The earliest signs of prostate cancer are often no signs at all. This silent nature is the disease’s most deceptive trait.
While many men wait for a clear warning, early-stage prostate cancer frequently develops without causing any noticeable symptoms.
However, certain subtle changes, particularly in urinary habits, can be the first clues that warrant a crucial conversation with your doctor.
This isn’t a rare disease affecting a small fraction of the population. It is the second most common cancer among American men, trailing only skin cancer.
The American Cancer Society estimates that in 2025 alone, there will be over 313,000 new cases of prostate cancer diagnosed and nearly 36,000 deaths.
This staggering statistic underscores the critical importance of awareness and proactive health management.
This article is designed to be your definitive guide. We will move beyond simple lists of symptoms to provide the context you need.
You will learn to recognize potential warning signs, understand the crucial difference between common aging issues like Benign Prostatic Hyperplasia (BPH) and potential cancer symptoms, identify your personal risk factors, and navigate the landscape of modern screening and detection.
Gaining this knowledge is the first and most powerful step you can take to be proactive about your long-term prostate health.
In This Article
The Core Challenge: Why Early Prostate Cancer is Often Asymptomatic
One of the most common and dangerous misconceptions about prostate cancer is the belief that you will “feel” something wrong if you have it.
This expectation leads many men to delay screening, believing that the absence of symptoms equals the absence of disease.
Unfortunately, this is a flawed and risky strategy.
Understanding the “why” behind its silent nature is key to shifting from a reactive to a proactive mindset.
Anatomical Location and Tumor Growth
The prostate is a small, walnut-shaped gland that is part of the male reproductive system.
Its primary function is to produce seminal fluid.
Crucially, it is located just below the bladder and surrounds the urethra—the tube that carries urine out of the body.
You might assume that any growth in this gland would immediately squeeze the urethra and cause problems, but the specific location of most early tumors is the reason this doesn’t happen.
The prostate is comprised of several zones.
According to research published in journals like Radiographics, approximately 70-80% of prostate cancers originate in the peripheral zone.
This is the outer region of the gland, furthest away from the urethra. In the early stages, a tumor can grow quite significantly in this area without pressing on the urethra or causing any urinary obstruction.
The symptoms many men associate with prostate issues—like a weak stream or frequent urination—only tend to appear when the tumor grows large enough to invade the central parts of the gland or when the disease is more advanced.
The Slow-Growing Nature of Most Prostate Cancers
Another critical factor is the growth rate.
Many prostate cancers are described as indolent, meaning they grow very slowly over many years, or even decades.
A small, slow-growing tumor in the peripheral zone may never become large enough to cause symptoms or pose a threat to a man’s life.
This is the basis for “active surveillance,” a common management strategy for low-risk prostate cancer where the disease is monitored closely rather than treated immediately.
However, other prostate cancers are aggressive, growing and spreading much more quickly.
Without screening, it’s impossible to know which type a man might have.
Waiting for symptoms to appear means you may be giving an aggressive cancer a significant head start.
The “Silent” Disease Analogy: Think of early prostate cancer like a small, slow leak in a pipe behind a wall. You won’t see any water damage on the surface until the leak has been active for a long time and has caused significant, potentially structural, problems. Proactive screening is like using a moisture meter to check behind the wall, allowing you to find and fix the leak before it ever becomes a visible crisis. This is why organizations like the Prostate Cancer Foundation emphasize that proactive screening, not symptom-watching, is the cornerstone of modern prostate health.
Decoding the Warning Signs: When to Pay Attention
While early-stage prostate cancer is often asymptomatic, as a tumor grows, it can begin to exert pressure on the urethra and bladder neck.
This can lead to a cluster of symptoms known as Lower Urinary Tract Symptoms (LUTS). It is critically important to understand that these symptoms are far more commonly caused by a non-cancerous condition called Benign Prostatic Hyperplasia (BPH), or simply an enlarged prostate.
However, because the symptoms can overlap, they should never be ignored or self-diagnosed.
They are your body’s signal to schedule a medical evaluation.
A Frequent or Urgent Need to Urinate, Especially at Night (Nocturia)
What It Feels Like
This isn’t just about needing to go to the bathroom a bit more often.
It’s a noticeable shift in your daily and nightly routine. You might find yourself constantly planning your day around bathroom availability.
The urgency can be sudden and overwhelming, making you feel like you might not make it in time.
The most disruptive aspect for many men is nocturia—the need to wake up to urinate.
Reality Check & When to See a Doctor
Waking up once during the night to urinate can be a normal part of aging.
However, if you consistently find yourself waking up two, three, or more times per night, it’s a significant change that is disrupting your sleep and warrants a discussion with your doctor.
This persistent interruption of sleep can lead to daytime fatigue, irritability, and a reduced quality of life, regardless of the underlying cause.
A Weak, Slow, or Interrupted Urine Stream
What It Feels Like
You might notice that it takes significantly longer to empty your bladder than it used to.
The stream itself may be weak, lacking the force it once had.
A common description from men in health forums is the feeling that the stream “starts and stops”; on its own, requiring them to wait for it to resume.
Many also report having to push or strain to initiate or maintain urination.
Experiential Insight & When to See a Doctor
This symptom can be a source of significant frustration and even public anxiety.
Using a urinal next to others can become an uncomfortable experience.
If you notice a consistent and progressive weakening of your urinary stream, or if you find yourself needing to strain to urinate, it’s a clear signal that there is some form of obstruction that needs to be professionally evaluated.
Difficulty Starting or Stopping Urination (Hesitancy)
What It Feels Like
Hesitancy is the experience of standing at the toilet, ready to urinate, but nothing happens for several seconds or even longer.
It feels as though the signal from your brain isn’t connecting properly.
The opposite end of this is post-urination dribbling, where you feel you’ve finished and shaken off, but urine continues to leak out afterwards, often staining underwear.
This happens because the bladder isn’t able to empty completely and forcefully.
When to See a Doctor
Occasional, momentary hesitancy can happen to anyone.
But if this becomes a regular pattern, or if post-urination dribbling is a persistent issue, it points to a potential problem with the prostate or bladder function that should be investigated by a doctor.
A Feeling That Your Bladder Hasn’t Fully Emptied
What It Feels Like
This is a persistent, nagging sensation.
You’ve just left the bathroom, but you feel like you could go again.
It’s a feeling of incomplete relief.
This happens because an enlarged prostate can prevent the bladder from contracting effectively to expel all the urine, leaving a residual amount behind.
This residual urine can also increase the risk of urinary tract infections (UTIs).
When to See a Doctor
If you consistently feel the need to urinate again within minutes of having just gone, this is a classic sign of incomplete bladder emptying.
It’s a significant symptom that should prompt a visit to your primary care physician or a urologist.
Are There Other, Less Common Signs of Prostate Cancer?
The following signs are less common, particularly for early, localized prostate cancer.
However, they are significant red flags that require immediate medical evaluation as they can sometimes indicate a more advanced or aggressive disease.
Blood in the Urine (Hematuria) or Semen (Hematospermia)
Seeing blood in your urine or semen can be alarming, and for good reason. While it can be caused by other issues like a vigorous infection, kidney stones, or trauma, it can also be a sign of cancer in the prostate, bladder, or kidneys.
Actionable Advice: There is no “normal” amount of blood in the urine or semen. Any instance, even if it’s just a pinkish tinge and it only happens once, should be considered a medical priority. Do not wait to see if it happens again. Schedule an appointment with a urologist immediately. According to the Mayo Clinic, this symptom warrants a thorough investigation.
New Onset of Erectile Dysfunction (ED)
Erectile dysfunction is an extremely common condition with a multitude of causes, including stress, cardiovascular disease, diabetes, and psychological factors. It is not, by itself, a primary indicator of prostate cancer.
However, the nerves that control erections are located very close to the prostate gland.
A tumor that is growing and pressing on these nerves could potentially interfere with their function.
Nuance is Key: The important factor here is context. A sudden change in erectile function, especially if it occurs alongside any of the urinary symptoms discussed above, is something that should be brought to your doctor’;s attention. It adds another piece to the puzzle that your doctor can use in their evaluation.
Pain or Discomfort in the Pelvic Area, Lower Back, Hips, or Chest
This is perhaps the most critical distinction to make in this entire article.
While pelvic discomfort can occasionally occur with a very large prostate or severe inflammation, persistent pain in the bones of the lower back, hips, pelvis, or ribs is not an early sign of prostate cancer.
Crucial Distinction: This type of bone pain is a classic symptom of advanced or metastatic prostate cancer—cancer that has escaped the prostate gland and spread to other parts of the body, most commonly the bones. The presence of this symptom indicates that the window for catching the disease at its earliest, most curable stage has likely passed. This highlights the profound danger of ignoring the earlier, more subtle urinary symptoms and waiting for a more “obvious” sign like pain to appear.
BPH vs. Prostate Cancer: A Critical Comparison
As you experience urinary changes, the most pressing question becomes: “Is this just a normal part of aging, or is it cancer?”.
This is the central point of confusion and anxiety for millions of men.
The vast majority of the time, these symptoms are caused by Benign Prostatic Hyperplasia (BPH).
But because the symptoms can be indistinguishable, a professional diagnosis is essential.
The Impossible Task of Self-Diagnosis
Let’s be unequivocally clear: the urinary symptoms of BPH and prostate cancer can be absolutely identical.
A man with a severely enlarged but non-cancerous prostate can have a very weak stream and wake up five times a night.
A man with early-stage prostate cancer might have the exact same symptoms, or none at all.
It is physically impossible for you to differentiate between the two based on how you feel.
This overlap is precisely why medical screening tools were developed.
The following table breaks down the key differences between these two distinct conditions.
This is designed to provide clarity, not to be a diagnostic tool.
| Feature | Benign Prostatic Hyperplasia (BPH) | Prostate Cancer |
|---|---|---|
| Nature | A non-cancerous, benign enlargement of the prostate gland, primarily in the transition zone surrounding the urethra. | A malignant (cancerous) tumor growth within the prostate, most often starting in the peripheral zone. |
| Common Symptoms | The primary cause of urinary symptoms: weak stream, frequency, urgency, nocturia, straining, incomplete emptying. | Often no symptoms in early stages. If symptoms are present, they can be identical to BPH’s urinary symptoms. |
| Progression | Symptoms may worsen over time as the gland continues to grow, further obstructing the urethra. | Can be slow-growing (indolent) or aggressive. If aggressive and untreated, it can spread (metastasize). |
| Key Differentiator | BPH is a benign condition. It does not spread to other parts of the body and is not life-threatening, though it can severely impact quality of life. | Prostate cancer is malignant. If it breaks out of the prostate capsule, it can spread to lymph nodes, bones, and other organs, becoming life-threatening. |
| Diagnosis | Diagnosis is based on symptom assessment, a digital rectal exam (DRE), and tests to rule out cancer. Treatment focuses on managing symptoms. | Requires a combination of a PSA blood test, DRE, and often an MRI. A definitive diagnosis can only be made with a prostate biopsy. |
The Bottom Line: Your symptoms tell your doctor that something is happening with your prostate. They are the starting signal for an investigation. They do not, however, provide the answer. The only way to know the true cause of your symptoms is to engage with the diagnostic process, which begins with a simple conversation with your doctor.
Proactive Health: Understanding Your Risk and Screening Options
Given that waiting for symptoms is an unreliable strategy, the focus must shift to proactive health management.
This involves two key components: understanding your personal risk profile and engaging in an informed discussion with your doctor about modern screening options.
This knowledge empowers you to take control of your health long before a problem becomes advanced.
Who Is at the Highest Risk for Developing Prostate Cancer?
While any man can develop prostate cancer, certain factors dramatically increase the likelihood.
Recognizing if you fall into a high-risk category is crucial for deciding when to start the screening conversation with your doctor.
Age: The Single Biggest Risk Factor
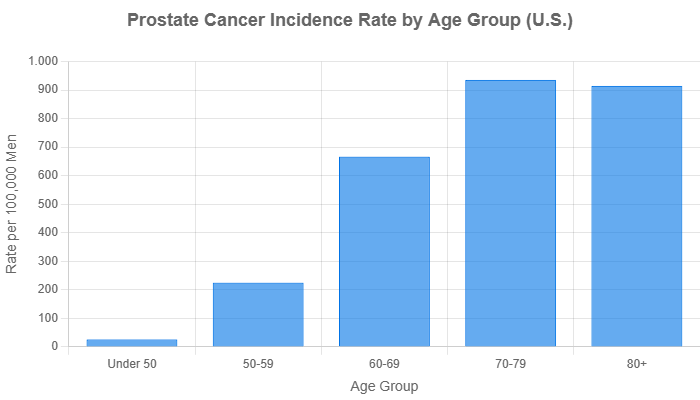
Age is the most significant, non-negotiable risk factor.
Prostate cancer is rare in men under 40. The risk begins to rise sharply after age 50 and continues to increase from there. According to the National Cancer Institute’s SEER Program, the average age at diagnosis is 67.
This data is why most screening guidelines focus on men in the 50-70 age range.
Race & Ethnicity: A Critical Health Disparity
For reasons that are still being intensely researched but likely involve a combination of genetic and environmental factors, Black men face a significantly higher risk of prostate cancer.
According to the Centers for Disease Control and Prevention (CDC), Black men are about 70% more likely to be diagnosed with prostate cancer and are more than twice as likely to die from the disease compared to white men.
They are also more likely to be diagnosed at a younger age and with a more aggressive form of the cancer.
This stark health disparity is why many organizations recommend that Black men begin the conversation about screening with their doctors earlier, typically starting at age 40 or 45.
Family History & Genetics: When Cancer Runs in the Family
Genetics play a powerful role. Your risk is significantly increased if you have a close relative (father, brother, or son) who was diagnosed with prostate cancer, especially if they were diagnosed at a young age (under 65).
Having multiple first-degree relatives with the disease increases your risk even more.
Furthermore, a family history of other cancers can be relevant. Inherited mutations in genes like BRCA1 and BRCA2, which are well-known for increasing breast and ovarian cancer risk in women, also substantially increase the risk of aggressive prostate cancer in men.
As detailed by the National Cancer Institute, a family history of breast, ovarian, pancreatic, or colon cancer can be a red flag. It’s vital to share your entire family health history with your doctor.
How Does Modern Prostate Cancer Screening Actually Work?
Prostate cancer screening has evolved significantly. It’s no longer a simple “yes or no” test but a nuanced process focused on “shared decision-making”.
This approach, championed by the U.S. Preventive Services Task Force (USPSTF) for men aged 55 to 69, means you and your doctor discuss the potential benefits (early detection of a lethal cancer) and harms (overdiagnosis and overtreatment of a harmless cancer) of screening to make a choice that aligns with your personal values and risk factors.
The PSA (Prostate-Specific Antigen) Blood Test Explained
The PSA test is the foundational tool of screening. It’s a simple blood test that measures the level of prostate-specific antigen, a protein produced by both normal and cancerous cells in the prostate. It’s crucial to understand what it is and what it isn’t:
- It is an indicator, not a cancer test. An elevated PSA level simply means something is happening with the prostate that is causing more of this protein to leak into the bloodstream. This could be cancer, but it is also commonly caused by BPH, a prostate infection (prostatitis), or even recent sexual activity or a long bike ride.
- There is no single “normal” number. While a level under 4.0 ng/mL was once considered normal, doctors now look at the value in context. A PSA of 3.5 might be more concerning in a 45-year-old than a 70-year-old. Doctors also look at the PSA velocity (how fast the level is rising over time) and PSA density (the PSA level relative to the size of the prostate) to make a more informed judgment.
The Digital Rectal Exam (DRE)
During a DRE, a doctor inserts a gloved, lubricated finger into the rectum to feel the surface of the prostate gland.
They are checking for any hard spots, lumps, or other abnormalities.
While the PSA test measures a chemical signal, the DRE provides a physical assessment.
Sometimes, a cancer can be felt with a DRE even when the PSA level is low.
The two tests are complementary.
The New Gold Standard? The Role of Prostate MRI
Perhaps the biggest advancement in prostate cancer diagnosis in the last decade is the widespread use of multi-parametric MRI (mpMRI).
In the past, an elevated PSA often led directly to a biopsy. Today, the modern approach is to use an mpMRI before a biopsy.
An mpMRI provides a detailed picture of the prostate, allowing radiologists to identify and grade suspicious areas. Its benefits are transformative:
- Avoiding Unnecessary Biopsies: If the MRI is clear, it can provide significant reassurance that an elevated PSA is likely due to a benign condition like BPH, allowing many men to safely avoid an invasive biopsy. A 2024 study in The New England Journal of Medicine highlighted how using MRI before biopsy significantly reduces the diagnosis of clinically insignificant cancers.
- Targeted Biopsies: If the MRI does show a suspicious lesion, it acts like a roadmap. During the subsequent biopsy, the urologist can use the MRI images (a technique called “fusion biopsy”) to precisely target the suspicious area, dramatically increasing the accuracy of the procedure and ensuring the most aggressive part of the tumor is sampled.
Frequently Asked Questions (FAQ)
1. What is the very first sign of prostate cancer?
Most often, there is no first sign. Early-stage prostate cancer is typically asymptomatic. When symptoms do occur, they are usually urinary changes like increased frequency or a weak stream, which are more commonly caused by non-cancerous BPH.
2. At what age should I start worrying about prostate cancer?
Instead of worrying, focus on awareness. Most guidelines suggest starting a screening conversation with your doctor at age 50 for average-risk men, age 45 for high-risk men (Black men, men with a first-degree relative with prostate cancer), and age 40 for those with multiple high-risk factors.
3. Can you have prostate cancer with a normal PSA level?
Yes, although it’s less common. Some aggressive forms of prostate cancer produce very little PSA. This is one reason why the digital rectal exam (DRE) remains a valuable part of the evaluation, as a tumor might be felt even with a low PSA.
4. Does frequent urination always mean a prostate problem?
No. While it’s a classic sign of an enlarged prostate (BPH), frequent urination can also be caused by high fluid intake (especially caffeine or alcohol), diabetes, bladder infections, or other conditions. A medical evaluation is needed to determine the cause.
5. Is prostate cancer curable if caught early?
Yes, absolutely. When prostate cancer is detected while it is still confined to the prostate gland (localized), the 5-year survival rate is nearly 100%. This is the primary goal of screening—to find potentially aggressive cancers early when they are most treatable.
6. How long can you have prostate cancer without knowing?
For many years, or even decades. Because many prostate cancers are very slow-growing (indolent), a man can live his entire life with it without it ever causing a problem or being detected. Screening helps differentiate between these harmless cancers and more aggressive ones that need treatment.
7. Does a high PSA score automatically mean I have cancer?
No. A high PSA is a warning flag, not a diagnosis. Benign Prostatic Hyperplasia (BPH), prostate inflammation (prostatitis), and recent ejaculation can all raise PSA levels. Further investigation, often starting with an MRI, is needed to determine the cause.
8. What is the most important test for detecting prostate cancer?
There isn’t one single “most important” test; it’s a process. The PSA blood test is the initial screening tool. However, the only test that can definitively diagnose prostate cancer is a prostate biopsy, where small tissue samples are examined under a microscope.
Conclusion
Navigating the world of prostate health can feel daunting, filled with uncertainty and confusing information.
But the path to clarity is paved with knowledge and proactive action.
The core messages from this guide are simple but powerful.
- Awareness Over Anxiety: The most critical takeaway is that early prostate cancer is a silent disease. You cannot rely on your body to send you a clear warning signal. Waiting for symptoms is a gamble you don’t need to take.
- Know Your Body & Your Risk: Pay attention to changes in your urinary habits, not as a source of panic, but as a signal to seek professional advice. Crucially, understand your personal risk factors—your age, your race, and your family’s health history are vital pieces of information.
- Dialogue is Key: The single most important step you can take is to have an open, honest conversation with your doctor. Discussing a personalized screening strategy based on your unique risk profile is the cornerstone of modern, responsible men’s healthcare.
Don’t let uncertainty dictate your future. If you are over 50 (or over 45 and in a high-risk group), or if you are experiencing any of the urinary symptoms discussed in this article, schedule an appointment with your doctor or a urologist. This conversation is not a commitment to treatment; it is a commitment to your own health and peace of mind. Early detection saves lives.
Share this article with the men in your life—your father, brothers, sons, and friends.
Normalizing these conversations is how we combat the silence surrounding prostate cancer.
Have you had a conversation about prostate health with your doctor? Share your experience in the comments below to help and encourage others.
Reference
[1] Symptoms of prostate cancer | Cancer Research UK
https://www.cancerresearchuk.org/about-cancer/prostate-cancer/symptoms
[2] What are the signs and symptoms of prostate cancer?
https://zerocancer.org/about-prostate-cancer/symptoms
[3] Understand your symptoms – Prostate Cancer UK Online Community
https://community.prostatecanceruk.org/posts/t28967-Understand-your-symptoms
[4] Nine Signs of Prostate Cancer to Discuss with Your Doctor
https://www.southshorehealth.org/wellness/blog/nine-signs-prostate-cancer-discuss-your-doctor
[5] My partner 47 diagnosed with advanced prostate cancer.
[6] Questions on cancer and other prostate problems
https://www.menshealthforum.org.uk/questions-cancer-and-other-prostate-problems
[7] Forums | ProstateCancer.net