Testosterone Replacement Therapy (TRT) is a medical treatment designed to restore normal testosterone levels in men with diagnosed hypogonadism.
It can offer significant benefits for sexual function, energy, and mood, but also carries considerable risks that require careful evaluation.
With prescriptions in the U.S. soaring from 7.3 million in 2019 to over 11 million by 2024, understanding the full picture of TRT has never been more critical.
Many men consider TRT as a potential “fountain of youth” to combat the natural effects of aging.
However, the line between treating a legitimate medical condition and seeking an anti-aging formula is often blurred.
This comprehensive guide will dissect the science, weigh the evidence-based pros and cons, and provide the clarity you need to have an informed conversation with your healthcare provider about whether TRT is right for you.
In This Article
What is Testosterone and Why Does It Matter?
Testosterone is the primary male sex hormone, though it is present in both men and women in different amounts.
In men, it is produced mainly in the testicles and is responsible for the development of male primary and secondary sexual characteristics during puberty.
Its role, however, extends far beyond adolescence.
This crucial hormone acts as a master regulator for numerous bodily functions throughout a man’s life. According to the Mayo Clinic, testosterone is essential for maintaining:
- Bone Density: It helps keep bones strong and reduces the risk of osteoporosis.
- Fat Distribution: It influences where the body stores fat. Low levels can lead to increased body fat, particularly around the abdomen.
- Muscle Strength and Mass: Testosterone is a key driver of muscle protein synthesis, helping to build and maintain muscle.
- Facial and Body Hair: It stimulates the growth of hair characteristic of adult males.
- Red Blood Cell Production: It plays a role in erythropoiesis, the process of creating red blood cells in the bone marrow.
- Sex Drive (Libido): Testosterone is a primary driver of sexual desire.
- Sperm Production: It is vital for spermatogenesis, the process of producing sperm.
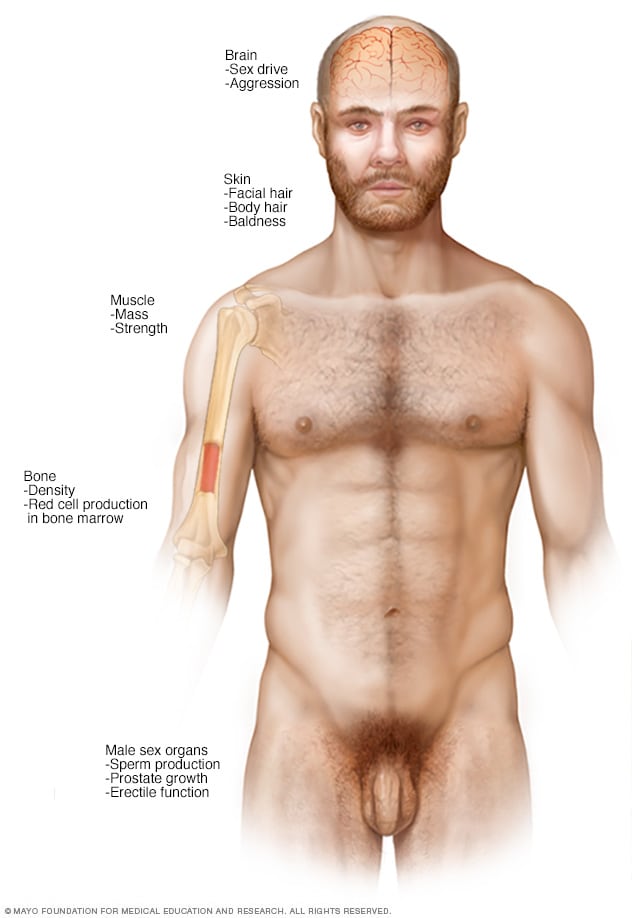
Testosterone influences multiple systems throughout the male body.
Low T: Differentiating Normal Aging from Clinical Hypogonadism
It’s a natural and expected part of aging for a man’s testosterone levels to decline.
Levels typically peak during adolescence and early adulthood.
After age 30 or 40, most men experience a gradual decline of about 1% per year.
This slow reduction is often called age-related low testosterone or “andropause”.
For many, this decline doesn’t cause significant issues.
However, a more severe or symptomatic drop in testosterone is classified as a medical condition called male hypogonadism.
The Endocrine Society defines hypogonadism as a syndrome comprising both symptoms and biochemical evidence of testosterone deficiency.
It’s crucial to distinguish this from the normal aging process, as TRT is only FDA-approved for treating diagnosed hypogonadism, not for combating the effects of aging.
What is Male Hypogonadism?
Hypogonadism occurs when the body cannot produce enough testosterone due to a problem with the testicles or the pituitary gland/hypothalamus in the brain. There are two main types:
- Primary Hypogonadism: This originates from a problem in the testicles themselves. They receive the signal to produce testosterone from the brain but are unable to do so adequately. Causes can include genetic disorders (like Klinefelter syndrome), physical injury to the testicles, or damage from chemotherapy or radiation.
- Secondary Hypogonadism: This occurs when the problem lies in the hypothalamus or pituitary gland. These parts of the brain fail to produce the hormones (Luteinizing Hormone – LH) that signal the testicles to make testosterone. Causes can include pituitary tumors, inflammatory diseases or certain medications.
The key takeaway is this: TRT is designed to treat a diagnosed medical failure (hypogonadism), not to reverse the natural, gradual decline of testosterone that comes with age. Treating normal aging with TRT is not recommended by major medical bodies like the American College of Physicians.
How is Low Testosterone (Hypogonadism) Diagnosed?
A diagnosis of hypogonadism is not made lightly.
Due to the non-specific nature of many symptoms, which can overlap with other conditions like depression, thyroid problems, or sleep apnea, a thorough evaluation is essential.
According to the American Urological Association (AUA) 2024 Guidelines, a diagnosis requires two key components:
- Presence of Signs and Symptoms: The patient must be experiencing symptoms consistent with low testosterone.
- Biochemical Confirmation: Blood tests must confirm unequivocally low testosterone levels.
Step 1: Symptom Evaluation
A healthcare provider will first assess for a pattern of symptoms, which can be categorized as physical, sexual and emotional changes.
- Sexual Symptoms: These are often the most specific indicators and include reduced sexual desire (low libido), difficulty achieving or maintaining erections (erectile dysfunction) and fewer spontaneous morning erections.
- Physical Symptoms: These can include increased body fat, reduced muscle mass and strength, decreased bone density (osteoporosis), loss of body or facial hair and swollen or tender breasts (gynecomastia).
- Emotional/Cognitive Symptoms: Patients may experience persistent fatigue, lack of energy, decreased motivation or self-confidence, feelings of sadness or depression and trouble with concentration or memory.
Step 2: Blood Testing
If symptoms are present, blood tests are the next step. The AUA provides clear guidance on this process:
- Two Separate Tests: A diagnosis should only be made after two separate total testosterone measurements, both showing low levels.
- Morning Samples: Blood must be drawn in the early morning (typically between 7 a.m. and 10 a.m.) when testosterone levels are at their peak. A level taken in the afternoon could be falsely low.
- The Cut-Off Value: The AUA uses a total testosterone level below 300 nanograms per deciliter (ng/dL) as a reasonable cut-off to support a diagnosis.
Your doctor may also order additional tests, such as for Luteinizing Hormone (LH) to determine if the hypogonadism is primary or secondary and a complete blood count to check for anemia or elevated red blood cells.
The Potential Benefits of TRT (The “Pros”)
For men with clinically diagnosed hypogonadism, TRT can offer life-changing improvements by restoring testosterone to a normal physiological range.
It’s important to note that these benefits are most pronounced in men who are truly deficient, the effects on men with borderline or age-related low testosterone are less clear and often minimal.
Improved Sexual Function
This is one of the most well-documented and consistent benefits of TRT.
A meta-analysis published in Andrology confirmed that TRT significantly improves libido (sexual desire).
Many men also report improvements in erectile function, though TRT is often less effective for ED caused by vascular or nerve issues.
For some, TRT may increase desire without fully resolving erection problems, requiring additional treatments.
Changes in Body Composition
Testosterone plays a direct role in regulating fat metabolism and muscle protein synthesis. Studies have consistently shown that TRT can lead to:
- An increase in lean body mass and muscle strength.
- A decrease in overall fat mass, particularly visceral fat (the dangerous fat around organs).
These changes are most effective when combined with a healthy diet and resistance exercise.
Enhanced Bone Mineral Density (BMD)
Testosterone is crucial for bone health, and long-term deficiency is a known risk factor for osteoporosis.
TRT has been shown to increase bone mineral density, particularly in the lumbar spine and hip.
However, the evidence on whether this translates to a lower fracture risk is conflicting.
A recent substudy of the TRAVERSE trial surprisingly found a numerically higher incidence of fractures in the testosterone group, a finding that requires more research.
Mood, Energy and Cognitive Improvements
Many men on TRT report subjective improvements in mood, energy levels and overall sense of well-being.
Some studies suggest it can alleviate depressive symptoms, particularly in men with both low T and depression.
However, evidence for cognitive benefits, such as improved memory or concentration, is weak and inconsistent.
The American College of Physicians notes there is little evidence that TRT improves vitality and energy in otherwise healthy men.
Correction of Anemia
Because testosterone stimulates red blood cell production, TRT can effectively correct unexplained anemia in hypogonadal men.
The TRAVERSE trial confirmed that TRT significantly increased hemoglobin levels and resolved anemia in a substantial portion of participants.
The Significant Risks and Side Effects of TRT (The “Cons”)
While the benefits can be appealing, TRT is not without significant risks and side effects.
These must be carefully weighed with your doctor, especially since therapy is often a lifelong commitment.
Once you start TRT, your body’s natural testosterone production shuts down, and it can be difficult and take a long time to recover if you decide to stop.
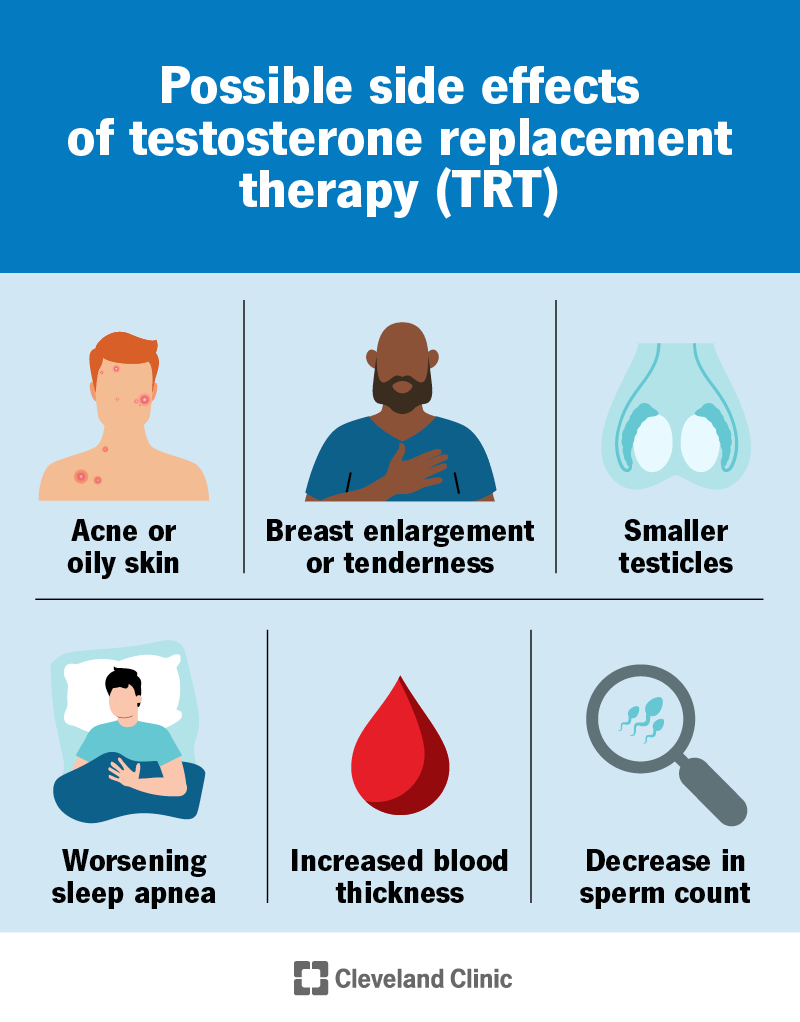
TRT comes with a range of potential side effects that require monitoring.
Cardiovascular Risks
The link between TRT and heart health has been a subject of intense debate.
In 2015, the FDA issued a warning about a possible increased risk of heart attack and stroke. However, the large-scale TRAVERSE trial, with results published in 2023 in the New England Journal of Medicine, provided much-needed clarity.
The study found that in men with hypogonadism and pre-existing or high risk of cardiovascular disease, TRT was not associated with an increased risk of major adverse cardiac events (like heart attack or stroke) compared to placebo.
Despite this reassuring top-line result, the trial did find a higher incidence of:
- Atrial Fibrillation (A-Fib): An irregular and often rapid heart rate.
- Pulmonary Embolism: A blood clot that travels to the lungs.
- Acute Kidney Injury.
Therefore, while the primary fear of heart attacks was not realized, other cardiovascular and related risks remain a concern.
Prostate Health
This is another long-standing concern. Testosterone can stimulate the growth of prostate tissue. For this reason, TRT can:
- Worsen symptoms of benign prostatic hyperplasia (BPH), such as urinary difficulties.
- Potentially stimulate the growth of existing, undiagnosed prostate cancer.
Current evidence, including from the TRAVERSE trial, does not show that TRT causes new cases of prostate cancer.
However, it is contraindicated in men with active prostate cancer.
Careful screening with a PSA test and digital rectal exam (DRE) is mandatory before starting therapy.
Erythrocytosis (Increased Red Blood Cell Count)
TRT stimulates the bone marrow to produce more red blood cells.
If the hematocrit (the percentage of red blood cells in the blood) gets too high (typically >54%), it thickens the blood.
This condition, called erythrocytosis or polycythemia, increases the risk of blood clots, which can lead to stroke or pulmonary embolism.
This is one of the most common side effects requiring dose adjustment or cessation of therapy.
Infertility and Testicular Atrophy
Exogenous (external) testosterone signals the brain to stop producing LH, the hormone that tells the testicles to make their own testosterone and sperm.
This leads to a sharp decrease in sperm production, causing infertility in most men on therapy.
It also causes the testicles to shrink (atrophy).
For men who wish to preserve their fertility, TRT is not a suitable option.
Alternative treatments like HCG or SERMs may be considered.
Other Common Side Effects
- Worsening Sleep Apnea: TRT can exacerbate pre-existing obstructive sleep apnea, a serious condition where breathing repeatedly stops and starts during sleep.
- Skin Reactions: Acne or oily skin is common. Gels and patches can cause skin irritation at the application site.
- Gynecomastia: Some testosterone can be converted to estrogen in the body, leading to breast tissue enlargement or tenderness.
- Fluid Retention: Swelling in the ankles (edema) can occur.
What Are the Different Types of TRT?
Testosterone therapy is available in several formulations, each with its own pros, cons and administration schedule.
The choice often comes down to a combination of patient preference, cost, insurance coverage and lifestyle.
According to a review in StatPearls, all FDA-approved methods aim to restore testosterone to the normal physiological range.
| Formulation | Administration | Pros | Cons |
|---|---|---|---|
| Injections (Cypionate, Enanthate) | Intramuscular or subcutaneous injection every 1-2 weeks. | Highly effective, low cost (especially generics), infrequent dosing. | Causes peaks and troughs in T levels (“roller coaster” effect), requires self-injection or office visits, potential for injection site pain. |
| Transdermal Gels (AndroGel, Testim, etc.) | Applied daily to the skin (shoulders, upper arms, thighs). | Provides stable, daily T levels; easy to apply. | Risk of transference to others (women, children) through skin contact; can cause skin irritation; can be expensive. |
| Transdermal Patches (Androderm) | Applied daily to the skin (back, abdomen, arms, thighs). | Mimics natural daily T rhythm. | High rate of skin irritation and rashes; may not adhere well with sweat; must rotate application sites. |
| Subdermal Pellets (Testopel) | Pellets are surgically implanted under the skin every 3-6 months. | Very convenient (“set it and forget it”); excellent compliance; stable T levels. | Requires a minor in-office surgical procedure for insertion and removal; risk of infection or pellet extrusion; dose cannot be easily adjusted. |
| Oral Capsules (Jatenzo) | Taken twice daily with food. | Avoids injections and skin applications. | Must be taken with fatty meals for absorption; can cause blood pressure increases (carries a black box warning); older oral forms were linked to liver toxicity. |
| Nasal Gel (Natesto) | Applied inside each nostril three times per day. | Rapid absorption; no risk of skin transference. | Inconvenient dosing schedule (3x/day); can cause nasal irritation, runny nose or nosebleeds. |
Who Should Not Use TRT?
TRT is not safe for everyone. The Endocrine Society and AUA guidelines list several absolute and relative contraindications.
You should not use TRT if you have:
- Prostate or Breast Cancer: Active cancer in these hormone-sensitive tissues is an absolute contraindication.
- Desire for Future Fertility: As TRT shuts down sperm production, it should be avoided by men planning to have children in the near term.
- Elevated Hematocrit: A high red blood cell count at baseline increases the risk of dangerous blood clots.
- Untreated Severe Obstructive Sleep Apnea: TRT can make this condition worse.
- Untreated Severe Heart Failure: The risk of fluid retention can be dangerous for patients with compromised heart function.
- A Recent Major Cardiovascular Event: The AUA recommends waiting 3-6 months after a heart attack or stroke before considering TRT.
- A High PSA Level or Prostate Nodule: These require further urological evaluation to rule out cancer before starting therapy.
How Much Does TRT Cost?
The cost of TRT can vary dramatically based on the type of therapy, insurance coverage, and whether you use brand-name or generic products.
The global TRT market was valued at over $2 billion in 2024, reflecting its widespread use.
- Injections: Generic testosterone cypionate is often the most affordable option, potentially costing as little as $40-$100 per month out-of-pocket for the medication and supplies.
- Gels: These are often more expensive. Without insurance, brand-name gels can cost $500-$800 or more per month. Generic versions and patient assistance programs can significantly lower this cost.
- Pellets: The cost of the pellets plus the in-office insertion procedure can range from $600 to $1.200 per treatment, which occurs every 3-6 months.
- Other Costs: Don’t forget to factor in the cost of doctor’s visits and regular lab work (blood tests for testosterone, PSA and hematocrit), which are essential for safe monitoring.
Insurance coverage is highly variable. Most plans will cover TRT for a confirmed diagnosis of hypogonadism, but may require prior authorization or prefer certain formulations (e.g., generic injections) over more expensive options.
Are There Natural Ways to Boost Testosterone?
Before turning to medication, it’s always wise to address lifestyle factors.
For men with low-normal levels or those whose levels are low due to poor health habits, these strategies can make a meaningful difference and are recommended by physicians before considering TRT.
- Lose Excess Weight: Fat tissue, especially abdominal fat, contains the enzyme aromatase, which converts testosterone into estrogen. Losing weight is one of the most effective ways to naturally increase testosterone levels.
- Resistance Training: Lifting weights and other forms of strength training have been shown to provide a temporary and long-term boost to testosterone levels. Focus on compound movements like squats, deadlifts and presses.
- Get Enough Sleep: The majority of testosterone is produced during sleep. Consistently getting less than 7-8 hours of quality sleep per night can significantly lower your levels.
- Manage Stress: Chronic stress elevates cortisol, a hormone that has an inverse relationship with testosterone. When cortisol is high, testosterone tends to be low. Practices like meditation, yoga or mindfulness can help.
- Balanced Diet: Ensure you’re getting enough zinc, vitamin D, and healthy fats, all of which are important for testosterone production. Avoid excessive alcohol consumption, which can lower T levels.
While these methods can help optimize your natural production, they are unlikely to raise testosterone levels from clinically low (hypogonadal) to normal on their own.
They are best viewed as a foundational part of men’s health, whether you are on TRT or not.
Conclusion
Testosterone Replacement Therapy is a powerful medical tool, not an anti-aging miracle.
For men with a confirmed diagnosis of hypogonadism, TRT can dramatically improve quality of life by alleviating debilitating symptoms related to sexual function, energy, and mood.
The potential benefits are real and well-documented.
However, the decision to start TRT must be made with a full understanding of its significant risks and lifelong commitment.
The potential for cardiovascular issues, prostate stimulation, infertility, and other side effects requires diligent monitoring by a qualified healthcare provider.
The latest evidence from the TRAVERSE trial has eased some of the most severe fears about heart attacks but has also highlighted other risks like A-Fib and blood clots.
Ultimately, the choice is a personal one, made in close consultation with your doctor.
It involves weighing the severity of your symptoms against the potential harms of the therapy.
If you suspect you have low testosterone, the first step is not to seek out a “low T clinic”, but to have a comprehensive evaluation with your primary care physician or an endocrinologist to rule out other causes and confirm a diagnosis with proper testing.
What are your thoughts or experiences with TRT? Share your questions or comments below to help others in their journey.
Frequently Asked Questions (FAQ)
1. What is TRT?
TRT stands for Testosterone Replacement Therapy. It is a medical treatment prescribed to men with clinically diagnosed low testosterone (hypogonadism) to restore hormone levels to a normal range using injections, gels, patches, or other methods.
2. How do I know if I need TRT?
You may need TRT if you have persistent symptoms (like low libido, fatigue, erectile dysfunction) AND at least two separate early-morning blood tests confirm your total testosterone is below 300 ng/dL. A doctor must make the diagnosis.
3. How long does it take for TRT to work?
Some benefits, like improved libido, can be felt within a few weeks. Other changes, such as increased muscle mass and bone density, can take 3-6 months or longer to become noticeable. Full effects may take up to a year.
4. Can TRT make me infertile?
Yes. TRT suppresses the body’s natural hormone signals, leading to a drastic reduction or complete halt in sperm production. It is a common cause of male infertility and should be avoided if you plan on having children.
5. Does TRT cause prostate cancer?
Current evidence does not show that TRT causes new cases of prostate cancer. However, it can stimulate the growth of existing prostate cancer, which is why it is contraindicated for men with the active disease.
6. Is TRT safe for the heart?
The large TRAVERSE trial (2023) found TRT did not increase the risk of heart attack or stroke in at-risk men. However, it did show a higher incidence of atrial fibrillation and pulmonary embolism, so cardiovascular risks still exist.
7. What happens if I stop TRT?
When you stop TRT, your body’s natural testosterone production is suppressed. It can take several months for your system to recover, during which you may feel a significant worsening of low T symptoms. A restart protocol should be managed by a doctor.
8. What is the best type of TRT?
There is no single “best” type. The choice between injections, gels, or pellets depends on your lifestyle, cost, insurance, and personal preference. Injections are often cheapest, while gels offer stable levels and pellets offer convenience.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. The information contained herein is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay in seeking it because of something you have read in this article.
Reference
[1] Testosterone Deficiency Guideline – American Urological Association
https://www.auanet.org/guidelines-and-quality/guidelines/testosterone-deficiency-guideline
[2] Testosterone Treatment in Adult Men With Age-Related Low …
https://www.acpjournals.org/doi/10.7326/M19-0882
[3] Testosterone Therapy for Hypogonadism Guideline Resources
https://www.endocrine.org/clinical-practice-guidelines/testosterone-therapy
[4] Pharmacology of testosterone replacement therapy preparations
https://pmc.ncbi.nlm.nih.gov/articles/PMC5182226
[7] Cardiovascular Safety of Testosterone-Replacement Therapy
https://www.nejm.org/doi/full/10.1056/NEJMoa2215025
[8] Testosterone Treatment and Fractures in Men with Hypogonadism

