Low testosterone, medically known as male hypogonadism, is a condition where the body doesn’t produce enough of this crucial hormone, leading to symptoms like low sex drive, persistent fatigue, and mood changes.
It’s a health issue that quietly affects millions of men, often masked by the assumption that it’s just a normal part of “getting older”.
The numbers, however, tell a more urgent story.
A landmark study published in The American Journal of Medicine suggests that testosterone deficiency (TD) afflicts approximately 30% of men aged 40-79 years, with prevalence increasing with age and common health conditions like obesity.
This isn’t a rare condition, it’s a widespread health concern that can significantly diminish a man’s quality of life, affecting everything from his physical strength and energy to his mental clarity and emotional well-being.
Many men suffer in silence, attributing their symptoms to stress, a busy life, or the inevitable march of time.
But what if that persistent brain fog, lack of motivation, and dwindling libido aren’t just “part of the package”?
In this comprehensive guide, we will delve deep into the 10 most common signs of low testosterone, explore the underlying causes, explain how a proper diagnosis is made, and outline the modern treatment options available.
If you’ve been feeling unlike yourself, understanding these signs is the first step toward taking back control.
In This Article
The Core of the Matter: What is Low Testosterone?
Before we dive into the symptoms, it’s essential to understand what testosterone is and why it’s so vital for men’s health.
It’s more than just the “male hormone”; it’s a master regulator that influences a vast array of bodily functions.
What Does Testosterone Actually Do for Men?
Testosterone is the primary male sex hormone, but its influence extends far beyond the bedroom.
Produced mainly in the testicles, it’s responsible for the development of male characteristics during puberty and plays a continuous, critical role throughout a man’s life. Its key functions include:
- Sexual Function: It drives libido (sex drive) and plays a role in achieving and maintaining erections.
- Muscle Mass and Strength: Testosterone is anabolic, meaning it helps build and maintain muscle tissue by stimulating protein synthesis.
- Bone Density: It is crucial for bone health, helping to maintain bone mineral density and prevent osteoporosis.
- Fat Distribution: It helps regulate where the body stores fat, and low levels can lead to an increase in body fat, particularly around the abdomen.
- Red Blood Cell Production: Testosterone stimulates the bone marrow to produce red blood cells, which carry oxygen throughout the body.
- Mood and Cognitive Function: It influences mood, confidence, motivation, and cognitive abilities like memory and concentration.
Your body has a sophisticated control system to manage testosterone production, known as the Hypothalamic-Pituitary-Testicular Axis (HPTA).
In simple terms, your brain (hypothalamus and pituitary gland) sends signals to your testicles, telling them when to produce more testosterone. If any part of this communication chain breaks down, levels can fall.
What Testosterone Level is Considered Low?
This is one of the most common questions, and the answer has some important nuances.
According to the American Urological Association (AUA), a total testosterone level below 300 nanograms per deciliter (ng/dL) is a reasonable cutoff to support a diagnosis of low testosterone in adult men.
However, it’s crucial to understand that this number isn’t an absolute, black-and-white threshold. Here’s what adds complexity:
- Symptoms Matter Most: A man with a level of 350 ng/dL but severe symptoms may be considered for treatment, while a man with a level of 280 ng/dL and no symptoms might not. Doctors treat the patient, not just the lab number.
- Time of Day is Critical: Testosterone levels are naturally highest in the morning and decline throughout the day. For this reason, diagnostic blood tests should always be performed early in the morning (typically between 7 AM and 10 AM) to get an accurate reading of peak levels.
- “Free” vs. “Total” Testosterone: Most testosterone in your blood is bound to proteins, making it inactive. “;Free testosterone” is the unbound, active form. Sometimes, total testosterone can be in the low-normal range, but free testosterone is low, which can still cause symptoms.
A diagnosis of low testosterone is never based on a single number. It’s a clinical judgment that combines a patient’s specific symptoms with consistent, low morning testosterone levels confirmed on at least two separate occasions.
The 10 Common Signs of Low Testosterone
The symptoms of low testosterone can be subtle and are often mistaken for other conditions.
Here is a detailed breakdown of the 10 most common signs that should prompt a conversation with your doctor.
Sign #1: Plummeting Sex Drive (Low Libido)
A significant and persistent drop in your desire for sex is the most frequently reported symptom of low testosterone.
The Science Behind It
Testosterone is the primary driver of libido in men.
It acts on specific receptors in the brain to stimulate sexual thoughts, fantasies, and the motivation to seek out sexual activity.
When testosterone levels fall, the “;volume” on these signals is turned down, leading to a noticeable lack of interest.
What It Feels Like in Real Life
This isn’t just feeling “,not in the mood” occasionally.
Men with low T often describe it as a switch being turned off.
As one user on a Reddit forum described it, “It’s not that I couldn’t perform, it’s that the thought of sex just never crossed my mind. My wife would initiate, and it felt like a chore, not a desire”.
It’s a profound lack of initiation and spontaneous sexual thought.
What the Research Says
The link is well-established.
A study in the Journal of Clinical Endocrinology & Metabolism demonstrated a direct, dose-dependent relationship between testosterone levels and sexual desire.
As testosterone levels were experimentally lowered in healthy men, their self-reported levels of sexual desire and arousal dropped in lockstep.
Sign #2: Difficulties with Erections (Erectile Dysfunction)
While low libido is about desire, erectile dysfunction (ED) is about physical performance—the inability to achieve or maintain an erection firm enough for sex.
The Science Behind It
Testosterone’s role in erections is complex.
While erections are primarily driven by nitric oxide release and blood flow, testosterone helps facilitate this process.
It helps maintain the health of the penile tissues and nerves involved in an erection.
More subtly, low testosterone can reduce the frequency of spontaneous nocturnal erections (morning wood), which are important for penile health.
What It Feels Like in Real Life
Men may notice that their erections are less firm, more difficult to achieve even with direct stimulation, or harder to maintain during intercourse.
A classic sign often linked to low T is the disappearance of morning erections.
It’s important to note that while low T can cause ED, most cases of ED are caused by vascular issues (poor blood flow), especially in older men.
What the Research Says
While low testosterone is not the primary cause of all ED, it is a significant contributing factor.
The Cleveland Clinic notes that while testosterone replacement therapy (TRT) is very effective at restoring libido, its effect on ED is more variable.
If ED persists after testosterone levels are normalized, it suggests other underlying causes, like cardiovascular disease, may be present.
Sign #3: Constant Fatigue and Low Energy
This is a profound, bone-deep weariness that isn’t relieved by a good night’s sleep and can be debilitating.
The Science Behind It
The exact mechanism is multifaceted.
Testosterone influences energy metabolism, red blood cell production (which carry oxygen), and has a direct effect on central nervous system arousal and motivation.
Low levels can lead to anemia, reduced mitochondrial function (the “powerhouses” of your cells), and a general sense of lethargy and apathy.
What It Feels Like in Real Life
This isn’t just feeling tired after a long day. It’s a persistent lack of physical and mental energy.
Men often describe needing a nap in the afternoon just to get through the workday, losing interest in hobbies they once loved, and feeling a complete lack of “drive” or “get-up-and-go”.
It’s a feeling of running on empty, no matter how much you rest.
What the Research Says
Fatigue is one of the most common complaints of men with hypogonadism.
A systematic review in Reviews in Urology found that fatigue and low energy were consistently reported across numerous studies of men with testosterone deficiency.
Furthermore, TRT has been shown to significantly improve energy levels and reduce fatigue in these men.
Sign #4: Loss of Muscle Mass and Strength
Despite working out, you may notice a decrease in muscle size and find it harder to lift weights or see progress in the gym.
The Science Behind It
Testosterone is a powerful anabolic hormone. It binds to androgen receptors in muscle cells, signaling them to increase the rate of protein synthesis—the process of repairing and building new muscle fibers.
When testosterone is low, the balance shifts from an anabolic (building) state to a catabolic (breaking down) state, making it difficult to maintain, let alone build, muscle mass.
What It Feels Like in Real Life
This can be incredibly frustrating.
Men who are active may feel like they’re “spinning their wheels” at the gym.
They put in the effort but don’t see the results they used to.
They may notice a visible decrease in the size of their arms, chest, and legs, and a general feeling of weakness or frailty.
Simple tasks like carrying groceries or opening a jar might feel more difficult.
What the Research Says
The effect of testosterone on muscle is well-documented.
The famous “Testosterone Trials” (T-Trials), a series of large-scale studies, found that men treated with testosterone for one year had a significant increase in lean muscle mass and strength (like leg press and chest press strength) compared to those on placebo.
Sign #5: Increase in Body Fat (Especially Belly Fat)
You might notice your waistline expanding and a shift towards a softer, less defined physique, even if your diet and exercise habits haven’t changed.
The Science Behind It
This is a double-edged sword.
First, low testosterone slows down metabolism and reduces muscle mass, which is metabolically active tissue.
This means you burn fewer calories at rest.
Second, and more insidiously, fat cells (particularly visceral belly fat) contain an enzyme called aromatase.
This enzyme converts what little testosterone you have into estrogen.
This creates a vicious cycle: low T leads to more fat, and more fat leads to even lower T.
What It Feels Like in Real Life
Men often report a stubborn accumulation of fat around their midsection that is resistant to diet and exercise.
Some may also develop gynecomastia, an enlargement of male breast tissue, due to the increased ratio of estrogen to testosterone.
This change in body composition can be distressing and negatively impact self-esteem.
What the Research Says
A study in Frontiers in Endocrinology highlights the strong bidirectional relationship between obesity and low testosterone.
It notes that moderate obesity predominantly decreases total testosterone levels.
Conversely, TRT has been consistently shown to reduce fat mass, particularly abdominal fat, and increase lean body mass.
Sign #6: Mood Swings, Irritability, or Depression
You may find yourself feeling unusually grumpy, impatient, sad, or emotionally flat for no apparent reason.
The Science Behind It
Testosterone has a profound impact on the brain’s chemistry, influencing neurotransmitters like serotonin and dopamine that regulate mood.
Low levels can disrupt this delicate balance, leading to symptoms that mimic clinical depression, anxiety, or what’s often dismissed as “grumpy old man syndrome.”
What It Feels Like in Real Life
This can be one of the most disruptive symptoms, affecting relationships at home and at work.
Men describe a short fuse, a lack of patience, and a general sense of pessimism or apathy.
Others report a persistent low-grade depression or a feeling of being emotionally numb.
It’s a change in personality that is often noticed by partners and family members first.
What the Research Says
The link between low testosterone and depression is strong.
The AUA guidelines note that men diagnosed with depression are significantly more likely to have low testosterone.
A 2025 systematic review in Impact of Testosterone on Male Health confirmed that depressive symptoms are strongly associated with low testosterone levels, and that TRT can have a positive effect on mood in hypogonadal men.
Sign #7: Brain Fog and Difficulty Concentrating
You may struggle with memory, find it hard to focus on tasks, or feel a general lack of mental sharpness.
The Science Behind It
The brain is rich in androgen receptors, especially in areas responsible for memory and attention, like the hippocampus and prefrontal cortex.
Testosterone plays a neuroprotective role and influences cognitive processing speed and spatial memory.
Low levels can impair these functions, leading to what is commonly described as “;brain fog.”
What It Feels Like in Real Life
This manifests as difficulty finding words, forgetting why you walked into a room, struggling to follow complex conversations, or a feeling that your brain is “working in slow motion.”
It can impact productivity at work and lead to a frustrating sense of not being as mentally “on” as you used to be.
What the Research Says
Cognitive complaints are common in men with low T.
While research on TRT’s effect on cognition has had mixed results, some studies show modest improvements.
The Cleveland Clinic points out that difficulties with concentration and memory are recognized symptoms of low testosterone, though they can also be caused by the fatigue and poor sleep that often accompany the condition.
Sign #8: Hair Loss (Body and Facial)
While male pattern baldness is primarily genetic, a loss of hair on the body, face, and in the pubic area is a classic sign of low testosterone.
The Science Behind It
Testosterone and its derivative, dihydrotestosterone (DHT), are responsible for the growth of secondary male hair characteristics during puberty—like chest, armpit, facial, and pubic hair.
While high DHT is linked to scalp hair loss, low testosterone can cause a thinning or complete loss of this body hair because there isn’t enough hormone to maintain the follicles.
What It Feels Like in Real Life
Men may notice they have to shave their face less often, or that their beard is becoming patchy.
They might see thinning hair on their chest, legs, and arms, or a reduction in pubic hair.
This is a different pattern from typical male pattern baldness on the head.
What the Research Says
The Mayo Clinic lists decreased body and facial hair growth as a key symptom of male hypogonadism that develops after puberty.
It’s considered a more specific sign of a hormonal issue than scalp hair loss alone.
Sign #9: Reduced Bone Density (Osteoporosis)
This is a silent, long-term symptom that you won’t feel until it’s too late, often resulting in a fracture from a minor fall.
The Science Behind It
Testosterone plays a vital role in the bone remodeling process, where old bone is broken down and replaced with new bone.
It directly stimulates bone-building cells (osteoblasts) and is also converted to estrogen in bone tissue, which is critical for slowing bone breakdown.
Low testosterone disrupts this balance, leading to a net loss of bone mass over time.
What It Feels Like in Real Life
You don’t “feel” your bones getting weaker.
The first sign is often a fracture in a situation that shouldn’t have caused one, such as breaking a wrist from a simple fall or a rib from coughing too hard.
This is why it’s a particularly dangerous and often overlooked consequence of long-term, untreated low testosterone.
What the Research Says
The link between hypogonadism and osteoporosis in men is definitive.
The T-Trials demonstrated that men on TRT for one year had a significant increase in bone mineral density and estimated bone strength, particularly in the spine, compared to the placebo group.
This highlights the importance of maintaining healthy testosterone levels for long-term skeletal health.
Sign #10: Sleep Disturbances or Sleep Apnea
You may have trouble falling or staying asleep, or you may be diagnosed with obstructive sleep apnea (OSA).
The Science Behind It
The relationship between sleep and testosterone is bidirectional.
Poor sleep, especially due to conditions like sleep apnea where oxygen levels drop, puts stress on the body and significantly lowers testosterone production.
Conversely, low testosterone can contribute to changes in body composition (increased fat) and muscle tone in the airway, which can worsen or even cause sleep apnea. It can also disrupt the natural sleep-wake cycle.
What It Feels Like in Real Life
Men may experience insomnia, wake up frequently during the night, or wake up feeling unrefreshed no matter how long they were in bed.
Their partners may report loud snoring, gasping, or pauses in breathing during sleep—all hallmark signs of sleep apnea.
The resulting daytime fatigue creates a vicious cycle with the fatigue caused directly by low T.
What the Research Says
Research has firmly established this two-way street.
A study in the Journal of the American Medical Association (JAMA) found that just one week of sleep restriction (5 hours per night) in healthy young men decreased their daytime testosterone levels by 10-15%.
Furthermore, Cleveland Clinic lists obstructive sleep apnea as both a potential cause and a comorbidity of low testosterone.
Understanding the “Why”: What Causes Low Testosterone?
Once you recognize the signs, the next logical question is, “Why is this happening to me?”.
The causes of low testosterone, or hypogonadism, can be broadly divided into problems with the testicles themselves, problems with the brain signals that control them, and a host of lifestyle factors that disrupt the entire system.
Is It Just Aging, or Is Something Else Causing My Low T?
Doctors categorize the causes into two main types:
Primary Hypogonadism (A Problem with the Testicles)
Think of this as a problem at the “factory.”
The testicles themselves are unable to produce enough testosterone, even though the brain is sending the right signals.
In this case, blood tests will show low testosterone but high levels of the signaling hormones (LH and FSH) as the brain tries to overcompensate. Causes include:
- Physical Injury: Direct trauma to the testicles.
- Chemotherapy or Radiation: These treatments can damage the testosterone-producing Leydig cells.
- Infections: Mumps, particularly after puberty, can cause inflammation (orchitis) that damages the testicles.
- Genetic Conditions: Klinefelter’s syndrome (an extra X chromosome) is a common genetic cause.
- Undescended Testicles: A condition from birth that can impair testicular function later in life.
Secondary Hypogonadism (A Problem with the Brain’s Signals)
Think of this as a problem with “management”.
The testicles are healthy, but the hypothalamus or pituitary gland in the brain isn’t sending the necessary signals (GnRH and LH) to tell them to produce testosterone.
Blood tests will show both low testosterone and low or inappropriately normal levels of LH and FSH. Causes include:
- Pituitary Disorders: Tumors (usually benign), inflammation, or injury to the pituitary gland.
- Inflammatory Diseases: Conditions like sarcoidosis or tuberculosis can affect the hypothalamus.
- High Prolactin Levels: High levels of the hormone prolactin can suppress testosterone production.
The Biggest Lifestyle Factors and Comorbidities
For most men, especially as they age, low testosterone is not caused by a single dramatic event but by a combination of factors related to aging and overall health.
This is often called “late-onset hypogonadism.”
- Aging (Andropause): After age 30, most men experience a gradual decline in testosterone of about 1% per year. This is a natural process, but for some, the decline is steeper or starts from a lower baseline, leading to symptomatic low T. The chart below illustrates the typical decline in average testosterone levels across a man’s lifespan.
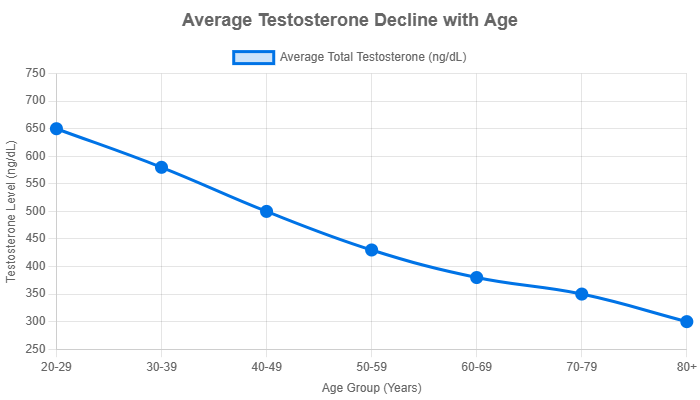
Data for this chart is based on aggregated reference ranges from sources like Labcorp OnDemand and other clinical guidelines. Individual levels can vary significantly.
- Obesity and Metabolic Syndrome: This is arguably the most significant modifiable risk factor. As mentioned earlier, excess body fat, especially visceral fat, increases the activity of the aromatase enzyme, which converts testosterone to estrogen, further suppressing testosterone production in a vicious cycle.
- Type 2 Diabetes: The link is incredibly strong. Studies show that up to 25% of men with Type 2 diabetes have low testosterone, compared to about 13% of men without diabetes. Insulin resistance appears to disrupt the HPTA signals.
- Chronic Illness & Stress: Chronic diseases of the liver or kidneys, HIV/AIDS, and high levels of chronic stress (which elevates the hormone cortisol) can all suppress the body’s ability to produce adequate testosterone.
The Path Forward: Diagnosis and Treatment
If you’re experiencing several of the signs discussed, the next step is not to self-diagnose or buy supplements online, but to seek a professional medical evaluation. Here’s what that process looks like.
How Do I Get a Proper Diagnosis for Low Testosterone?
A thorough diagnosis is a multi-step process designed to confirm low levels and rule out other conditions.
- Symptom Discussion: The process begins with a detailed conversation with your doctor. Be honest and specific about your symptoms—when they started, how they affect your life, and what you’re experiencing. This subjective information is just as important as any lab test.
- Blood Test: If your symptoms are suggestive of low T, your doctor will order a blood test to measure your total testosterone level. As mentioned, this must be a morning blood draw (between 7-10 AM) to be accurate.
- Confirmatory Testing: Because levels can fluctuate, a single low reading is not enough for a diagnosis. Your doctor will order a second morning blood test on a different day to confirm the result.
- Further Investigation: If both tests come back low, your doctor may order additional blood work to determine the cause. This often includes measuring Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH). This helps differentiate between primary (testicular) and secondary (brain signal) hypogonadism. They may also check your “free” testosterone, prolactin, and estrogen levels.
- Ruling Out Other Conditions: A good physician will also be a good detective. Symptoms like fatigue and depression can be caused by many other issues, such as thyroid problems, anemia, vitamin deficiencies, or clinical depression itself. Your doctor will likely run tests to rule these out before settling on a diagnosis of low testosterone.
What Are My Treatment Options for Low Testosterone (TRT)?
If you are diagnosed with clinical hypogonadism, the standard medical treatment is Testosterone Replacement Therapy (TRT).
The goal of TRT is to restore your testosterone levels to a normal physiological range, thereby alleviating your symptoms.
There are several effective methods for delivering testosterone, each with its own pros and cons.
Comparison of TRT Methods
| Method | Frequency | Pros | Cons |
|---|---|---|---|
| Injections | Every 1-2 weeks (or smaller, more frequent self-injections) | Highly effective, low cost, flexible dosing. | Causes peaks and troughs in levels (can affect mood/energy), requires needles. |
| Gels | Daily | Provides stable, daily hormone levels; non-invasive. | Risk of transference to others (partners, children) through skin contact; can cause skin irritation; can be messy. |
| Patches | Daily | Provides stable hormone levels; convenient. | Often causes significant skin irritation/rashes; may not adhere well with sweat. |
| Pellets | Every 3-6 months | “Set it and forget it” convenience; very stable hormone levels. | Requires a minor in-office surgical procedure for insertion and removal; dosing is not easily adjustable. |
Is TRT Safe? Discussing the Risks and Benefits
When prescribed and monitored by a qualified doctor for a legitimate diagnosis, TRT is generally safe and highly effective.
The benefits can be life-changing: improved libido, energy, mood, muscle mass, and bone density.
However, it is not without risks and requires ongoing medical supervision. Potential risks include:
- Polycythemia: An increase in red blood cell count, which can thicken the blood and increase the risk of clotting. This is monitored with regular blood work.
- Infertility: Exogenous testosterone signals the brain to shut down its own production, which also halts sperm production. TRT is a form of male contraception and should not be used by men trying to conceive.
- Cardiovascular Concerns: The debate on TRT and heart health is ongoing. While some older studies suggested a risk, more recent, robust research, including the TRAVERSE trial published in 2023, has shown TRT to be largely safe from a cardiovascular standpoint in appropriately selected men. However, it’s a crucial point of discussion with your doctor, especially if you have pre-existing heart disease.
- Prostate Health: TRT does not cause prostate cancer, but it can stimulate the growth of an existing cancer. Your doctor will monitor your prostate health via PSA tests.
The decision to start TRT is a personal one, made in partnership with your doctor after weighing the potential benefits against the risks for your individual health profile.
Can I Increase My Testosterone Without a Prescription?
This is a common question, especially for men with borderline-low levels or those hesitant to start medical therapy.
The answer is yes—lifestyle modifications can have a meaningful impact on your natural testosterone production.
However, it’s important to have realistic expectations.
For men with clinically diagnosed hypogonadism (levels below 300 ng/dL with symptoms), lifestyle changes alone are unlikely to be sufficient to resolve symptoms.
For others, they are the first and most important line of defense.
- Weight Management: This is the single most effective natural strategy. Losing excess body fat, particularly belly fat, reduces the aromatase enzyme activity, meaning less of your testosterone is converted to estrogen.
- Exercise (The Right Kind): Resistance training (weightlifting) and High-Intensity Interval Training (HIIT) have been shown to provide a short-term boost in testosterone and improve the hormonal environment long-term by building muscle and reducing fat.
- Optimize Sleep: Prioritize 7-9 hours of quality sleep per night. Most of your daily testosterone is produced during sleep, so chronic sleep deprivation will crush your levels.
- Stress Reduction: Chronic stress elevates cortisol, a hormone that is catabolic and directly inhibits testosterone production. Practices like meditation, mindfulness, and ensuring you have downtime can help lower cortisol.
- Balanced Diet: Ensure your diet includes adequate healthy fats (crucial for hormone production), zinc (found in meat, shellfish), and Vitamin D. Many people are deficient in Vitamin D, which functions like a hormone in the body.
A word of caution on “T-Boosters”: The over-the-counter supplement market is filled with products making bold claims.
Most of these “testosterone boosters” are not supported by science and do not significantly raise testosterone levels.
Some may contain ingredients that help with libido or energy through other mechanisms, but they are not a substitute for medical treatment.
Frequently Asked Questions (FAQ)
1. At what age do testosterone levels start to drop?
Testosterone levels typically peak in late adolescence and early adulthood. A gradual decline of about 1% per year usually begins around age 30. This rate can vary significantly between individuals based on genetics, health, and lifestyle factors.
2. Can stress cause low testosterone?
Yes. Chronic stress leads to elevated levels of the hormone cortisol. Cortisol has an inverse relationship with testosterone; when cortisol is high, it can suppress the body’s ability to produce testosterone. Managing stress is a key component of hormonal health.
3. Will TRT make me infertile?
Yes, TRT acts as a male contraceptive by shutting down your body’;s natural sperm production. Men who are currently trying to conceive should not use TRT. Other therapies, like HCG, can be used to stimulate testosterone production while preserving fertility.
4. How quickly will I feel better on TRT?
It varies. Improvements in libido, energy, and mood can often be felt within the first 3-6 weeks. Changes in muscle mass and body composition take longer, typically becoming noticeable after 3-6 months of consistent therapy and exercise.
5. Do testosterone boosters from the store actually work?
Most over-the-counter “T-boosters” have little to no scientific evidence to support their claims of significantly increasing testosterone levels. They are not regulated by the FDA and are not a substitute for medical treatment for diagnosed hypogonadism.
6. Can a vasectomy cause low testosterone?
No. A vasectomy is a procedure that blocks the vas deferens, the tubes that carry sperm. It has no effect on the testicles’ ability to produce testosterone, which is released directly into the bloodstream. A vasectomy does not cause low T.
7. Is low testosterone linked to heart problems?
The relationship is complex. Low testosterone itself is associated with risk factors for heart disease, like obesity and diabetes. While past concerns existed about TRT, recent large-scale studies have shown it to be generally safe for the heart in properly monitored men.
8. What kind of doctor should I see for low testosterone?
You can start with your primary care physician (PCP). If a diagnosis is confirmed, they may refer you to a specialist. The two main specialists for low testosterone are Urologists, who focus on the male reproductive system, and Endocrinologists, who specialize in hormones.
Conclusion and Next Steps
Low testosterone is far more than just a decline in sex drive, it’s a legitimate medical condition with a wide array of distinct physical, mental, and emotional signs.
From persistent fatigue and brain fog to changes in body composition and mood, the symptoms can profoundly impact a man’s vitality and quality of life.
While aging plays a role, factors like obesity, poor sleep, and chronic illness are often the primary drivers.
Recognizing the signs is the first, most crucial step.
The fatigue you can’t shake, the frustration in the gym, and the emotional irritability you’re experiencing are not just things you have to “live with”.
They are signals from your body that something is out of balance.
If these symptoms resonate with you, the most powerful next step is to start a conversation with your doctor.
Self-diagnosing or experimenting with unregulated supplements can be ineffective and potentially harmful.
A proper medical evaluation is the only way to get a definitive answer and explore safe, effective treatment options tailored to your specific needs.
Taking charge of your hormonal health is a proactive step towards reclaiming your energy, strength, and overall well-being for years to come.
Have you experienced any of these signs? Share your experience or questions in the comments below to help foster a supportive community.
Reference
[1] Testosterone Replacement in Men With Hypogonadism …
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2811123
[2] Testosterone Deficiency
https://www.amjmed.com/article/s0002-9343(11)00274-9/fulltext
[3] Understanding the signs, causes and treatment options for low …
[4] Testosterone therapy in older men: clinical implications of recent …
https://academic.oup.com/ejendo/article/191/1/R22/7698939
[5] Low Testosterone Associated With Obesity and the Metabolic …
https://pmc.ncbi.nlm.nih.gov/articles/PMC3120209
[6] Low Testosterone (Low T): Causes, Symptoms & Treatment
https://my.clevelandclinic.org/health/diseases/15603-low-testosterone-male-hypogonadism
[7] Low Testosterone and Your Health – WebMD
https://www.webmd.com/men/what-low-testosterone-can-mean-your-health
[8] How low testosterone treatment can help – and harm – a man’s sex …
https://utswmed.org/medblog/low-testosterone-symptoms-causes-treatment
[9] What are the signs of low testosterone in men? – Bupa UK
https://www.bupa.co.uk/newsroom/ourviews/low-testosterone-men
[10] Testosterone therapy: Potential benefits and risks as you age
[11] Risks of testosterone replacement therapy in men – PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC3897047
[12] Full article: Testosterone therapy over 60 months improves aging …
https://www.tandfonline.com/doi/full/10.1080/13685538.2024.2357548
[13] Lowered testosterone in male obesity: mechanisms, morbidity and …
https://pmc.ncbi.nlm.nih.gov/articles/PMC3955331
[14] Impact of Testosterone on Male Health: A Systematic Review – PMC

