Celiac disease in adults often presents with non-digestive “hidden” signs like persistent fatigue, iron-deficiency anemia and neurological issues, rather than classic gut symptoms.
This atypical presentation is a primary reason why so many cases are missed. In fact, an estimated 83% of Americans with celiac disease are undiagnosed or misdiagnosed with other conditions.
This staggering statistic highlights a major public health challenge, often visualized as the “celiac iceberg”, where the vast majority of cases lie undetected beneath the surface of clinical awareness.
For many adults, the journey to a diagnosis is long and frustrating, marked by years of unexplained health problems that affect nearly every system in the body.
This comprehensive guide will delve deep into the subtle, surprising, and often-overlooked symptoms of adult-onset celiac disease.
We will explore the complex diagnostic process, explain the critical importance of proper medical testing before changing your diet, and provide a roadmap for managing this serious autoimmune condition to reclaim your health and well-being.
In This Article
What is Celiac Disease and Why is it More Than a Digestive Issue?
At its core, celiac disease is not a food allergy or a simple intolerance. It is a serious, chronic autoimmune disorder that occurs in genetically predisposed individuals where the ingestion of gluten leads to damage in the small intestine.
Unlike a food sensitivity, where the body might have trouble digesting a substance, celiac disease triggers a complex and destructive immune response that has systemic, body-wide consequences.
The Autoimmune Reaction: Your Body Attacking Itself
When a person with celiac disease consumes gluten, their immune system mistakenly identifies components of gluten as a threat. This triggers an inflammatory cascade.
The immune system produces antibodies, most notably against an enzyme called tissue transglutaminase (tTG).
These antibodies don’t just attack the gluten proteins, they also attack the lining of the small intestine itself.
This self-attack is the hallmark of an autoimmune disease, placing celiac disease in the same category as conditions like rheumatoid arthritis and type 1 diabetes.
Gluten: The Trigger Protein
Gluten is a family of proteins found in certain grains. The primary culprits are:
- Wheat (including varieties like spelt, kamut, farro and durum)
- Barley
- Rye
These grains are staples in the Western diet, found in everything from bread, pasta and cereal to less obvious sources like soups, sauces, salad dressings and even some medications.
This ubiquity makes avoiding gluten a significant challenge for those diagnosed with celiac disease.
Villi Damage: The Root of Malabsorption
The small intestine is lined with tiny, finger-like projections called villi.
Their purpose is to dramatically increase the surface area of the intestine, allowing for the efficient absorption of nutrients from food.
In celiac disease, the autoimmune attack flattens and destroys these villi, a condition known as villous atrophy.
This damage severely impairs the body’s ability to absorb essential vitamins, minerals and calories, leading to a state of malabsorption and malnutrition, no matter how much healthy food a person eats.
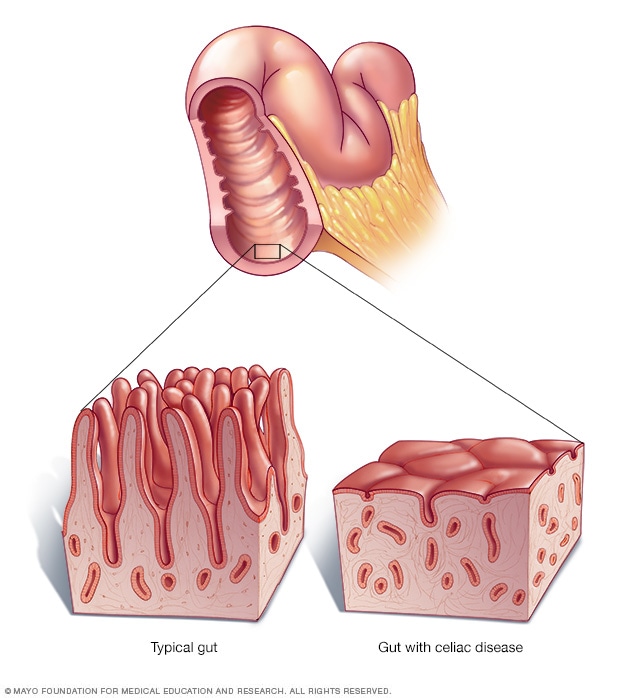
As shown in this illustration, the autoimmune response in celiac disease damages the intestinal villi, leading to malabsorption.
This malabsorption is the direct cause of many of the “hidden” signs of celiac disease.
When the body can’t get the iron, calcium, vitamin D, B vitamins and other nutrients it needs, it can lead to a cascade of problems far beyond the digestive tract, affecting the bones, brain, skin and reproductive system.
Why Are So Many Adults with Celiac Disease Undiagnosed?
The path to a celiac disease diagnosis is notoriously difficult for adults.
While awareness has grown, a significant gap remains between the number of people affected and those who receive a formal diagnosis.
Several key factors contribute to this widespread underdiagnosis.
The “Celiac Iceberg”: The Scale of the Undiagnosed Problem
Experts often use the “celiac iceberg” analogy to describe the disease’s epidemiology.
The tip of the iceberg, visible above the water, represents the small number of patients diagnosed with classic, severe symptoms.
The massive, hidden part of the iceberg submerged below represents the far larger population of individuals with atypical, subtle, or even no symptoms (silent celiac disease) who remain undiagnosed.
Studies suggest that for every one person diagnosed, there may be five to seven others who have the disease but don’t know it.
The Shift from Classic to Atypical Presentations
Historically, celiac disease was considered a rare childhood disease characterized by severe digestive distress, malnutrition and failure to thrive.
However, research over the past few decades has revealed a dramatic shift.
Today, adults are more likely to be diagnosed than children, and they are far more likely to present with non-digestive or “atypical” symptoms.
More than half of adults with newly diagnosed celiac disease report no significant digestive issues, making it easy for both patients and doctors to overlook the possibility.
Overlap with Other Conditions
Many of the hidden signs of celiac disease are non-specific and overlap with other common conditions, leading to frequent misdiagnosis. For example:
- Fatigue and brain fog may be attributed to chronic fatigue syndrome, fibromyalgia or simply stress.
- Bloating and abdominal pain are hallmark symptoms of Irritable Bowel Syndrome (IBS). A significant number of people diagnosed with IBS may actually have undiagnosed celiac disease.
- Anxiety and depression might be treated as primary psychiatric conditions without investigating an underlying physical cause.
- Joint pain can be mistaken for arthritis.
The Long Road to Diagnosis
Because of these challenges, the average time from the onset of symptoms to a formal diagnosis of celiac disease in the United States can be a staggering 5 to 11 years.
During this time, individuals may see multiple doctors and specialists, undergo numerous tests for other conditions and suffer from declining health and quality of life, all while the underlying autoimmune damage continues unchecked.
What Are the Hidden, Non-Digestive Signs of Celiac Disease in Adults?
While digestive issues can occur, the majority of adults with celiac disease experience symptoms outside of the gut.
These “extraintestinal” manifestations are the direct result of systemic inflammation, the autoimmune response and chronic malabsorption of nutrients.
Recognizing these hidden signs is crucial for a timely diagnosis.
Systemic Symptoms: The Body-Wide Impact
These are generalized symptoms that affect your overall sense of well-being.
- Persistent, Overwhelming Fatigue: This is more than just feeling tired. It’s a profound lack of energy that isn’t relieved by rest, often caused by a combination of chronic inflammation, malnutrition and anemia.
- Unexplained Weight Loss: Despite a normal or even increased appetite, some adults lose weight due to severe malabsorption. Conversely, some may experience unexplained weight gain.
- “Brain Fog” or Cognitive Impairment: Difficulty concentrating, memory lapses and a feeling of mental cloudiness are commonly reported. This is thought to be linked to both inflammation and nutrient deficiencies affecting brain function.
Neurological Manifestations: The Brain-Gut Connection
The nervous system is surprisingly vulnerable to the effects of celiac disease.
Neurological symptoms are present in up to 10% of patients and can sometimes be the only sign of the disease.
- Migraines & Chronic Headaches: A higher prevalence of severe headaches and migraines is seen in individuals with celiac disease compared to the general population.
- Peripheral Neuropathy: This involves damage to the nerves outside the brain and spinal cord, causing symptoms like numbness, tingling, burning or pain, typically in the hands and feet.
- Balance Problems (Gluten Ataxia): In rare cases, the immune response can target the cerebellum, the part of the brain that controls coordination and balance, leading to unsteadiness and difficulty walking.
- Anxiety and Depression: The link is complex, likely involving a mix of chronic inflammation, nutrient deficiencies (like B vitamins), and the psychological burden of living with a chronic, undiagnosed illness.
Dermatological Signs: Your Skin’s Cry for Help
Dermatitis Herpetiformis (DH) is not just a rash, it is the skin manifestation of celiac disease. It’s caused by the same autoimmune reaction to gluten.
- Dermatitis Herpetiformis (DH): This is an intensely itchy, blistering skin rash that typically appears symmetrically on the elbows, knees, buttocks, and back. People with DH almost always have celiac disease, even if they have no digestive symptoms. A skin biopsy is used to diagnose DH.
- Other Skin Issues: While less specific, some individuals may experience other chronic skin problems that improve on a gluten-free diet.
Hematological and Vascular Clues: What Your Blood Reveals
Blood work abnormalities are among the most common hidden signs of celiac disease.
- Iron-Deficiency Anemia: This is a classic sign, especially when it is resistant to treatment with oral iron supplements. The damaged intestine simply cannot absorb enough iron from food or pills.
- Unexplained B12 or Folate Deficiency: Like iron, these crucial B vitamins are absorbed in the small intestine, and their levels can plummet due to villous atrophy.
- Reduced Spleen Function (Hyposplenism): The spleen helps filter blood and fight infections. In some people with celiac disease, it can become less effective, making them more susceptible to certain infections.
Musculoskeletal Problems: Aches, Pains, and Bone Loss
The inability to absorb calcium and vitamin D has a direct and devastating impact on bone health.
- Osteoporosis or Osteopenia: A diagnosis of low bone density, especially at a young age (“early-onset osteoporosis”), should be a major red flag for undiagnosed celiac disease.
- Joint Pain (Arthralgia) and Muscle Pain (Myalgia): Widespread aches and pains are common, likely due to systemic inflammation.
- Bone Pain and Increased Fracture Risk: A direct consequence of weakened bones.
Reproductive and Hormonal Health Issues
Malnutrition and inflammation can disrupt the delicate balance of the endocrine system.
- Infertility: Unexplained infertility in both men and women can be a sign of celiac disease.
- Recurrent Miscarriages: Multiple pregnancy losses have been linked to the autoimmune activity of the disease.
- Irregular Menstrual Cycles: Amenorrhea (absence of periods) or other irregularities are common.
Oral and Dental Manifestations
The mouth can offer some of the earliest clues.
- Dental Enamel Defects: Permanent teeth may show signs of poor development, such as pitting, discoloration (white, yellow, or brown spots), or a translucent appearance. This damage occurs while the teeth are forming and is irreversible.
- Recurrent Canker Sores (Aphthous Stomatitis): Frequent, painful sores inside the mouth are a common complaint.
Liver and Gallbladder Involvement
An unexplained finding on a routine blood test can be a key indicator.
- Unexplained Elevated Liver Enzymes: Mild to moderate elevations in liver enzymes (ALT and AST) with no other cause (like viral hepatitis or alcohol use) can be a sign of celiac disease. In most cases, these levels return to normal after starting a gluten-free diet.
Do Adults Still Get the “Classic” Digestive Symptoms?
Yes, while non-digestive symptoms are more common in adults, a significant number of individuals still experience the “classic” gastrointestinal (GI) signs of celiac disease.
For some, these are their primary complaints, while for others, they occur alongside the hidden, systemic symptoms.
It’s important to note that the severity can range from mild and intermittent to severe and chronic.
Common Digestive Symptoms in Adults
- Chronic Diarrhea: Often described as loose, watery and frequent stools.
- Bloating and Gas: A feeling of fullness, pressure, or painful trapped gas is extremely common due to maldigestion and fermentation of food in the gut.
- Abdominal Pain: This can range from dull, cramping aches to sharp, severe pain.
- Constipation: While less common than diarrhea, a surprising number of adults with celiac disease report chronic constipation as their main digestive issue.
- Nausea and Vomiting: Though more prevalent in children, some adults experience these symptoms, especially after consuming a large amount of gluten.
- Lactose Intolerance: The damage to the intestinal villi can lead to a temporary inability to produce lactase, the enzyme needed to digest dairy. This often resolves after the gut has healed on a gluten-free diet.
Why Symptoms Vary So Much Between Individuals
The presentation of celiac disease is incredibly heterogeneous.
Two people with the same condition can have completely different sets of symptoms.
The reasons for this variability are not fully understood but are thought to involve:
- The extent of intestinal damage: Some people may have patchy damage, while others have widespread villous atrophy.
- Age at onset: The disease may manifest differently when it becomes active in adulthood versus childhood.
- Genetic factors: Beyond the primary HLA-DQ2/DQ8 genes, other genes may influence the type and severity of the immune response.
- The gut microbiome: The composition of bacteria in the gut may play a role in modulating the immune system’s reaction to gluten.
How is Celiac Disease Officially Diagnosed?
Diagnosing celiac disease is a multi-step process that requires careful medical evaluation.
Self-diagnosis or starting a gluten-free diet based on suspicion is strongly discouraged, as it can interfere with the accuracy of the tests and prevent a correct diagnosis.
The Critical First Step: Do NOT Go Gluten-Free Yet!
For the diagnostic tests to be accurate, you must be actively consuming gluten. The tests work by detecting the body’s immune response to gluten. If you remove gluten from your diet, the antibody levels will drop and the intestinal damage may begin to heal, leading to false-negative results. If you have already started a gluten-free diet, your doctor may recommend a “gluten challenge” (eating gluten daily for several weeks) before testing.
Step 1: Serology (Blood Testing)
The initial step is a simple blood draw to screen for specific antibodies that are hallmarks of celiac disease.
The most common and reliable tests are:
- Tissue Transglutaminase IgA Antibody (tTG-IgA): This is the single most sensitive and specific test for celiac disease and is the preferred test for initial screening.
- Endomysial IgA Antibody (EMA-IgA): This test is highly specific but less sensitive than the tTG-IgA test. It is often used as a confirmatory blood test.
- Deamidated Gliadin Peptide (DGP-IgA and DGP-IgG): These tests can be useful, especially in young children and in individuals who are deficient in IgA (a condition that can cause a false-negative tTG-IgA result).
Your doctor will also likely test your total serum IgA level to rule out an IgA deficiency.
Step 2: The Endoscopic Biopsy
If the blood tests are positive and suggest celiac disease, the next step is to confirm the diagnosis with an upper endoscopy.
This is considered the “gold standard” for diagnosis.
- The Procedure: A gastroenterologist passes a thin, flexible tube with a camera (an endoscope) through your mouth, down your esophagus and into the small intestine.
- The Biopsy: The doctor takes several tiny tissue samples (biopsies) from the lining of the small intestine (specifically, the duodenum).
- The Analysis: A pathologist examines the tissue under a microscope to look for the characteristic damage of celiac disease, such as villous atrophy, crypt hyperplasia and an increase in intraepithelial lymphocytes.
The Role of Genetic Testing (HLA-DQ2/DQ8)
Genetic testing involves a blood test or cheek swab to see if you carry the genes associated with celiac disease (HLA-DQ2 or HLA-DQ8).
Its primary value is its high negative predictive value.
- What it means: Nearly all people with celiac disease have one of these genes. Therefore, if you test negative for both HLA-DQ2 and HLA-DQ8, it is extremely unlikely that you have or will ever develop celiac disease. It effectively rules out the condition.
- What it doesn’t mean: A positive result does not diagnose celiac disease. About 30-40% of the general population carries these genes, but only a small fraction of them will ever develop the disease. A positive result simply means you are genetically predisposed.
Diagnostic Pathway for Celiac Disease
| Test Type | What It Measures | Purpose | Key Consideration |
|---|---|---|---|
| Serology (e.g., tTG-IgA) | Autoantibodies produced in response to gluten. | Initial screening to identify individuals who likely have celiac disease. | Must be on a gluten-containing diet. Can be falsely negative in cases of IgA deficiency. |
| Endoscopy with Biopsy | Physical damage (villous atrophy) to the small intestine lining. | Confirms the diagnosis by providing direct evidence of intestinal damage. The “gold standard”. | Must be on a gluten-containing diet. An invasive but essential procedure for definitive diagnosis. |
| Genetic Testing (HLA-DQ2/DQ8) | Presence of genes that predispose to celiac disease. | Primarily used to rule out the disease. Helpful for at-risk family members or in ambiguous cases. | A positive result does not diagnose the disease, only indicates genetic risk. |
What are the Risks of Undiagnosed or Untreated Celiac Disease?
Leaving celiac disease untreated is not an option.
It is a serious condition with significant long-term health consequences that extend far beyond digestive discomfort.
The ongoing autoimmune attack and chronic malabsorption can lead to a variety of severe complications.
Long-Term Malnutrition and Its Consequences
Even with a healthy diet, the damaged intestine cannot absorb nutrients properly.
This leads to deficiencies in iron, calcium, vitamin D, folate, vitamin B12 and other essential nutrients, causing a wide range of health problems including severe anemia, fatigue and neurological issues.
Increased Risk of Other Autoimmune Diseases
People with celiac disease have a significantly higher risk of developing other autoimmune conditions.
The chronic inflammation can dysregulate the immune system, making it more likely to launch other self-attacks.
Common co-occurring conditions include:
- Type 1 Diabetes
- Autoimmune Thyroid Disease (Hashimoto’s or Graves’ disease)
- Autoimmune Liver Disease
- Addison’s Disease
- Sjögren’s Syndrome
Severe Bone Weakening (Osteoporosis)
The impaired absorption of calcium and vitamin D leads directly to a loss of bone density.
Untreated celiac disease is a major cause of early-onset osteoporosis, dramatically increasing the risk of painful fractures later in life.
Increased Cancer Risk
While the absolute risk is still low, individuals with long-standing, untreated celiac disease have an increased risk of developing certain types of cancer, most notably intestinal lymphomas (like enteropathy-associated T-cell lymphoma) and small bowel cancer.
Adhering to a strict gluten-free diet has been shown to significantly reduce this risk.
Neurological Complications
If left untreated, neurological symptoms like peripheral neuropathy and gluten ataxia can become permanent and irreversible, even after starting a gluten-free diet.
Early diagnosis and treatment are critical to prevent long-term nerve damage.
Non-Responsive and Refractory Celiac Disease
A small percentage of individuals do not improve on a gluten-free diet.
This is known as non-responsive celiac disease.
The most common cause is unintentional, ongoing gluten exposure from cross-contamination.
However, in very rare cases, individuals may have refractory celiac disease, a severe form where the intestinal damage persists despite a strict gluten-free diet, often requiring immunosuppressive medications.
What is the Treatment for Celiac Disease?
Currently, there is no cure or medication to prevent the autoimmune reaction in celiac disease.
The only available and effective treatment is a strict, 100% gluten-free diet for life.
The Only Treatment: A Strict, Lifelong Gluten-Free Diet
This is not a lifestyle choice but a medical necessity.
Adherence to the diet allows the intestinal villi to heal, which resolves symptoms, corrects nutrient deficiencies and reduces the long-term risk of complications.
For most people, symptoms begin to improve within weeks of eliminating gluten, though complete intestinal healing can take months or even a couple of years.
What to Eat and What to Avoid
Learning the celiac disease diet involves understanding which foods are safe and which contain gluten.
- Foods to AVOID (Contain Gluten):
- Wheat (all varieties, including spelt, kamut, farro, durum, semolina)
- Barley
- Rye
- Malt (which is made from barley)
- Triticale (a cross between wheat and rye)
- Naturally Gluten-Free Foods (Safe to Eat):
- Fruits and vegetables
- Meat, poultry, fish and eggs
- Beans, legumes, nuts and seeds
- Dairy products
- Grains like rice, corn (maize), quinoa, buckwheat, millet and certified gluten-free oats
The Hidden Dangers: Cross-Contamination and Hidden Gluten
Following a gluten-free diet goes beyond simply avoiding bread and pasta.
Gluten can be a hidden ingredient in many processed foods and cross-contamination is a major concern.
- Hidden Gluten: Always read labels. Gluten can be found in soy sauce, salad dressings, marinades, soups, processed meats, candy and even nutritional supplements and medications.
- Cross-Contamination: This occurs when gluten-free food comes into contact with gluten. Even a few crumbs can be enough to trigger an immune reaction. Common sources include shared toasters, cutting boards, utensils, condiment jars and deep fryers in restaurants.
The Importance of a Registered Dietitian
Upon diagnosis, it is essential to work with a registered dietitian who specializes in celiac disease.
They can provide invaluable guidance on:
- Reading food labels and identifying hidden gluten.
- Preventing cross-contamination at home and when dining out.
- Ensuring a balanced and nutritionally complete diet.
- Finding gluten-free substitutes for favorite foods.
How Does Celiac Disease Affect Quality of Life?
A diagnosis of celiac disease can be life-changing, bringing both relief from years of unexplained symptoms and a new set of challenges.
The impact on daily life is profound and extends beyond just the food on one’s plate.
The Psychological and Social Burden
The need for constant vigilance around food can create significant stress and anxiety.
- Food Anxiety: Many individuals develop a fear of eating, especially in situations they can’t control, worried about accidental gluten exposure and the resulting illness.
- Social Isolation: Social events that revolve around food—parties, dinners with friends, work lunches—can become sources of stress rather than enjoyment. It can be difficult and isolating to navigate these situations safely.
- Feeling Like a Burden: Patients often express feeling like an inconvenience to friends, family, or restaurant staff when they have to make special requests or ask detailed questions about ingredients.
Navigating the Gluten-Free World
While the availability of gluten-free products has improved dramatically, navigating the world is still a challenge.
Traveling requires extensive pre-planning, and dining out necessitates a high level of trust in the restaurant’s kitchen staff to prevent cross-contamination.
The financial cost can also be a burden, as certified gluten-free products are often significantly more expensive than their conventional counterparts.
Finding Support and Community
Connecting with others who have celiac disease can be incredibly helpful. Support groups, both online and in-person, provide a space to share experiences, exchange tips, and feel understood.
Organizations like the Celiac Disease Foundation and Beyond Celiac offer a wealth of resources, recipes and community support to help individuals thrive on a gluten-free diet.
Frequently Asked Questions About Celiac Disease
1. Can you develop celiac disease as an adult?
Yes, absolutely. While it can be diagnosed in childhood, it is very common for celiac disease to develop or be diagnosed at any age, including in older adults. The onset can sometimes be triggered by a stressful event like surgery, pregnancy or a viral infection.
2. What’s the difference between celiac disease and gluten sensitivity?
Celiac disease is an autoimmune disorder that causes intestinal damage. Non-celiac gluten sensitivity (NCGS) involves symptoms that react to gluten but without the specific antibodies or intestinal damage seen in celiac disease. NCGS is a diagnosis of exclusion made after ruling out celiac disease and wheat allergy.
3. If my blood test is negative, can I still have celiac disease?
It’s possible, but less likely. A false-negative can occur if you were not eating gluten before the test or if you have an IgA deficiency. If suspicion remains high despite a negative test, genetic testing or even an endoscopy may still be considered by your doctor.
4. How long does it take to feel better on a gluten-free diet?
Most people start to notice an improvement in their symptoms within a few days to a few weeks. However, complete healing of the intestine and resolution of all symptoms, especially neurological ones, can take many months or even a couple of years.
5. Is a gluten-free diet healthy for someone without celiac disease?
Not necessarily. Many processed gluten-free products are lower in fiber, iron, and B vitamins and higher in sugar and fat than their gluten-containing counterparts. For those without a medical need, a balanced diet that includes whole grains is generally healthier than a restrictive gluten-free one.
6. If a family member has celiac disease, should I get tested?
Yes. First-degree relatives (parents, siblings, children) of someone with celiac disease have about a 1 in 10 risk of developing it themselves. Screening is highly recommended, even in the absence of symptoms, as per guidelines from organizations like the NIDDK.
7. Can celiac disease go away?
No. Celiac disease is a lifelong genetic condition. There is currently no cure, and the only treatment is to maintain a strict gluten-free diet for the rest of your life to keep the disease in remission and prevent complications.
8. What is the “celiac rash” (dermatitis herpetiformis)?
Dermatitis herpetiformis (DH) is a very itchy, blistering skin rash that is a direct manifestation of celiac disease. It is caused by gluten ingestion and typically appears on the elbows, knees and buttocks. A diagnosis of DH is a diagnosis of celiac disease.
9. Can celiac disease cause constipation instead of diarrhea?
Yes. While diarrhea is more common, a significant minority of adults with celiac disease present with chronic constipation as their primary digestive symptom. This atypical presentation can contribute to delays in diagnosis.
10. Does celiac disease cause weight gain or weight loss?
It can cause either. Unexplained weight loss is a classic sign of malabsorption. However, some individuals may be overweight or experience weight gain. After diagnosis and starting a gluten-free diet, some people gain weight as their intestine heals and begins absorbing nutrients properly.
Taking Control of Your Health
Celiac disease is a complex and often misunderstood autoimmune condition.
Its ability to masquerade as dozens of other illnesses, particularly in adults, means that countless individuals are living with unexplained symptoms that profoundly impact their quality of life.
The key takeaways are clear: celiac disease is serious, its presentation is often hidden behind non-digestive signs, a proper medical diagnosis before altering your diet is absolutely essential and the only effective treatment is a strict, lifelong gluten-free diet.
Recognizing the hidden signs—from persistent anemia and fatigue to neurological issues and bone loss—is the first step toward empowerment.
If you have read this article and recognized your own health struggles in these descriptions, the most important action you can take is to advocate for yourself.
If you suspect you have symptoms of celiac disease, schedule an appointment with your healthcare provider to discuss your concerns and ask about getting tested.
Your journey to health may have been long, but a diagnosis can be the turning point.
It provides an answer, a clear path forward, and the opportunity to heal.
We encourage you to share your story, experiences, or questions in the comments below.
Your journey could be the encouragement someone else needs to seek answers.
Reference
[1] Beyond Celiac/Harris Poll Reveals that Most Americans with a Child …
https://www.beyondceliac.org/press-room/beyond-celiac-harris-poll-2024/
[2] https://www.mayoclinic.org/diseases-conditions/celiac-disease/symptoms-causes/syc-20352220
[3] [PDF] Symptoms and Diagnosis of Celiac Disease: A Literature Review
https://rsdjournal.org/rsd/article/download/36384/30402/401589
[4] Incidence of Celiac Disease Steadily Increasing
https://celiac.org/2020/02/20/incidence-of-celiac-disease-steadily-increasing
[5] Celiac Disease: Symptoms, Causes, and Diagnosis | Allergy Insider
[6] [PDF] Celiac Disease Foundation
https://celiac.org/wp-content/uploads/2023/05/FY24-NIH-white-paper-FINAL-2.22.23.pdf
[7] Celiac Disease: Extraintestinal Manifestations and Associated …

