Psoriasis is a chronic, long-term skin disease that causes a rash with itchy, scaly patches. It occurs when the immune system becomes overactive, causing skin cells to multiply up to 10 times faster than normal.
This rapid cell turnover leads to a buildup of cells on the skin’s surface, forming the raised, scaly plaques characteristic of the condition.
While it most commonly appears on the knees, elbows, trunk, and scalp, psoriasis can affect any part of the body.
An impactful fact from the Mayo Clinic is that about a third of all cases begin in childhood, highlighting that this is not just a condition affecting adults. Psoriasis is not contagious.
This comprehensive guide will walk you through everything you need to know about psoriasis, from its various types and symptoms to its underlying causes, triggers, diagnosis, and the most effective treatment strategies available today.
Understanding this condition is the first step toward managing it effectively and improving your quality of life.
In This Article
What is Psoriasis and What Causes It?
Understanding psoriasis begins with knowing it’s more than just a skin condition.
It is a chronic autoimmune disease, meaning it stems from a problem with the body’s own immune system.
While its exact cause isn’t fully understood, researchers have identified key factors that contribute to its development.
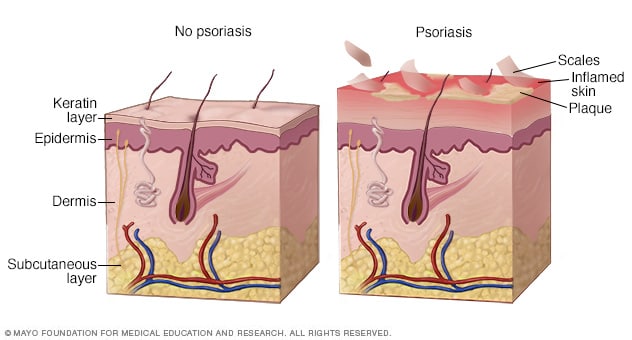
A Deeper Look at the Disease Process
In a person without psoriasis, skin cells grow deep in the skin and slowly rise to the surface, a process that takes about a month.
Once they reach the surface, they die and flake off. In someone with psoriasis, this entire process is dramatically accelerated.
As described by the Mayo Clinic, the life cycle of skin cells greatly speeds up, causing them to build up rapidly on the surface of the epidermis.
This leads to the formation of thick, scaly patches known as plaques.
The Immune System’s Mistake
At its core, psoriasis is thought to be an immune system problem where infection-fighting cells, specifically T-cells, mistakenly attack healthy skin cells.
In a normal immune response, T-cells would identify and attack foreign invaders like bacteria or viruses.
In psoriasis, they trigger an inflammatory response in the skin as if they were fighting an infection or healing a wound.
This misguided attack causes increased production of healthy skin cells, T-cells, and other white blood cells, leading to the cycle of inflammation and rapid cell turnover.
Genetic and Environmental Factors
Researchers believe that both genetics and environmental factors play a crucial role. The condition often runs in families, indicating a strong genetic link.
According to the Mayo Clinic, having one parent with psoriasis increases your risk, and having two parents with the condition increases your risk even more.
However, not everyone with the genetic predisposition will develop psoriasis.
The disease often remains dormant until it is activated by an environmental “trigger”.
This explains why many people may be free of symptoms for years before their first flare-up.
What are the Different Types of Psoriasis?
Psoriasis is not a one-size-fits-all condition. It manifests in several different forms, each with unique characteristics and symptoms.
Identifying the specific type of psoriasis is a critical step for determining the most effective treatment plan.
Plaque Psoriasis (Psoriasis Vulgaris)
This is the most common form of psoriasis, affecting the vast majority of people with the condition.
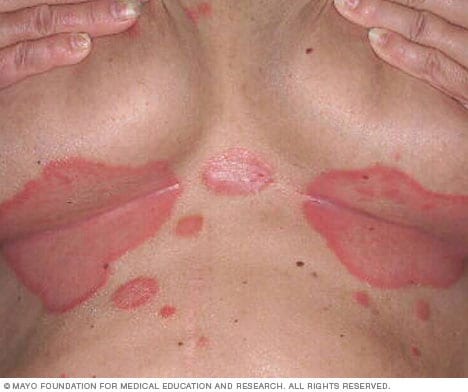
Plaque psoriasis is characterized by dry, itchy, raised skin patches (plaques) covered with silvery-white or grayish scales.
These plaques can be few or many and typically appear on the elbows, knees, lower back, and scalp.
The appearance can vary depending on skin color, on brown or Black skin, the patches may look purplish or darker than the surrounding skin with gray scales, while on white skin, they tend to be pink or red with silver scales.

Plaque psoriasis, the most common type, causes raised, scaly patches on the skin.
Guttate Psoriasis
Guttate psoriasis primarily affects children and young adults. It often appears suddenly and is typically triggered by a bacterial infection, such as strep throat.
This type is marked by small, water-drop-shaped, scaling spots on the trunk, arms, or legs.
The spots are usually not as thick as the plaques in plaque psoriasis but can be widespread across the body.

Guttate psoriasis appears as small, drop-shaped spots, often after an infection.
Inverse Psoriasis
Inverse psoriasis mainly affects skin folds, such as the groin, buttocks, and under the breasts.
It causes smooth, shiny patches of red, inflamed skin that worsen with friction and sweating.
Unlike plaque psoriasis, the affected areas are typically not scaly due to the moist environment of the skin folds.
Fungal infections can sometimes trigger this type of psoriasis.
Inverse psoriasis causes smooth, inflamed patches in skin folds.
Pustular Psoriasis
This is a rare and more severe form of psoriasis characterized by clearly defined, pus-filled blisters (pustules).
These blisters are not infectious and do not contain bacteria. Pustular psoriasis can develop quickly, with the blisters appearing just hours after the skin becomes red and tender.
It can occur in widespread patches across the body or be localized to smaller areas, such as the palms of the hands or the soles of the feet.
Erythrodermic Psoriasis
Erythrodermic psoriasis is the least common but most severe type. It can cover the entire body with a peeling, fiery-red rash that can itch or burn intensely.
This form of psoriasis disrupts the body’s normal chemistry and temperature regulation, which can lead to serious complications like severe illness, pneumonia, or congestive heart failure. It requires immediate medical attention.
Nail Psoriasis
Many people with psoriasis also experience changes in their fingernails and toenails.
Nail psoriasis can cause pitting (small dents in the nail surface), abnormal nail growth, discoloration (yellow-brown spots), and separation of the nail from the nail bed (onycholysis).
In severe cases, the nail may become thick, brittle, and crumble.

Nail psoriasis can cause pitting, discoloration, and abnormal nail growth.
What are the Common Symptoms of Psoriasis?
While symptoms can vary greatly from person to person and depend on the type of psoriasis, there are several common signs to watch for.
The condition is cyclic, meaning symptoms may flare up for a few weeks or months and then subside or even go into complete remission for a time.
Common signs and symptoms of psoriasis include:
- A patchy rash that can range from a few spots of dandruff-like scaling to major eruptions covering large areas of the body.
- Rashes that vary in color, appearing as pink or red with silver scales on white skin, and as shades of purple or dark brown with gray scales on brown or Black skin.
- Dry, cracked skin that may bleed or itch.
- Itching, burning, or soreness in the affected areas. This is a very common and often distressing symptom.
- Thickened, pitted, or ridged nails.
- Swollen and stiff joints, which can be a sign of psoriatic arthritis, a related condition.
When to See a Doctor
If you suspect you have psoriasis, it’s important to see a health care provider for an accurate diagnosis.
You should also seek medical care if your condition:
- Becomes severe or widespread.
- Causes you significant discomfort, pain, or interferes with your sleep and daily activities.
- Leads to concern about the appearance of your skin, affecting your mental well-being.
- Does not improve with over-the-counter products or basic skin care.
- Is accompanied by joint pain, as this could indicate psoriatic arthritis.
What Triggers a Psoriasis Flare-Up?
For individuals with a genetic predisposition to psoriasis, the disease can be activated or worsened by specific environmental factors known as triggers.
Identifying and managing these triggers is a cornerstone of preventing flare-ups.
According to the National Psoriasis Foundation, while there is no known way to prevent the onset of psoriasis, managing triggers can significantly reduce flares.
Common psoriasis triggers include:
- Infections: Both bacterial and viral infections can trigger psoriasis. Strep throat is a well-known trigger for guttate psoriasis, particularly in children. Other skin infections can also lead to a flare.
- Injury to the Skin (Koebner Phenomenon): An injury to the skin, such as a cut, scrape, bug bite, or even a severe sunburn, can trigger a psoriasis flare at the site of the injury. This reaction is known as the Koebner phenomenon.
- Stress: High levels of stress are a major trigger for many people. Because psoriasis is an immune-mediated disease, the impact of stress on the immune system can initiate or worsen a flare.
- Weather: Cold, dry weather can dry out the skin and make psoriasis symptoms worse. Conversely, many people find their symptoms improve in warm, sunny climates with higher humidity.
- Smoking and Alcohol: Smoking tobacco not only increases the risk of developing psoriasis but can also increase its severity and make treatments less effective. Heavy alcohol consumption is also a known trigger and can interfere with treatment efficacy.
- Certain Medications: Some medications are known to trigger psoriasis or worsen existing symptoms. These include lithium (used to treat bipolar disorder), certain high blood pressure drugs (like beta-blockers), antimalarial drugs, and iodides.
- Rapid Withdrawal of Corticosteroids: Abruptly stopping systemic (oral or injected) corticosteroids can cause a severe rebound flare of psoriasis, sometimes in a more aggressive form like pustular or erythrodermic psoriasis.
“Psoriasis is often a lifelong condition. To help their patients live well with psoriasis, dermatologists recommend finding and avoiding your psoriasis triggers.” – American Academy of Dermatology
How is Psoriasis Diagnosed?
A correct diagnosis is the foundation for an effective treatment plan.
Typically, a dermatologist or other health care provider can diagnose psoriasis by examining your skin, scalp, and nails.
The diagnostic process involves considering several key factors.
Factors Considered in Diagnosis
According to the National Psoriasis Foundation, a health care provider will consider the following when making a diagnosis:
- Appearance of the Skin: The provider will look for the characteristic signs of psoriasis, such as thick, raised plaques with well-defined edges and silvery or gray scales.
- Location of the Rash: Psoriasis has a tendency to appear in specific areas, such as the scalp, elbows, knees, and lower back. The location of the lesions provides important clues.
- Patient’s Symptoms: The provider will ask about your symptoms, particularly itching. Itch is a very common and telling symptom of psoriasis. They will also ask about your personal and family medical history.
- Skin Biopsy: In some cases, especially if the diagnosis is uncertain, the provider may perform a skin biopsy. This involves removing a small piece of skin to be examined under a microscope. A biopsy can confirm the diagnosis of psoriasis and rule out other conditions with similar symptoms, such as eczema or a fungal infection.
How is Psoriasis Treated and Managed?
Although there is currently no cure for psoriasis, the field of treatment has advanced dramatically.
Today, there are more effective options than ever before to control symptoms, clear skin, and improve quality of life.
Treating psoriasis is also crucial for lowering the risk of developing related health conditions (comorbidities).
Treatment goals are to stop the skin cells from growing so quickly and to remove scales.
Treatment choice depends on the severity of the psoriasis, the type, its location, and the patient’s overall health and preferences.
Treatment Categories
Treatments generally fall into three main categories, as outlined by the National Psoriasis Foundation:
1. Topical Treatments
These are creams, ointments, lotions, and shampoos applied directly to the skin.
They are usually the first line of defense for mild to moderate psoriasis.
- Topical Corticosteroids: These are anti-inflammatory drugs that are the most frequently prescribed medication for mild to moderate psoriasis. They come in various strengths.
- Topical Non-Steroids: These include vitamin D analogues (like calcipotriene), retinoids (tazarotene), and calcineurin inhibitors (tacrolimus, pimecrolimus), which work by slowing skin cell growth and reducing inflammation.
- Over-the-Counter (OTC) Topicals: Products containing salicylic acid or coal tar can help remove scale and reduce itching and inflammation. Moisturizers are also essential to combat dryness.
2. Phototherapy (Light Therapy)
This treatment uses natural or artificial ultraviolet (UV) light.
The simplest form involves regular, brief exposure to natural sunlight. Other forms are administered in a clinical setting.
- UVB Phototherapy: Controlled doses of ultraviolet B (UVB) light from a special lamp can treat single patches, widespread psoriasis, and psoriasis that resists topical treatments.
- PUVA (Psoralen plus ultraviolet A): This more aggressive treatment combines a light-sensitizing medication (psoralen) with UVA light exposure.
- Excimer Laser: This laser delivers a high-intensity beam of UVB light to a very specific, targeted area of affected skin, sparing healthy surrounding tissue.
3. Systemic Medications
These are prescription drugs that work throughout the body, reserved for moderate to severe psoriasis or cases that are resistant to other treatments. They are administered orally or by injection.
- Oral Treatments: Traditional systemic drugs include methotrexate, cyclosporine, and acitretin. These work by suppressing the overactive immune system. Newer oral treatments like apremilast work by targeting specific molecules inside immune cells.
- Biologics: These are a newer class of protein-based drugs derived from living cells. They target very specific parts of the immune system that are known to fuel the disease process of psoriasis. They are given by injection or intravenous (IV) infusion and have proven highly effective for many with moderate to severe disease.
- Biosimilars: A biosimilar is a biologic medical product that is almost an identical copy of an original biologic drug. They offer a more affordable but equally effective alternative to some of the established biologic treatments.
Complementary and Integrative Medicine (CIM)
Many people find that incorporating CIM into their treatment plan helps manage symptoms.
This can include lifestyle changes (like diet and exercise), natural products (like aloe vera or tea tree oil), and mind-body practices (like meditation and yoga to reduce stress).
It is crucial to talk with your health care provider before adding any CIM to your plan to ensure it is safe and appropriate for you.
What are the Potential Complications of Psoriasis?
The inflammation associated with psoriasis is not just skin-deep.
It is a systemic process that can affect the entire body, increasing the risk of developing other serious health conditions, known as comorbidities.
Treating psoriasis effectively can help lower these risks.
According to sources like the Mayo Clinic and the National Psoriasis Foundation, people with psoriasis are at a greater risk of developing:
| Condition | Description |
|---|---|
| Psoriatic Arthritis (PsA) | An inflammatory arthritis that causes pain, stiffness, and swelling in and around the joints. It can also affect tendons and ligaments. Up to 30% of people with psoriasis develop PsA. |
| Cardiovascular Disease | The chronic inflammation from psoriasis can affect the heart and blood vessels, increasing the risk of heart attack, stroke, and other heart-related problems. |
| Type 2 Diabetes | People with psoriasis, especially severe cases, have a higher risk of developing type 2 diabetes. Inflammation is believed to play a role in insulin resistance. |
| Obesity | Psoriasis is more common and often more severe in people who are obese. Fat cells produce inflammatory proteins that can worsen the condition. |
| Metabolic Syndrome | A cluster of conditions including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels, which collectively increase the risk of heart disease, stroke, and diabetes. |
| Other Autoimmune Diseases | Having psoriasis increases the risk of developing other autoimmune conditions, such as celiac disease, sclerosis, and the inflammatory bowel disease called Crohn’s disease. |
| Eye Conditions | Certain eye problems, such as conjunctivitis, blepharitis, and uveitis (inflammation of the eye’s middle layer), are more common in people with psoriasis. |
| Mental Health Conditions | The physical and emotional burden of living with a visible, chronic disease can lead to low self-esteem, social isolation, anxiety, and a significantly higher risk of depression. |
How Can You Live Well with Psoriasis?
Living with psoriasis is a lifelong journey, but it’s one that can be managed effectively.
Beyond medical treatments, adopting certain lifestyle habits and coping strategies can make a significant difference in your physical and mental well-being.
Dermatologist-Recommended Strategies
The American Academy of Dermatology suggests several key strategies to help patients live well:
- Use Psoriasis-Friendly Skin Care: Keep your skin moisturized. Take daily baths or showers using lukewarm water and mild soaps. After bathing, gently pat your skin dry and apply a heavy, ointment-based moisturizer to trap moisture in.
- Identify and Manage Your Triggers: Keep a journal to track your symptoms and identify what might be causing your flares. Once you know your triggers (e.g., stress, certain foods, lack of sleep), you can take steps to avoid or manage them.
- Adhere to Your Treatment Plan: Treat your psoriasis as prescribed by your dermatologist. Consistency is key to keeping symptoms under control.
- Communicate with Your Doctor: Be open with your dermatologist about all your symptoms, even if they seem unrelated to your skin, such as joint pain or feeling down. This helps them see the full picture and manage your overall health.
Lifestyle and Home Remedies
- Eat a Healthy Diet: While no diet can cure psoriasis, many people find that an anti-inflammatory diet rich in fruits, vegetables, lean proteins, and healthy fats can help reduce symptoms.
- Maintain a Healthy Weight: Losing excess weight can reduce the severity of psoriasis and make treatments more effective.
- Exercise Regularly: Exercise is a great way to reduce stress, maintain a healthy weight, and lower your risk of cardiovascular disease.
- Limit Alcohol and Quit Smoking: Both are known to worsen psoriasis and can interfere with treatments.
Frequently Asked Questions (FAQ)
1. Is psoriasis contagious?
No, psoriasis is not contagious. It is an autoimmune disease, not an infection. You cannot catch it from or give it to another person by touching their skin, swimming in the same pool, or through any other form of contact.
2. Is there a cure for psoriasis?
Currently, there is no cure for psoriasis. However, there are many highly effective treatments that can control symptoms, clear the skin for long periods, and reduce the risk of related health conditions. Research for new treatments and a cure is ongoing.
3. Does diet affect psoriasis?
While no specific diet is proven to cure psoriasis, many people report that their symptoms improve by avoiding inflammatory foods (like red meat and processed foods) and eating an anti-inflammatory diet rich in fruits, vegetables, and omega-3 fatty acids.
4. Can stress cause psoriasis?
Stress doesn’t cause psoriasis, but it is one of the most common triggers for a flare-up in people who already have the condition. Managing stress through techniques like meditation, yoga, or exercise can help prevent flares.
5. What is the difference between psoriasis and eczema?
Psoriasis typically causes well-defined, thick, red, scaly patches, and the itch is often described as a burning or stinging sensation. Eczema often presents as less-defined patches and causes a more intense, persistent itch. A dermatologist can provide a definitive diagnosis.
6. Can psoriasis go away on its own?
Psoriasis is a chronic condition with a cyclical nature. Symptoms may subside and go into remission for a period, making it seem like it has gone away. However, it can flare up again later, often due to a trigger.
7. What is psoriatic arthritis?
Psoriatic arthritis (PsA) is a form of inflammatory arthritis that affects some people with psoriasis. It causes joint pain, stiffness, and swelling. Early diagnosis and treatment are crucial to prevent permanent joint damage.
8. Can I get psoriasis as an adult?
Yes. While about a third of cases begin in childhood, psoriasis can develop at any age. It is common for the first onset to occur in two age peaks: between 20-30 years old and between 50-60 years old.
Conclusion
Psoriasis is a complex, chronic autoimmune disease that extends beyond the skin, impacting overall health and quality of life.
While the journey can be challenging, significant advancements in medicine have provided a powerful arsenal of treatments—from topicals and phototherapy to groundbreaking systemic and biologic drugs—that can effectively manage symptoms and reduce the risk of comorbidities.
Understanding the nature of the disease, identifying personal triggers, and adopting a healthy lifestyle are equally vital components of a comprehensive management plan.
If you have or suspect you have psoriasis, the most important step is to partner with a health care provider.
Together, you can create a personalized treatment strategy that not only clears your skin but also supports your long-term physical and mental well-being.
You are not alone in this journey, and with the right knowledge and support, you can live a full and active life.
We hope this guide has empowered you with the knowledge to better understand and manage psoriasis.
If you found this information helpful, please consider sharing it with others who may benefit.
Do you have an experience with psoriasis you’d like to share? Leave a comment below.

