The most common signs you might need a root canal are severe, persistent tooth pain, lingering sensitivity to hot or cold, and swollen gums.
While the phrase “root canal” can cause anxiety, this common procedure is designed to relieve pain and save your natural tooth from extraction.
In fact, according to the American Association of Endodontists (AAE), more than 15 million root canals are performed every year, helping millions of people preserve their smiles.
Understanding the warning signs is the first step toward getting the right treatment and stopping the pain for good.
Ignoring these symptoms won’t make them disappear, an infected tooth cannot heal on its own.
This comprehensive guide will walk you through the seven key signs that indicate a root canal may be necessary.
We’ll explore what a root canal actually is, how a dentist confirms the diagnosis, what the procedure involves, and what alternatives exist.
Read on to understand your symptoms and empower yourself to make an informed decision about your dental health.
In This Article
What Is a Root Canal and Why Is It Necessary?
Before diving into the symptoms, it’s crucial to understand what a root canal is and why it becomes a necessary treatment.
The term itself refers to the natural cavity within the center of the tooth, but in dentistry, it describes a procedure to treat infection within that space.
A Simple Definition of a Root Canal
A root canal, or endodontic therapy, is a dental procedure that involves removing the infected or inflamed soft tissue from the center of a tooth.
This tissue, called the pulp, is then replaced with a filling and sealing material to prevent further infection and save the tooth.
As the Cleveland Clinic explains, it’s a restorative procedure designed to clear the infection and preserve the natural tooth structure.
Understanding the Tooth’s Anatomy: Pulp, Canals and Nerves
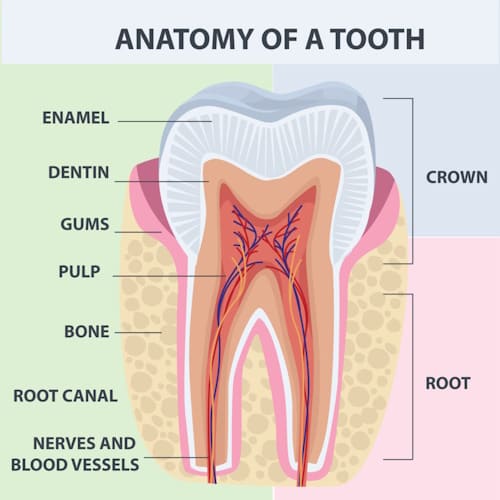
To grasp why a root canal is needed, let’s look inside a tooth:
- Enamel: The hard, white outer layer you see.
- Dentin: A layer of hard tissue beneath the enamel.
- Pulp Chamber: The soft center of the tooth, containing the dental pulp. The pulp is a collection of nerves, blood vessels, and connective tissue. It’s vital during a tooth’s growth and development.
- Root Canals: These are the pathways that extend from the bottom of the pulp chamber down to the tip of the tooth’s root, housing the pulp and nerves.
Once a tooth is fully mature, it can survive without the pulp because the surrounding tissues provide nourishment.
This is why removing the infected pulp can save the tooth without compromising its day-to-day function.
From Reversible to Irreversible Pulpitis: The Point of No Return
Pulp damage doesn’t happen overnight. It typically begins with inflammation, a condition known as pulpitis.
This condition is a direct response to threats like deep decay, trauma, or cracks that allow bacteria to get close to the pulp. There are two stages of pulpitis:
- Reversible Pulpitis: This is a mild inflammation of the pulp. It often causes sharp, brief sensitivity to sweets or cold, but the pain disappears quickly once the stimulus is removed. At this stage, if the cause (like a small cavity) is treated, the pulp can heal and return to normal.
- Irreversible Pulpitis: This is when the inflammation becomes severe, and the pulp tissue is damaged beyond repair. The pain is more intense, lingers long after a stimulus is removed, and can occur spontaneously, even waking you up at night. According to a study in the journal Frontiers in Dental Medicine, this progression involves complex immunological processes that eventually lead to tissue death . At this point, a root canal or extraction is the only option. If left untreated, it leads to pulp necrosis (pulp death) and a dental abscess.
The Top 7 Signs You Might Need a Root Canal
If your tooth’s pulp is fighting a losing battle against infection, it will send out clear distress signals. Here are the seven most common signs that you may need a root canal.
Sign 1: Persistent or Severe Tooth Pain
This is the most well-known symptom. While not all toothaches mean you need a root canal, the pain associated with pulp damage has specific characteristics.
What Does This Pain Feel Like?
The pain is often more than a minor ache. Patients describe it as:
- Spontaneous: It can start without any trigger.
- Throbbing or Pulsating: A rhythmic, intense pain that feels like a heartbeat in your tooth.
- Constant and Severe: The pain doesn’t go away and can be strong enough to disrupt your sleep and daily activities.
Why It Hurts: The Role of Inflammation and Infection
When bacteria infect the pulp, your body’s immune system responds by sending more blood to the area, causing inflammation and swelling.
However, because the pulp is encased in the hard, unyielding walls of the tooth, this swelling creates immense pressure on the nerves, resulting in severe pain.
This is a key finding discussed in research on dental pulp inflammation .
Pain When Chewing or Applying Pressure
If your tooth hurts when you bite down or even just touch it, it’s a strong indicator of a problem.
This pain occurs because the infection has spread to the ligaments and bone surrounding the root tip, a condition called apical periodontitis.
The pressure from chewing irritates these already inflamed tissues.
Sign 2: Lingering Sensitivity to Hot or Cold
Many people have sensitive teeth, but the sensitivity associated with irreversible pulpitis is different.
The 30-Second Rule: Differentiating Normal Sensitivity from a Warning Sign
A key diagnostic clue used by endodontists is the duration of the pain. If you drink something cold and the sensitivity vanishes within a few seconds, it’s likely reversible pulpitis or simple dentin hypersensitivity.
However, if the pain lingers for more than 30 seconds after the hot or cold stimulus is gone, it’s a classic sign of irreversible pulpitis and a strong indicator that you need a root canal.
How Damaged Pulp Reacts to Temperature
A healthy pulp can handle temperature changes. But when the pulp is severely inflamed, the nerves become hyper-reactive. Hot liquids or foods can increase the pressure inside the tooth, causing intense pain.
Cold can initially provide relief by constricting blood vessels, but the pain often returns with a vengeance as the tooth warms up again.
Sign 3: Swollen or Tender Gums
Infection inside a tooth doesn’t always stay contained. It can spread to the surrounding tissues, causing visible symptoms on your gums.
Identifying Gum Swelling Near a Specific Tooth
You might notice that the gum tissue near the painful tooth is swollen, puffy, and tender to the touch. The swelling can be localized to one tooth or may appear more widespread.
This is a sign that the infection is trying to find a way out of the bone surrounding the tooth’s root.
What Causes the Swelling?
The swelling is caused by an accumulation of pus (a thick fluid containing dead white blood cells, tissue debris and bacteria) from the infection at the root tip. Your body is trying to wall off the infection, creating an abscess.
Sign 4: A Pimple on the Gums (Gum Boil or Abscess)
This symptom is a definitive sign of infection that requires immediate dental attention.
What Is That “Pimple”?
That small, pimple-like bump on your gum is called a gum boil, parulis or draining sinus tract.
It’s essentially a tunnel that the infection has created from the abscess at the root tip through the bone and gum tissue to drain the pus.
According to the Mayo Clinic, this is a clear sign of a periapical (root tip) abscess.
Why It Might Not Hurt
Interestingly, the formation of this drainage tract can sometimes relieve the pressure inside the tooth, causing the intense throbbing pain to subside. This can be misleading, making you think the problem has resolved.
However, the infection is still active and will continue to cause bone damage until treated with a root canal.
Sign 5: Tooth Discoloration
A tooth that changes color and appears darker than its neighbors can be a sign of internal damage.
From Healthy White to Gray or Black
When the pulp inside a tooth dies due to trauma or infection, the breakdown of blood cells and other tissues can release pigments that seep into the porous dentin layer.
This internal staining can cause the tooth to turn a grayish, brownish or even blackish color. While external stains from coffee or tea can be polished off, this internal discoloration cannot.
Is Discoloration Always a Sign of a Dead Nerve?
Not always, but it is a significant red flag. A single dark tooth, especially after an injury, strongly suggests that the pulp has suffered trauma and may be necrotic (dead).
A dentist will need to perform tests to confirm the pulp’s status, but discoloration is a strong visual clue that a root canal may be in the future.
Sign 6: A Chipped or Cracked Tooth
A deep crack or chip in a tooth is like an open door for bacteria to invade the pulp.
How Cracks Lead to Infection
Even a microscopic crack can be large enough for bacteria from your saliva to penetrate the enamel and dentin and reach the pulp chamber.
Once inside, they can cause inflammation and infection. According to the Cleveland Clinic, untreated cracked teeth are a common cause of pulp infection and can lead to the need for a root canal.
Symptoms of a Cracked Tooth
Symptoms can be erratic. You might feel a sharp pain when you bite down and then again upon releasing the bite. You may also experience sensitivity to temperatures or sweets.
If a crack is deep enough to involve the pulp, you will likely develop the persistent pain and sensitivity described in the signs above.
Sign 7: Deep Decay or a Large Filling
A history of extensive dental work on a tooth or a very deep cavity increases its risk for pulp problems.
When a Cavity Reaches the Pulp
A dental cavity is tooth decay caused by bacteria. If left untreated, the decay will progress through the enamel and dentin until it reaches the pulp chamber.
This direct exposure of the pulp to bacteria will inevitably lead to infection and the need for a root canal.
The Risk from Multiple Procedures
Even if a tooth has been filled, repeated dental procedures (like replacing a large filling multiple times) can cause stress and trauma to the pulp over time.
Each procedure can bring the pulp closer to inflammation, eventually leading to irreversible damage.
This is why a tooth with a large, old filling might suddenly start to hurt and require endodontic treatment.
Are You Experiencing These Symptoms?
If any of these seven signs sound familiar, don’t wait for the pain to become unbearable. An infected tooth will not heal on its own. Contact your dentist for an evaluation to determine if a root canal is the right treatment to save your tooth and relieve your pain.
How Does a Dentist Confirm You Need a Root Canal?
A diagnosis is never based on symptoms alone. Your dentist or an endodontist (a root canal specialist) will perform a series of tests to confirm the health of your tooth’s pulp and determine the best course of action.
The Diagnostic Process
- Visual Examination and History: The dentist will ask about your symptoms (type of pain, duration, triggers) and visually inspect the tooth and surrounding gums for swelling, discoloration or cracks.
- Dental X-rays: An X-ray is essential. It allows the dentist to see the shape of the root canals and look for signs of infection in the surrounding bone. An infection often appears as a dark spot (a radiolucency) at the tip of the root, indicating bone loss from the abscess.
- Percussion Test: The dentist will gently tap on your teeth with a small instrument. A tooth with a damaged pulp is often sensitive to tapping because the inflammation has spread to the surrounding tissues.
- Pulp Vitality Testing (Cold Test): A cold stimulus (like a small, frozen cotton pellet) is applied to the tooth. As mentioned earlier, the reaction helps differentiate between a healthy tooth, reversible pulpitis and irreversible pulpitis. A healthy tooth feels the cold but it goes away quickly. A tooth with irreversible pulpitis will have a lingering, intense pain. A necrotic (dead) tooth will not feel the cold at all.
What Happens During a Root Canal Procedure?
Thanks to modern anesthetics and techniques, a root canal is typically no more uncomfortable than getting a regular filling. The goal is to remove the source of the pain—the infected pulp.
A Step-by-Step Guide
The procedure, as detailed in the provided file from Healthline, generally follows these four steps:
- Step 1: Anesthetic and Preparation: The dentist numbs the tooth and surrounding area with a local anesthetic. A small protective sheet called a “dental dam” is placed over the area to isolate the tooth and keep it clean and dry during the procedure.
- Step 2: Accessing and Removing the Pulp: A small opening is made in the crown of the tooth to access the pulp chamber. The dentist then uses very small instruments, called files, to carefully remove the diseased pulp from the pulp chamber and root canals.
- Step 3: Cleaning, Shaping, and Disinfecting: Once the pulp is removed, the inside of the tooth is meticulously cleaned, shaped and disinfected with special irrigating solutions to wash away any remaining bacteria. The dentist may place an antibiotic inside the tooth to kill any lingering infection.
- Step 4: Filling and Sealing the Canals: The cleaned and disinfected canals are filled with a biocompatible, rubber-like material called gutta-percha. It is placed with an adhesive cement to ensure the canals are completely sealed, preventing bacteria from re-entering. A temporary filling is then placed to close the opening in the tooth.
After the root canal is complete, you will need to return to your dentist to have a permanent restoration, usually a crown, placed on the tooth. A crown is crucial because a tooth that has had a root canal can become brittle and is more prone to fracture.
Are There Alternatives to a Root Canal?
While a root canal is the standard treatment for saving a tooth with irreversible pulpitis, there are other options to consider, depending on the specific situation.
| Treatment | Description | Best For | Pros | Cons |
|---|---|---|---|---|
| Root Canal Therapy | Removes infected pulp, cleans, and seals the tooth. | Irreversible pulpitis or necrotic pulp in a salvageable tooth. | Saves the natural tooth; maintains normal biting and chewing function. | Requires a crown; can be costly. |
| Tooth Extraction | Complete removal of the affected tooth. | Severely fractured or decayed teeth that cannot be restored. | Removes the source of infection completely; can be less expensive initially. | Loss of natural tooth; requires replacement (implant, bridge) which is costly and invasive; can cause adjacent teeth to shift. |
| Pulp Capping | A medicated material is placed directly over a small pulp exposure to encourage healing. | Minimal pulp exposure from trauma or decay in a tooth with reversible pulpitis. | Less invasive than a root canal; preserves pulp vitality. | Not suitable for infected pulp; success is not guaranteed. |
| Pulpotomy | Removal of the coronal (crown) portion of the pulp, leaving the root pulp intact. | Primarily used on baby teeth, but sometimes on permanent teeth with pulp exposure and no root inflammation. | Less invasive than a full root canal; preserves some pulp tissue. | Limited application in adult teeth; may not be a permanent solution. |
For most cases of irreversible pulpitis, the choice comes down to a root canal versus extraction. The AAE strongly advocates for saving the natural tooth whenever possible, as nothing can fully replace the look, feel, and function of your own tooth.
Recovery, Success Rates and Long-Term Care
After a root canal, your tooth can last a lifetime with proper care.
What to Expect After the Procedure
It’s normal to experience some sensitivity or soreness for a few days after the procedure, especially if there was pain or infection before. This can usually be managed with over-the-counter pain relievers like ibuprofen or acetaminophen.
You should avoid chewing on the treated tooth until it has its permanent restoration.
How Successful Are Root Canals?
Root canal treatment has a very high success rate. Studies show varying rates depending on the criteria, but the outlook is overwhelmingly positive.
A 2023 study published in the Journal of Endodontics followed patients for up to 37 years and found a cumulative tooth survival rate of 97% at 10 years and 76% at 30 years. The study concluded that root canal treatment demonstrates “high longevity in symptomless function”.
Other meta-analyses have reported success rates (defined as healing and absence of disease) between 82% and 93%, making it one of the most predictable procedures in dentistry.
Long-Term Care for Your Treated Tooth
A tooth that has had a root canal and a crown requires the same care as any other tooth:
- Brush at least twice a day with fluoride toothpaste.
- Floss daily to clean between the teeth and under the crown’s margin.
- Visit your dentist for regular check-ups and cleanings.
When Is Tooth Pain a Dental Emergency?
While most toothaches can wait for a scheduled dental appointment, some symptoms indicate a severe, spreading infection that requires immediate medical attention.
Go to an emergency room or seek urgent dental care if your tooth pain is accompanied by:
- High fever
- Facial swelling that is spreading to your cheek, eye or neck
- Difficulty breathing or swallowing
- Uncontrolled bleeding
These are signs that the infection may have spread beyond the tooth, a condition that can be life-threatening.
An ER can provide antibiotics and pain relief to manage the acute situation, but you will still need to see a dentist to treat the source of the problem.
Frequently Asked Questions (FAQ)
1. Is a root canal painful?
No, a root canal procedure itself is not painful. Dentists use effective local anesthesia to completely numb the tooth and surrounding area. The procedure is designed to relieve the severe pain caused by the infection, not cause more of it.
2. How long does a root canal take?
Most root canal procedures can be completed in one or two appointments, each lasting about 60 to 90 minutes. The number of visits depends on the complexity of the tooth’s canal system and the extent of the infection.
3. What is the cost of a root canal?
The cost varies widely depending on the tooth’s location (molars are more expensive) and your geographic area. It is generally more expensive than an extraction but less expensive than replacing a tooth with a dental implant or bridge.
4. Do I need a crown after a root canal?
In most cases, yes. A tooth becomes more brittle after a root canal and is prone to fracture. A crown protects the tooth, restores its strength, and allows it to function normally for years to come.
5. Can an infected tooth heal on its own?
No. Once the pulp is irreversibly inflamed or necrotic, it cannot heal itself. The infection will persist and worsen, leading to bone loss and potentially spreading to other parts of the body if left untreated by a dentist.
6. What happens if I don’t get a root canal?
If you don’t get a root canal, the infection will continue to spread. This will cause more pain, lead to a dental abscess, destroy the bone around your tooth, and eventually require the tooth to be extracted.
7. Can a tooth hurt after a root canal?
It’s normal to have some mild soreness or sensitivity for a few days after the procedure. However, if you experience severe or throbbing pain, you should contact your dentist, as it could be a sign of a complication.
8. What is an endodontist?
An endodontist is a dental specialist with at least two additional years of training beyond dental school. They specialize in diagnosing tooth pain and performing root canal treatment and other procedures relating to the interior of the tooth.
Conclusion
Recognizing the signs you might need a root canal—from persistent pain and lingering sensitivity to a pimple on your gum—is the first and most important step toward preserving your dental health.
While the idea of the procedure can be intimidating, a root canal is a routine, pain-relieving treatment with an excellent track record of success.
Ignoring the symptoms will only lead to more severe pain, bone loss and the eventual loss of your tooth. By seeking timely care, you can stop the infection, eliminate the pain, and keep your natural smile intact for a lifetime.
If you are experiencing any of the seven signs discussed in this article, the best course of action is to consult your dentist.
We hope this guide has empowered you with the knowledge to understand your symptoms. If you found this information helpful, please consider sharing it with others who might be experiencing similar dental issues.
Do you have a personal experience with a root canal? Share your story in the comments below!

