The primary signs of cataracts include increasingly blurry or cloudy vision, faded colors, significant glare from lights, and difficulty seeing at night.
A cataract is a progressive clouding of the eye’s natural lens, the part responsible for focusing light and producing clear, sharp images.
If you feel like you’re perpetually looking through a foggy window, you may be experiencing the onset of this common condition.
This isn’t a rare phenomenon. In fact, cataracts are a leading cause of vision loss worldwide and a natural consequence of aging for many.
The scale is staggering: according to the National Eye Institute (NEI), more than half of all Americans age 80 or older either have cataracts or have undergone surgery to correct them.
This underscores the importance of understanding this condition not as a rare disease, but as a common health consideration in later life.
In this comprehensive guide, we will move beyond the simple definition to provide a deep, evidence-based exploration of cataracts.
We will dissect the subtle early signs that are often dismissed, trace the progression of symptoms, and illuminate the underlying causes and risk factors.
You will learn about the different types of cataracts, how they are diagnosed, and what modern medicine offers for treatment.
Are you experiencing some of these changes in your vision? Keep reading to understand what they mean for your eye health and what you can do about it.
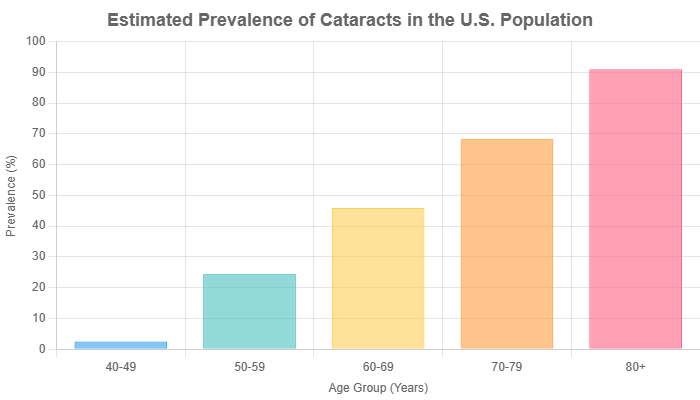
Data Source: Based on prevalence estimates from the National Eye Institute (NEI) and Centers for Disease Control and Prevention (CDC).
In This Article
What Exactly Are Cataracts? A Clear Explanation
To understand the symptoms, we must first understand the mechanism.
At its core, a cataract is a clouding of the natural lens inside your eye, which lies behind the iris and the pupil.
This lens, which is normally crystal clear, works much like the lens of a camera—it adjusts the eye’s focus, allowing us to see things clearly at varying distances.
The most effective analogy, cited by ophthalmologists and institutions like the Mayo Clinic, is that of looking through a foggy or frosted window.
Initially, the “fog” may only cover a small part of the lens, and you might not even notice a change in your vision.
But as the cataract grows larger and denser, it clouds more of the lens, making it increasingly difficult for light to pass through cleanly.
The Science of Clouding: A Breakdown of the Lens
The human lens is a marvel of biological engineering, composed primarily of water and highly organized proteins called crystallins.
These proteins are arranged in a precise structure that allows the lens to remain transparent and effectively refract light onto the retina at the back of the eye.
The retina then converts this light into nerve signals that are sent to the brain, which interprets them as images.
With age, and accelerated by certain risk factors, the delicate structure of these proteins can begin to break down and denature.
They start to clump together, forming opaque or cloudy areas within the lens.
This clumping is the physical manifestation of a cataract.
As these protein aggregates grow, they scatter and block the light passing through the lens, preventing a sharply defined image from reaching the retina.
The result is the hallmark symptom of cataracts: blurred vision.
This process is typically slow and painless, which is why many people don’t realize their vision is deteriorating until it begins to significantly impact their daily lives.
What Are the Telltale Signs and Symptoms of Cataracts?
The symptoms of cataracts develop gradually and can vary depending on the type and density of the cataract.
What begins as a minor annoyance can evolve into a significant visual impairment.
Recognizing these signs early is the first step toward managing the condition effectively.
Blurry, Cloudy, or Dim Vision
This is the most universally reported symptom of cataracts.
Vision may seem generally out of focus, as if you’re looking through a piece of filmy glass.
This blurriness is constant and cannot be corrected by blinking or cleaning your glasses.
Experiential Insight: Many people initially attribute this symptom to their glasses being dirty or their prescription needing a minor update. A common complaint found on patient forums is the frustration of constantly wiping spectacles, only to find the “smudge” is in their vision itself. It can make it difficult to recognize faces across a room or read street signs, creating a sense of detachment from the world.
The scientific reason for this blur is the scattering of light by the aggregated proteins in the lens. Instead of focusing light into a single, sharp point on the retina, the cataract scatters it in multiple directions, creating a hazy and unfocused image.
Increasing Difficulty with Night Vision
A significant and often alarming symptom is a marked decline in the ability to see in low-light conditions.
Activities that were once routine, such as walking in a dimly lit room or driving at night, become challenging and potentially dangerous.
Experiential Insight: Night driving is a frequent topic of concern for those developing cataracts. As one user on a Reddit forum described, “Oncoming headlights, which were once just bright, now seem to explode into blinding starbursts. It feels like every light source has a halo, making it impossible to judge distance or see the road clearly”. This experience can lead to a loss of confidence and independence.
This phenomenon occurs because in low light, the pupil dilates (widens) to let in more light.
This exposes more of the clouded lens, maximizing the light-scattering effect of the cataract.
The high contrast between bright headlights and a dark road exacerbates this effect, leading to severe glare and halos.
Sensitivity to Light and Glare
Known clinically as photophobia, this symptom makes normal levels of light seem overwhelmingly bright and painful.
Bright sunlight or even intense indoor lighting can cause squinting and discomfort.
This sensitivity is another direct result of light scattering.
The cataract breaks up incoming light rays, causing them to spread across the retina in an uncontrolled manner instead of being focused properly.
This stray light creates the sensation of glare and can make it difficult to see in bright conditions.
You might find yourself reaching for sunglasses more often, even on overcast days.
Seeing “Halos” or Starbursts Around Lights
While related to glare, this symptom is more specific. It involves seeing distinct rings (halos) or star-like patterns around light sources, especially at night.
This is a classic sign of certain types of cataracts, particularly posterior subcapsular cataracts.
This visual distortion is caused by the diffraction of light as it passes through the opaque parts of the lens.
The tiny, clumped proteins act like a flawed prism, splitting the light into a spectrum or pattern that is perceived as a halo.
Fading or Yellowing of Colors
As a cataract matures, it can take on a yellowish or brownish hue.
This acts like a filter, altering color perception and making the world appear less vibrant.
Whites may look creamy or yellow, and it can become difficult to distinguish between similar colors like blue and purple.
Experiential Insight: This symptom is often subtle and progresses so slowly that individuals may not notice it until after they have cataract surgery on one eye. Post-surgery, patients are frequently astonished by the true vibrancy of colors, realizing they had been living in a “sepia-toned” world. Artists, photographers, and designers may notice this change earlier due to their trained eye for color accuracy.
This color shift is most common with nuclear sclerotic cataracts, where the central part of the lens hardens and yellows over time, absorbing blue light wavelengths.
Frequent Changes in Eyeglass or Contact Lens Prescription
If you find that your vision prescription is becoming unstable and you need frequent updates to your glasses or contacts, it could be a sign of developing cataracts.
As the cataract alters the shape and refractive index of the lens, your vision can fluctuate.
The “Second Sight” Phenomenon
In some cases, particularly with nuclear cataracts, the lens may swell slightly and increase its focusing power.
This can temporarily improve a person’s near vision, an effect sometimes called “second sight”.
An individual who has needed reading glasses for years might suddenly find they can read small print without them.
However, this improvement is fleeting.
As the cataract progresses, this temporary benefit disappears, and overall vision deteriorates.
Double Vision (Diplopia) in a Single Eye
Cataracts can cause monocular diplopia, which is the perception of two images when looking with only one eye.
This is different from the more common binocular diplopia, which is caused by eye misalignment and disappears when one eye is covered.
This occurs because the cataract can split the light beam into two separate paths as it enters the eye, creating two distinct (though often overlapping) images on the retina.
This symptom often resolves as the cataract becomes denser and obscures one of the light paths.
What Are the Different Types of Cataracts?
Not all cataracts are the same. They are classified based on their location within the lens.
The type of cataract influences the specific symptoms you experience and how quickly they progress.
Understanding the type can help you and your doctor anticipate how your vision might change over time.
Nuclear Sclerotic Cataracts
This is the most common type of age-related cataract. It forms deep in the central zone (nucleus) of the lens. Its primary characteristic is the gradual hardening and yellowing of the lens, a process called sclerosis.
This type progresses slowly over many years and primarily affects distance vision more than near vision initially.
The yellowing of the lens is what leads to the dulling of colors and is also responsible for the temporary “second sight” phenomenon.
Cortical Cataracts
A cortical cataract begins as whitish, wedge-shaped opacities or streaks on the outer edge of the lens cortex.
As it progresses, the streaks extend toward the center and interfere with light passing through the lens.
The primary symptom associated with cortical cataracts is significant glare, making night driving and seeing in bright sunlight particularly difficult.
Individuals with diabetes have a higher risk of developing cortical cataracts.
Posterior Subcapsular Cataracts
This type begins as a small, opaque area on the back (posterior) surface of the lens, directly in the path of light.
Posterior subcapsular cataracts (PSCs) tend to progress much faster than other types, with vision loss occurring over months rather than years.
They disproportionately affect reading vision and cause significant glare and halos around lights.
PSCs are more common in younger people and those who have taken high doses of steroid medications, have diabetes, or have extreme nearsightedness.
Congenital Cataracts
Some people are born with cataracts, or they develop during childhood.
These are known as congenital cataracts.
They can be genetic or associated with an infection or trauma during pregnancy (e.g., rubella).
They can also be linked to certain syndromes like myotonic dystrophy.
Not all congenital cataracts affect vision, but if they do, they are typically removed soon after detection to allow for normal visual development.
Comparative Overview of Cataract Types
To help summarize these distinctions, the following table provides a clear comparison of the main cataract types.
| Type of Cataract | Location in Lens | Primary Symptoms | Commonly Affects |
|---|---|---|---|
| Nuclear Sclerotic | Center (Nucleus) | Blurry distance vision, faded/yellowed colors, “second sight” | Older adults as a natural part of aging |
| Cortical | Edge (Cortex) | Significant glare, light sensitivity, wedge-shaped opacities | Individuals with diabetes |
| Posterior Subcapsular | Back Surface (Posterior Capsule) | Rapid vision loss, severe glare/halos, difficulty reading | Younger individuals, steroid users, diabetics |
| Congenital | Varies (Present at Birth) | Can be asymptomatic or cause significant blur, nystagmus | Infants and children (genetic or due to other conditions) |
What Causes Cataracts and Who Is at Risk?
While the exact mechanism of protein clumping is still under intense study, researchers have identified a primary cause and a host of contributing risk factors.
The single greatest risk factor for developing cataracts is simply getting older.
However, lifestyle and other medical conditions can significantly influence when and how quickly they develop.
A 2024 study published in Frontiers in Public Health highlighted that while the age-standardized incidence of cataracts is decreasing globally due to better health, the absolute number of cases is rising due to an aging population.
The study also reinforced the role of modifiable risk factors.
Here are the key risk factors that increase your likelihood of developing cataracts:
- Increasing Age: The proteins in the lens change over a lifetime, making age the most significant and unavoidable risk factor.
- Diabetes: People with diabetes are at a much higher risk. High blood sugar (hyperglycemia) can cause the lens to swell and can lead to the accumulation of sorbitol in the lens, which contributes to protein aggregation and cataract formation.
- Excessive Sunlight Exposure: Long-term, unprotected exposure to ultraviolet (UV) radiation from the sun is a well-established cause. UV light generates free radicals that damage the lens proteins. The World Health Organization (WHO) identifies cataracts as a major consequence of UV exposure.
- Smoking: Smoking doubles the risk of developing cataracts. The toxins in cigarette smoke are absorbed into the bloodstream and can cause oxidative stress throughout the body, including in the lens.
- Obesity: A high body mass index (BMI) is associated with an increased risk of cataracts, likely due to increased oxidative stress and inflammation.
- High Blood Pressure (Hypertension): Some studies suggest a link between hypertension and an increased risk of certain types of cataracts.
- Previous Eye Injury or Inflammation: Trauma to the eye can disrupt the lens structure and lead to a “traumatic cataract”, which can form immediately or years after the injury. Chronic inflammation (uveitis) can also contribute.
- Previous Eye Surgery: Prior ocular surgeries, such as a vitrectomy for retinal issues, can accelerate cataract formation.
- Prolonged Use of Corticosteroid Medications: Long-term use of steroids, whether taken orally, through an inhaler, or as eye drops, is a major risk factor for developing posterior subcapsular cataracts.
- Drinking Excessive Amounts of Alcohol: Heavy alcohol consumption has been linked to an increased risk of cataract formation.
- Family History: A genetic predisposition can play a role in how early you develop cataracts.
- Poor Nutrition: A diet lacking in antioxidants may increase risk. A large population study cited by the American Academy of Ophthalmology (AAO) suggests that a diet rich in vitamins and minerals from fruits and vegetables is associated with a reduced risk.
- Air Pollution: Emerging research, such as the 2024 study in Frontiers in Public Health, suggests that environmental factors like particulate matter pollution may also contribute to cataract development.
How Are Cataracts Diagnosed?
Diagnosing cataracts is a straightforward process performed by an ophthalmologist or optometrist during a comprehensive eye examination.
If you suspect you have cataracts based on your symptoms, a professional evaluation is the only way to get a definitive answer.
The exam is painless and involves several key tests.
Visual Acuity Test
This is the most basic and familiar eye test.
You will be asked to read letters from an eye chart (a Snellen chart) at various distances.
This test measures the clarity and sharpness of your vision. Your vision will be recorded as a fraction, such as 20/20 or 20/40.
A score of 20/40 means you must be 20 feet away to see what a person with normal vision can see from 40 feet away.
This test helps quantify the degree of vision loss.
Slit-Lamp Examination
This is the gold standard for diagnosing cataracts.
A slit lamp is a high-magnification binocular microscope with a bright, narrow beam of light (the “slit”).
It allows your eye doctor to examine the structures at the front of your eye—the cornea, iris, and lens—in minute, three-dimensional detail.
By looking through the slit lamp, the doctor can identify the exact location, size, and density of any opacities in your lens, confirming the presence of a cataract and determining its type.
Retinal Exam (Pupil Dilation)
To get a better view of the back of your eye, your doctor will likely dilate your pupils.
This involves administering special eye drops that cause the pupils to widen significantly.
After waiting 15-30 minutes for the drops to take effect, the doctor can look through the enlarged pupil to thoroughly examine the retina and the optic nerve. This is crucial for two reasons:
- It allows for a clearer view of the entire lens, especially the posterior part, helping to assess the full extent of the cataract.
- It enables the doctor to rule out other eye diseases that could be causing your vision symptoms, such as macular degeneration or diabetic retinopathy.
After dilation, your eyes will be very sensitive to light, and your near vision will be blurry for several hours.
It is essential to bring sunglasses to your appointment and arrange for someone to drive you home.
When Is It Time for Cataract Surgery?
Once diagnosed, the path to treatment depends entirely on how much the cataracts are affecting your vision and your life.
There is no medication, eye drop, or exercise that can reverse or “cure” cataracts.
The only definitive treatment is surgery.
Early-Stage Management
In the early stages, when symptoms are mild, surgery is usually not necessary.
Vision can often be improved with simple, non-invasive measures:
- Updating Your Prescription: A new prescription for eyeglasses or contact lenses can often sharpen vision temporarily.
- Using Brighter Lighting: Increasing the ambient light for reading and other close-up tasks can make a significant difference.
- Anti-Glare Sunglasses: Wearing sunglasses that have an anti-reflective coating can help reduce glare during the day.
- Magnifying Lenses: For reading and hobbies, a magnifying glass can be a useful aid.
The Deciding Factor: Quality of Life
The decision to proceed with cataract surgery is not based on a specific vision score or the “ripeness” of the cataract—an outdated concept.
Instead, the primary consideration is your quality of life.
Your ophthalmologist will recommend surgery when your cataracts begin to interfere with your ability to perform essential and enjoyable daily activities.
The key question to ask yourself is: “Is my vision preventing me from doing the things I need or want to do?”
This could include difficulty with:
- Driving safely, especially at night.
- Reading books, newspapers, or screens.
- Working or performing your job effectively.
- Enjoying hobbies like sewing, painting, or playing cards.
- Recognizing faces or seeing expressions clearly.
- Navigating your home safely and avoiding falls.
What is Cataract Surgery?
Cataract surgery is one of the most common, safest, and most effective surgical procedures performed today.
The procedure involves removing the clouded natural lens and replacing it with a clear, artificial lens called an intraocular lens (IOL).
The surgery is typically performed on an outpatient basis and takes less than 30 minutes.
The success rate is exceptionally high.
According to the Cleveland Clinic, the vast majority of patients experience significantly improved vision after the procedure, with studies showing success rates well over 98%.
While all surgery carries some risk, serious complications from cataract surgery are rare.
Can You Prevent or Slow Down Cataracts?
While there is no scientifically proven way to completely prevent age-related cataracts, compelling evidence suggests that certain lifestyle choices and preventive measures can help reduce your risk and potentially slow their progression.
These strategies focus on minimizing oxidative stress and protecting the eyes from environmental damage.
A 2024 review in the journal Frontiers in Nutrition analyzed the correlation between diet and cataracts, concluding that balanced diets rich in antioxidants are protective.
Here are evidence-based strategies to protect your eye health:
- Protect Your Eyes from UV Light: This is one of the most effective preventive steps. Always wear sunglasses that block 100% of UVA and UVB rays when you are outdoors. A wide-brimmed hat provides additional protection.
- Quit Smoking: If you smoke, stopping is one of the best things you can do for your overall health and your eyes. Quitting can help slow the progression of cataracts.
- Manage Other Health Problems: Diligently follow your treatment plan for conditions like diabetes and hypertension. Keeping blood sugar and blood pressure under control is crucial for protecting the delicate blood vessels and structures in your eyes.
- Eat a Diet Rich in Antioxidants: While antioxidant pills have not been definitively proven to prevent cataracts, a diet rich in natural sources of these nutrients is beneficial. Focus on consuming fruits and vegetables high in:
- Vitamin C: Found in citrus fruits, bell peppers, broccoli, and strawberries.
- Lutein and Zeaxanthin: Found in leafy green vegetables like spinach and kale, as well as eggs. These carotenoids are known to accumulate in the lens and retina, where they help filter harmful blue light. A study published in PubMed Central confirms that intake of these minerals is associated with a reduced risk.
Reduce Alcohol Consumption: Limiting your intake of alcohol can lower your risk of developing cataracts.
Get Regular Eye Exams: Routine examinations (every 1-2 years, especially after age 50) allow your eye doctor to detect cataracts and other eye problems at their earliest stages, providing more options for management and treatment.
Frequently Asked Questions (FAQ)
1. Are cataracts painful?
No, cataracts themselves are not painful. They do not cause eye pain, redness, or irritation. The vision changes they cause are gradual and painless. If you experience eye pain, you should see a doctor immediately as it may be a sign of another serious condition.
2. Can cataracts be reversed without surgery?
Currently, there is no non-surgical cure for cataracts. No eye drops, medications, or dietary supplements have been proven to reverse or dissolve existing cataracts. Surgery to replace the clouded lens is the only effective treatment to restore clear vision.
3. How long does it take for a cataract to become “ripe”?
The concept of a cataract needing to be “ripe” is outdated. Modern surgery allows for removal at any stage. Progression varies greatly, some cataracts develop slowly over decades, while others (like posterior subcapsular) can cause significant vision loss in months.
4. Am I too young to get cataracts?
While most common in people over 60, cataracts can occur at any age. Younger individuals may develop them due to genetics, eye injuries, certain medical conditions like diabetes, or prolonged use of steroid medications. Congenital cataracts are present at birth.
5. What happens if I wait too long to have cataract surgery?
Waiting too long can make the cataract very dense and hard, which can make the surgery slightly more complex. More importantly, it means living with poor vision, which increases the risk of falls and injuries and can lead to a loss of independence and depression.
6. Can cataracts cause total blindness?
Yes, if left untreated, cataracts can progress to the point of causing legal or even total blindness. However, this blindness is reversible. Cataract surgery can restore vision even in very advanced cases, making it a leading cause of preventable blindness worldwide.
7. Does cataract surgery hurt?
No, the procedure itself is painless. Your eye will be completely numbed with anesthetic eye drops or an injection. You may feel slight pressure during the surgery, but you should not feel pain. Mild discomfort or a scratchy sensation is common for a day or two after.
8. Will my vision be perfect after cataract surgery?
Most people experience a dramatic improvement in their vision. The type of intraocular lens (IOL) you choose will determine your need for glasses afterward. While standard IOLs correct distance vision well, you will likely still need reading glasses. Premium IOLs can reduce or eliminate the need for glasses.
9. Can cataracts grow back after surgery?
No, a cataract cannot grow back because the natural lens has been removed. However, a common condition called posterior capsule opacification (PCO) can occur months or years later. The capsule that holds the IOL becomes cloudy, mimicking cataract symptoms. This is easily and painlessly corrected with a quick laser procedure.
Conclusion
The journey from noticing the first subtle signs of blurry vision to understanding a diagnosis of cataracts can be filled with uncertainty.
However, as we have explored, this condition is not a sentence for a life of poor vision.
It is a common, well-understood part of the aging process, and its symptoms, while progressive, are highly manageable.
The key takeaways are clear: recognizing the telltale signs—from the classic foggy vision and night-driving glare to the more subtle fading of colors—is the first and most crucial step.
Understanding that modern cataract surgery is an exceptionally safe and effective procedure can transform anxiety into empowerment.
The decision to act is based not on fear, but on a desire to reclaim the quality of life that clear vision affords.
A cataract diagnosis is simply a signpost, directing you toward a solution that has restored sight to millions.
The future of your vision can be bright and clear.
If you recognize any of the symptoms discussed in this article in your own vision, do not dismiss them or wait for them to worsen. Schedule a comprehensive eye exam with an ophthalmologist or optometrist. A clear diagnosis is the first step to creating a clear plan for your future.
Have you experienced any of these signs? Share your story or ask a question in the comments below to help others in the community navigate their own journey.
Reference
[1] Five Signs You May Have Cataracts | Cedars-Sinai
https://www.cedars-sinai.org/blog/five-signs-you-may-have-cataracts.html
[2] Understanding the Initial Sign of Cataracts – Visionary Eye Doctors
https://www.voeyedr.com/blog/understanding-the-initial-sign-of-cataracts/
[3] Spot the early signs of cataracts: symptoms to watch
https://practiceplusgroup.com/knowledge-hub/spot-first-signs-of-cataracts
[4] Global, regional, and national burden of cataract: A comprehensive …
https://pmc.ncbi.nlm.nih.gov/articles/PMC12185006
[5] Cataracts: Signs, Symptoms & Treatment – Cleveland Clinic
https://my.clevelandclinic.org/health/diseases/8589-cataracts-age-related
[6] Cataracts 101: Early Signs, Surgery Timing & Best Eye Hospital
https://www.hillcountryeye.com/cataracts-101-early-signs-and-when-to-consider-surgery
[7] Can a bad cataract cause blurriness to where you can’t even make …
[8] Discomfort due to a cataract? : r/CataractSurgery – Reddit
https://www.reddit.com/r/CataractSurgery/comments/14js4tc/discomfort_due_to_a_cataract/

