for.
You will learn the correct method for performing a monthly testicular self-exam, understand the critical risk factors, and gain clarity on what to do if you discover something concerning.
We will also explore common benign conditions to help differentiate them from cancer, reducing unnecessary anxiety while emphasizing the need for professional evaluation.
Knowledge and awareness are your most powerful tools for safeguarding your healt, let this guide be your first step.
In This Article
The Fundamentals of Testicular Cancer
What Exactly Is Testicular Cancer?
At its core, testicular cancer is a malignancy that originates in one or both testicles (also called *testes*).
The testicles are two oval-shaped male reproductive glands housed within the scrotum, a pouch of skin located below the penis.
These glands serve two primary, vital functions: the production of sperm for reproduction and the synthesis of male hormones, most notably testosterone.
The cancer begins when cells within a testicle start to grow and divide uncontrollably, forming a mass or tumor.
Over 90% of testicular cancers develop in specialized cells known as germ cells, which are the cells that produce sperm.
For reasons that are not yet fully understood, the DNA within these cells can undergo changes that disrupt their normal life cycle, leading to malignant growth.
Testicular germ cell tumors are broadly classified into two main types, and this distinction is critical for determining the appropriate treatment strategy:
- Seminomas: This type of testicular cancer tends to grow and spread more slowly than nonseminomas. They are particularly sensitive to radiation therapy and chemotherapy. Seminomas are more common in men in their late 20s and early 40s.
- Nonseminomas: This category includes several subtypes of cancer (such as embryonal carcinoma, yolk sac carcinoma, choriocarcinoma and teratoma). Nonseminomas typically develop earlier in life, usually in a man’s late teens to early 30s, and tend to be more aggressive, growing and spreading more rapidly than seminomas.
While testicular cancer is the most prevalent malignancy in its specific demographic, it accounts for only about 1% of all cancers in men.
The National Cancer Institute’s SEER Program projects approximately 9.720 new cases in the United States for 2025, highlighting its relative rarity in the broader population.
This unique epidemiological profile makes targeted awareness campaigns and education on self-examination profoundly important.
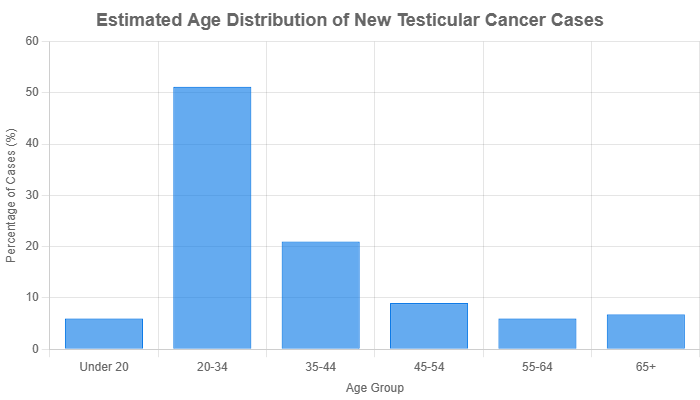
Estimated new cases of testicular cancer by age group in the U.S. Data shows a significant peak in young adulthood. Source: NCI SEER Program.
Why Is Early Detection So Critically Important?
The prognosis for testicular cancer is one of the most optimistic in oncology, but this success is directly tied to the stage at which the disease is diagnosed.
Early detection is not just beneficial, it is the single most important factor determining the simplicity of treatment, long-term health outcomes, and overall survival.
“Testicular cancer is one of the few cancers that—with almost all patients—we can cure the patient, even if they present with metastatic disease”, says Thomas Schwaab, MD, PhD, of Roswell Park Comprehensive Cancer Center. However, he adds, “A small testis tumor has a better prognosis than a large testis tumor”.
The connection between detection stage and survival is stark. According to the American Cancer Society, the 5-year relative survival rates are:
- 99% for localized testicular cancer (cancer that has not spread beyond the testicle).
- 96% for regional cancer (cancer that has spread to nearby lymph nodes).
- 73% for distant cancer (cancer that has metastasized to distant parts of the body like the lungs, liver or brain).
These statistics powerfully illustrate that when testicular cancer is caught before it has a chance to spread, it is almost always curable.
The primary goal of early detection is to identify the tumor while it is still confined to the testicle.
Furthermore, the stage of diagnosis dictates the intensity of the treatment required.
For early-stage, localized testicular cancer, the standard treatment is a surgical procedure called a *radical inguinal orchiectomy*, which involves the removal of the affected testicle and spermatic cord through a small incision in the groin.
For many men with Stage I cancer, this surgery may be the only treatment needed, followed by a period of active surveillance.
In contrast, later-stage cancer that has spread often requires multiple cycles of intensive chemotherapy and potentially radiation therapy or additional complex surgeries to remove affected lymph nodes.
These treatments, while life-saving, carry a greater burden of short-term and long-term side effects.
For the young men most affected by this disease, preserving fertility and long-term health is a major concern.
Early-stage treatment is significantly less likely to impact fertility.
While the removal of one testicle does not typically affect a man’s ability to have children or his testosterone levels, chemotherapy and radiation can have temporary or permanent effects on sperm production.
By detecting the cancer early, patients can often avoid these more aggressive therapies, thereby better preserving their future reproductive options and overall well-being.
The Core – Recognizing the Early Signs and Symptoms
What Are the Most Common Early Signs of Testicular Cancer?
Recognizing the early signs of testicular cancer begins with knowing what to look for.
While the disease can manifest in several ways, a few key symptoms are most common.
If you experience any of the following, it is essential to pay attention and consult a healthcare professional.
These signs are your body’s primary alert system.
- A Lump or Enlargement in Either Testicle: This is the hallmark sign of testicular cancer. The lump is often, but not always, painless and can range in size from as small as a pea to as large as a marble or even bigger.
- A Feeling of Heaviness in the Scrotum: Some men report that the affected side of their scrotum feels heavier or more solid than usual, even without a distinct lump.
- A Dull Ache in the Abdomen or Groin: A persistent, dull pain or pressure in the lower belly or groin area can be a symptom. This is different from the sharp pain of an injury.
- A Sudden Collection of Fluid in the Scrotum: A rapid accumulation of fluid around the testicle, known as a *hydrocele*, can sometimes be associated with an underlying tumor.
- Pain or Discomfort in a Testicle or the Scrotum: While most lumps are painless, some men do experience pain, tenderness, or a general sense of discomfort in the testicle or scrotum.
- Enlargement or Tenderness of the Breast Tissue: Known as *gynecomastia*, this surprising symptom can occur because certain types of testicular tumors secrete high levels of the hormone hCG (human chorionic gonadotropin), which stimulates breast tissue growth.
- A Significant Change in the Size or Shape of a Testicle: One testicle may become noticeably larger, firmer or change in its overall shape compared to the other.
It is important to remember that testicular cancer usually affects only one testicle.
Any asymmetry or difference between the two that is new or changing should be evaluated.
What Does a Testicular Cancer Lump Actually Feel Like?
This is one of the most frequent and important questions men have.
The abstract idea of a “lump” can be confusing, so understanding its typical characteristics is vital for accurate self-assessment.
While every case is unique, there are common descriptions that can help guide you.
The most critical feature to understand is that **a cancerous lump is almost always part of the testicle itself**.
It feels like a hard, fixed irregularity on the otherwise smooth, oval surface of the testicle.
Imagine a smooth, hard-boiled egg, a cancerous lump might feel like a small, hard pea or a piece of gravel that has become embedded in its surface.
It typically does not move separately from the testicle when you palpate it.
Key characteristics of a potentially cancerous lump include:
- Hardness: The lump is often very firm or hard, unlike the spongy feel of the testicle itself. It has been described as feeling like a small rock or a piece of uncooked rice.
- Painless Nature: This is a crucial and often misunderstood point. The vast majority of testicular cancer lumps are **painless**. The absence of pain should not provide a false sense of security, in fact, a painless, hard lump is more suspicious for cancer than a painful one. Pain is more commonly associated with infections (like epididymitis), torsion (twisting of the spermatic cord) or injury.
- Irregular Shape: While some lumps can be smooth and round, many are irregular in shape. The key is that it represents a change from the normal, smooth contour of the testicle.
- Location: Lumps are typically found on the front or side of the testicle. This helps distinguish them from the *epididymis*, a soft, rope-like tube located at the back of each testicle. The epididymis is a normal part of your anatomy, and it’s common to mistake it for an abnormality if you’re not familiar with how it feels. Learning to identify your epididymis is a key part of an effective self-exam.
In summary, the classic presentation of a testicular cancer lump is a hard, painless, fixed mass on the surface of the testicle. Any such finding warrants an immediate visit to a doctor.
Are There Other, More Subtle, Changes to Watch For?
While a distinct lump is the most well-known sign, testicular cancer can also present with more subtle, ambiguous symptoms.
Being aware of these less obvious changes is equally important, as they can be the earliest indicators of a problem.
A Sensation of Heaviness: This symptom can be difficult to describe but is frequently reported by patients. It’s a feeling that one testicle has become denser or heavier than the other. It might not be a noticeable weight difference if you were to hold them, but rather an internal sensation of fullness or dragging in that side of the scrotum. This can occur even without a palpable lump, as the tumor grows within the testicular tissue, increasing its overall density.
A Persistent Dull Ache: Unlike the sharp, acute pain of an injury, the ache associated with testicular cancer is typically low-grade, persistent, and located in the lower abdomen, groin, or the scrotum itself. It might come and go but doesn’t fully resolve. Men sometimes dismiss this as a muscle strain or the result of exercise, but if it lingers for more than a week or two without a clear cause, it should be investigated.
Change in Size, Shape, or Consistency: Sometimes, a testicle may simply begin to grow larger or feel firmer than its counterpart without a single, distinct lump. The entire testicle might feel more solid or “woody”. It’s normal for one testicle to be slightly larger or hang lower than the other, but a *change* in this baseline asymmetry is a red flag. Any noticeable increase in size or a change from a soft, yielding consistency to a firm, unyielding one needs to be checked.
Breast Tenderness or Growth (Gynecomastia): As mentioned earlier, this is a less common but very significant sign. Certain nonseminoma tumors, particularly choriocarcinomas, produce the hormone hCG. In men, elevated hCG can stimulate breast tissue, leading to tenderness, swelling and even noticeable growth. While there are many other causes of gynecomastia, its appearance in conjunction with any other testicular change is highly suspicious for testicular cancer.
In some advanced cases, the first symptoms may not be in the testicles at all, but related to where the cancer has spread. These can include persistent lower back pain (from spread to retroperitoneal lymph nodes), shortness of breath or a cough (from lung metastases) or abdominal pain (from liver or lymph node involvement).
Taking Action – Your Guide to the Testicular Self-Exam (TSE)
How Do You Perform a Monthly Testicular Self-Exam?
A testicular self-exam (TSE) is a simple, quick, and effective way to become familiar with your body and detect any changes early. Performing it correctly and consistently is key.
The following step-by-step guide, recommended by organizations like the American Cancer Society and urologists worldwide, can be completed in just a few minutes.
- Choose the Right Time and Place. The best time to perform a TSE is during or immediately after a warm shower or bath. The warmth relaxes the skin of the scrotum, making it thinner and more pliable, which allows you to feel the testicles and their internal structures more easily.
- Examine Visually in a Mirror. Stand in front of a mirror and look at your scrotum. Check for any visible swelling, redness or changes to the skin. It’s normal for one testicle to hang lower or be slightly larger than the other, but you are looking for any *new* changes in this appearance.
- Examine Each Testicle Separately. Focus on one testicle at a time. Use one hand to gently support the scrotum and the other hand to perform the examination. This prevents the testicle from moving around too much.
- Use a Gentle Rolling Motion. Place your thumb on the front of the testicle and your index and middle fingers behind it. Gently but firmly roll the testicle between your thumb and fingers. The goal is to feel the entire surface area. The testicle should feel smooth, oval-shaped, and fairly firm, but not rock-hard.
- Feel for Lumps, Bumps and Changes. As you roll the testicle, be methodical. Feel for any hard lumps, firm nodules, smooth rounded bumps, or any changes in the size, shape, or consistency of the testicle. Remember, a cancerous lump is typically painless.
- Know Your Normal Anatomy. At the back of each testicle is a soft, rope-like structure called the *epididymis*. It runs up the back of the testicle and its function is to store and transport sperm. It can feel somewhat lumpy or tender, which is normal. It is crucial to locate your epididymis and learn what it feels like so that you do not mistake it for an abnormal lump on the testicle itself.
- Repeat on the Other Side. Once you have thoroughly examined one testicle, repeat the exact same process on the other one.
If you find anything unusual—a hard lump, a change in size, pain or swelling—contact your doctor without delay.
When Should You Start and How Often Should You Check?
Given that testicular cancer is most common in adolescents and young men, medical experts recommend that monthly self-exams begin during the teenage years, typically around age 15.
Starting at this age helps establish a lifelong habit of health awareness.
The key to an effective self-examination routine is **consistency**. The exam should be performed **once a month**.
This regular frequency allows you to establish a clear baseline of what feels normal for your own body.
Every man’s anatomy is slightly different.
By checking monthly, you become an expert on your own “normal”.
This familiarity is what will enable you to quickly and confidently identify any new lump, swelling, or change that deviates from that baseline.
Think of it like checking the tire pressure on your car. You do it regularly not because you expect to find a problem every time, but to ensure that when a problem does arise, you catch it before it becomes a major issue.
A monthly TSE is a small investment of time that offers a significant return in peace of mind and proactive health management.
Gaining Context – Is It Cancer or Something Else?
Could This Lump Be Something Other Than Cancer?
Discovering a lump or swelling in your scrotum can be an alarming experience, and it’s natural for your mind to jump to the worst-case scenario.
However, it is important to know that the vast majority of scrotal lumps are not cancerous.
There are several common, benign (non-cancerous) conditions that can cause similar symptoms.
Understanding these can help manage anxiety, but it does not replace the need for a professional diagnosis.
Below is a table comparing testicular cancer with common benign conditions. This is for informational purposes only.
| Condition | Typical Feeling & Symptoms | Is it Cancerous? |
|---|---|---|
| Testicular Cancer | A hard, firm, often painless lump located on the testicle itself. May be accompanied by heaviness or a dull ache. | Yes (Malignant) |
| Epididymal Cyst (Spermatocele) | A small, smooth, movable, fluid-filled sac located on the epididymis (the tube at the back of the testicle). It feels separate from the testicle. | No (Benign) |
| Varicocele | Enlargement of the veins within the scrotum, often described as feeling like a “bag of worms”. More noticeable when standing. Can cause a dull ache. | No (Benign) |
| Hydrocele | A painless buildup of fluid in the sac surrounding the testicle, causing the scrotum to swell. The testicle itself may be difficult to feel. | No (Benign) |
| Epididymitis/Orchitis | Inflammation/infection of the epididymis or testicle. Causes significant pain, swelling, redness and warmth. Often accompanied by fever. | No (Infection/Inflammation) |
| Inguinal Hernia | Occurs when part of the intestine pushes through a weak spot in the abdominal muscles into the scrotum. Causes a bulge that may be more prominent when coughing. | No (Structural Issue) |
Crucial Disclaimer: While this table provides general guidance, the symptoms of these conditions can overlap. It is impossible to distinguish between them with certainty through self-exam alone. Only a doctor, often with the help of an ultrasound, can make an accurate diagnosis. Any new lump, swelling, or persistent change you discover requires a professional medical evaluation to rule out testicular cancer.
What Are the Known Risk Factors for Testicular Cancer?
While the exact cause of testicular cancer is unknown, researchers have identified several factors that increase a man’s risk of developing the disease.
It’s important to note that having one or more risk factors does not mean you will get cancer, and many men who develop testicular cancer have no known risk factors.
The most significant risk factors, as identified by institutions like the Mayo Clinic and the National Cancer Institute, include:
- Undescended Testicle (Cryptorchidism): This is the single most significant risk factor. During fetal development, the testicles form in the abdomen and normally descend into the scrotum before birth. If a testicle fails to descend, the risk of developing cancer in that testicle is substantially higher, even if it is later surgically moved to the scrotum (a procedure called orchiopexy).
- Family History: Having a close relative—specifically a father or brother—who has had testicular cancer increases your risk. The risk is higher if a brother was affected than if the father was.
- Personal History of Testicular Cancer: Men who have had cancer in one testicle have a 3-4% chance of developing it in the other testicle over their lifetime. This is why ongoing surveillance is critical after an initial diagnosis.
- Age: This is a disease of the young. While it can occur at any age, about half of all cases are diagnosed in men between the ages of 20 and 34. It is the most common solid tumor in this age group.
- Race and Ethnicity: For reasons that are not well understood, testicular cancer is significantly more common in White men in the United States and Europe than in Black, Asian American or Hispanic men. The global incidence has been rising for several decades, particularly in industrialized nations.
- Carcinoma in Situ (CIS): This is a non-invasive form of testicular cancer where abnormal germ cells are present but have not spread. It is sometimes found during a biopsy for infertility and significantly increases the risk of developing invasive testicular cancer later.
Factors like injury or trauma to the testicles have **not** been shown to cause testicular cancer, although an injury may sometimes lead to a doctor’s visit where a pre-existing tumor is discovered incidentally.
The Next Steps – Seeking Professional Help
When Exactly Should You See a Doctor?
The rule for seeking medical advice is simple, clear, and absolute: do not wait.
You should schedule an appointment with your primary care physician or a urologist (a specialist in the urinary tract and male reproductive system) if you discover:
- Any lump or hard area on your testicle.
- Any swelling of your scrotum or testicle.
- Any change in the size, shape, or consistency of your testicle.
- Any persistent dull ache or feeling of heaviness in your scrotum, groin, or lower abdomen.
Even if you think it’s “probably nothing”, it is always best to have it professionally evaluated.
The guideline often cited by medical professionals is to see a doctor for any of these changes that persist for **more than two weeks**.
However, for a distinct, hard lump on the testicle, there is no reason to wait at all.
It is completely understandable to feel fear, anxiety or embarrassment about this type of health concern.
Many men delay seeking help out of fear of the diagnosis or awkwardness about the physical exam.
Please, do not let these feelings stop you.
A brief and professional medical appointment can provide peace of mind or, if necessary, start a life-saving treatment process.
A few minutes of potential discomfort are an infinitesimally small price to pay for your long-term health.
Your future self will thank you for your courage and proactivity.
What Happens at the Doctor’s Appointment?
Knowing what to expect at a doctor’s appointment can help alleviate anxiety.
The diagnostic process for a suspected testicular issue is standardized and straightforward.
- Medical History and Discussion: The appointment will begin with a conversation. Your doctor will ask you about the symptoms you’ve noticed, when you first observed them, whether you have any pain, and about your personal and family medical history, including any risk factors for testicular cancer.
- Physical Examination: The doctor will then perform a physical exam. This will involve carefully feeling the testicles, epididymis, and surrounding areas of the scrotum to assess the location, size, and consistency of any abnormality. They will also likely examine your abdomen and lymph node areas.
- Scrotal Ultrasound: If the physical exam reveals a suspicious lump or swelling, the next step is almost always a scrotal ultrasound. This is a quick, painless, and non-invasive imaging test. You will lie on an exam table, a clear gel will be applied to your scrotum, and a small, handheld probe (a transducer) will be moved over the skin. The transducer emits sound waves that bounce off the structures inside your scrotum and create a real-time image on a monitor. This test is extremely reliable for determining if a mass is solid (which is more likely to be cancer) or filled with fluid (like a cyst).
- Blood Tests (Tumor Markers): The doctor will likely order a blood test to check for specific proteins called tumor markers. The main markers for testicular cancer are alpha-fetoprotein (AFP), human chorionic gonadotropin (hCG), and lactate dehydrogenase (LDH). Elevated levels of these markers can strongly suggest the presence of a testicular germ cell tumor and can also help determine the type (seminoma vs. nonseminoma).
- The Definitive Diagnosis: It is critical to understand that while the ultrasound and blood tests can provide strong evidence, the only way to confirm a diagnosis of testicular cancer is by surgically removing the affected testicle and examining its tissue under a microscope (biopsy). This procedure is the radical inguinal orchiectomy mentioned earlier. A needle biopsy of the testicle is not performed because it risks spreading the cancer cells into the scrotum. If cancer is highly suspected, removal of the entire testicle is both the diagnostic and the initial therapeutic step.
Based on these results, your medical team will determine if cancer is present, and if so, will proceed with further imaging tests (like a CT scan) to determine its stage and plan the next steps in your treatment.
Frequently Asked Questions (FAQ)
1. Can you get testicular cancer in both testicles?
It is very rare, but possible. It can occur at the same time (synchronous) or, more commonly, a man who has had cancer in one testicle may develop it in the other years later (metachronous). The lifetime risk for the second testicle is about 3-4%.
2. Is testicular cancer painful?
Usually, it is not. The most common sign is a painless, hard lump. While some men do experience pain or discomfort, the absence of pain is more typical for a cancerous tumor and should not be a reason to delay seeing a doctor.
3. Can a vasectomy cause testicular cancer?
No. Large-scale scientific studies have found no link between having a vasectomy and an increased risk of developing testicular cancer. This is a common myth that has been thoroughly debunked by medical research.
4. What is the survival rate for testicular cancer?
The overall 5-year relative survival rate is excellent, at about 95%. For cancer that is confined to the testicle (localized), the survival rate is 99%. Early detection is the key to these high cure rates.
5. At what age is testicular cancer most common?
Testicular cancer is most frequently diagnosed in adolescents and young men, with a peak incidence between the ages of 15 and 35. Approximately half of all cases occur in this age range, making it the most common cancer for this demographic.
6. Can you still have children after testicular cancer?
Yes, most men can. The removal of one testicle usually does not affect fertility, as the remaining testicle can produce enough testosterone and sperm. Chemotherapy or radiation can impact fertility, so sperm banking is often recommended before starting these treatments.
7. Does testicular cancer spread quickly?
It can. Testicular cancers, particularly nonseminomas, can be aggressive and metastasize (spread) relatively quickly to lymph nodes, lungs, or other organs. This is why prompt evaluation of any symptom is so critical to catching it at an early, localized stage.
8. Can an injury to the testicles cause cancer?
No, there is no scientific evidence that an injury or trauma to the testicles causes cancer. However, an injury might cause swelling or pain that leads a man to examine himself or see a doctor, leading to the incidental discovery of a pre-existing tumor.
Conclusion
The journey through understanding testicular cancer is one of empowerment.
We have seen that while the diagnosis is serious, the outlook is overwhelmingly positive, especially with early action.
The key takeaways are simple but life-saving: testicular cancer is highly curable, early detection is paramount, the most common sign is a painless lump and monthly self-exams are your first line of defense.
You are the foremost expert on your own body.
By integrating a simple, two-minute self-exam into your monthly routine, you build an intimate knowledge of what is normal for you, enabling you to spot any deviation immediately.
This is not about inducing anxiety, it is about fostering a proactive and confident relationship with your own health.
If this guide has prompted you to check yourself, or if you have found something that concerns you, the next step is clear and non-negotiable: schedule an appointment with your doctor.
Do not dismiss your concerns. Do not wait to see if it goes away. The courage to act on a potential concern is a profound act of self-care. Your future self will thank you for the diligence and bravery you show today.
Finally, awareness is a collective responsibility.
Share this information with your friends, brothers, sons, and partners.
By normalizing the conversation around men’s health and testicular self-exams, we can dismantle the stigma and fear that too often lead to dangerous delays.
Together, we can ensure that the remarkable success story of testicular cancer treatment continues for generations to come.
Reference
[1] Symptoms of testicular cancer
https://www.nhs.uk/conditions/testicular-cancer/symptoms
[2] Testicular Cancer – StatPearls – NCBI Bookshelf
https://www.ncbi.nlm.nih.gov/books/NBK563159
[3] Key Statistics for Testicular Cancer | American Cancer Society
https://www.cancer.org/cancer/types/testicular-cancer/about/key-statistics.html
[4] What are the five warning signs of testicular cancer?
https://www.roswellpark.org/cancertalk/202404/what-are-five-warning-signs-testicular-cancer
[5] Cancer Stat Facts: Testicular Cancer – SEER
https://seer.cancer.gov/statfacts/html/testis.html
[6] https://www.testicularcancersociety.org
[7] Cancer Stat Facts: Testicular Cancer – SEER
https://seer.cancer.gov/statfacts/html/testis.html
[8] Testicular Cancer Treatment Options – Arizona Oncology
https://arizonaoncology.com/testicular-cancer/treatment-options/
[9] 7 Signs of Testicular Cancer That Young Men Should Know
https://stvincents.org/about-us/news-press/news-detail?articleId=55663&publicid=461

