Maintaining prostate health is a cornerstone of a man’s overall well-being, particularly as he ages.
Understanding its function, recognizing potential problems, and adopting preventive measures can significantly impact quality of life.
With the American Cancer Society estimating about 313,780 new cases of prostate cancer in the US for 2025, awareness has never been more critical.
This comprehensive guide delves into the essential aspects of prostate health, from the early signs of common conditions like BPH and prostatitis to evidence-based strategies for prevention and the latest in screening protocols.
Our goal is to empower you with the knowledge to make informed decisions alongside your healthcare provider.
In This Article
Understanding the Prostate Gland
Before diving into potential problems, it’s essential to understand what the prostate is and its vital functions within the male body.
This small gland plays a surprisingly large role in both the urinary and reproductive systems.
Anatomy and Location
The prostate is a small, soft gland, typically about the size and shape of a walnut.
It is strategically located deep within the pelvis, positioned just below the bladder and in front of the rectum.
A key anatomical feature is that it wraps around the urethra, the tube that carries urine from the bladder out of the body.
This specific location is why an enlarged or inflamed prostate often leads to noticeable urinary symptoms.
The Prostate’s Role in Reproduction and Urination
The prostate gland has two primary functions. Its main role is reproductive: it produces a milky, alkaline fluid that constitutes a significant portion of semen.
This fluid is crucial for nourishing and protecting sperm, enhancing their motility and viability, thereby increasing the chances of successful fertilization.
During ejaculation, the prostate contracts and releases this fluid into the urethra, where it mixes with sperm from the testicles.
Secondly, through its muscular fibers, the prostate helps control the flow of urine.
Common Prostate Conditions
As men age, the prostate is susceptible to three main conditions. While they share overlapping symptoms, they are distinct diseases with different causes and treatments.
Understanding these differences is the first step toward proper diagnosis and management.
Benign Prostatic Hyperplasia (BPH): The Common Enlargement
Benign Prostatic Hyperplasia, or BPH, is a non-cancerous enlargement of the prostate gland.
It is an extremely common part of aging.
As the gland grows, it can squeeze or “pinch” the urethra, leading to a range of urinary difficulties known as Lower Urinary Tract Symptoms (LUTS).
According to Yale Medicine, about 50% of men between 51 and 60 have BPH, a figure that rises to around 80% for men over 70.
It’s important to remember that BPH is not cancer and does not increase your risk of developing prostate cancer.
Prostatitis: Inflammation and Pain
Prostatitis refers to the inflammation or swelling of the prostate gland, and it can affect men of all ages.
It’s often accompanied by pain in the groin, pelvic area, or genitals, and can cause urinary symptoms and painful ejaculation.
There are several types:
- Acute Bacterial Prostatitis: A sudden bacterial infection causing fever, chills, and severe pain. It requires immediate medical attention.
- Chronic Bacterial Prostatitis: A recurring bacterial infection that can be more difficult to treat.
- Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS): The most common type, where no evidence of bacteria is found. The cause is often unknown but can be related to stress, nerve damage, or a previous infection.
Prostate Cancer: The Silent Threat
Prostate cancer occurs when cells in the prostate gland begin to grow out of control.
It is the second most common cancer in American men, after skin cancer.
A concerning aspect of prostate cancer is that in its early stages, it often presents no symptoms at all.
When symptoms do appear, they can be similar to those of BPH, such as trouble urinating.
This is why screening and regular check-ups are so vital.
Fortunately, as noted by the Mayo Clinic, many prostate cancers grow slowly and may not require immediate treatment, but early detection is key to having the most treatment options available.
Recognizing the Warning Signs
Being attuned to your body’s signals is crucial for early detection.
While many of these symptoms can be caused by non-cancerous conditions like BPH, they should never be ignored.
Here are the key signs of prostate problems to watch for.
Urinary Symptoms: Changes in Flow and Frequency
Because the prostate surrounds the urethra, any swelling or growth directly impacts urination.
These are often the first and most common signs of a prostate issue:
- A frequent or urgent need to urinate, especially at night (nocturia).
- Difficulty starting urination or a weak, slow, or interrupted urine stream.
- Dribbling at the end of urination.
- A feeling that the bladder has not fully emptied.
- Pain or a burning sensation during urination.
Pain and Discomfort: Where and When
Pain is a less common symptom for BPH and early prostate cancer but is a hallmark of prostatitis.
It can also indicate more advanced prostate cancer. Pay attention to:
- Pain or stiffness in the lower back, hips, pelvis, or rectal area.
- Pain in the area between the scrotum and rectum (perineum).
- Pain or discomfort during or after ejaculation.
Sexual Health Indicators
Prostate health is intrinsically linked to sexual function.
While erectile dysfunction (ED) has many causes, new or worsening ED can sometimes be related to a prostate condition.
Another significant, though less common, symptom is the presence of blood in the urine (hematuria) or semen (hematospermia).
Any instance of this warrants an immediate visit to your doctor.
When to See a Doctor
Any new or persistent urinary, sexual, or pain-related symptoms should be evaluated by a healthcare professional. Self-diagnosis is unreliable and can be dangerous, as the symptoms for BPH, prostatitis, and prostate cancer can overlap significantly. An inability to urinate is a medical emergency and requires immediate care.
A doctor can perform the necessary tests to determine the underlying cause and recommend the appropriate course of action, providing peace of mind and ensuring timely treatment if needed.
Proactive Prevention
While factors like age and genetics are beyond our control, a growing body of evidence shows that lifestyle choices can play a significant role in promoting good prostate health and potentially lowering the risk of developing problems.
The Power of a Prostate-Friendly Diet
Instead of focusing on single “miracle” foods, experts recommend adopting an overall healthy eating pattern.
A diet rich in fruits, vegetables, and healthy fats can have a protective effect.
Research from institutions like Harvard Health suggests the following dietary strategies:
- Eat more fruits and vegetables: Aim for at least five servings a day. Vegetables like broccoli and cauliflower (cruciferous vegetables) and fruits rich in lycopene, such as tomatoes and watermelon, are particularly beneficial.
- Choose healthy fats: Limit saturated fats from red meat and dairy. Instead, opt for healthy fats found in avocados, nuts, and olive oil. Omega-3 fatty acids, found in fish like salmon and sardines, may also reduce inflammation.
- Limit red and processed meats: High consumption of red meat (beef, pork, lamb) and processed meats has been linked to an increased risk of prostate cancer.
- Drink green tea: Some studies suggest that compounds in green tea may help lower the risk of prostate cancer.
The Undeniable Benefits of Regular Exercise
Physical activity is a powerful tool for overall health and has specific benefits for the prostate.
A large-scale study, the Health Professionals Follow-up Study, found that men who were more physically active were less likely to suffer from BPH.
Even moderate activity like brisk walking for 3 hours per week showed significant benefits.
A 2023 review published in Prostate Cancer and Prostatic Diseases confirmed that physical activity can improve outcomes and mental health in patients. Exercise helps by:
- Reducing inflammation: Regular activity can lower levels of systemic inflammation, a factor linked to both BPH and prostate cancer.
- Maintaining a healthy weight: Exercise is crucial for weight management, which is a key risk factor.
- Improving hormonal balance: Physical activity can help regulate hormones that influence prostate growth.
Maintaining a Healthy Weight
Obesity is a significant risk factor for developing more aggressive forms of prostate cancer and can also worsen the symptoms of BPH.
Excess body fat, particularly around the abdomen, promotes a state of chronic inflammation and can disrupt hormone levels, creating an environment where prostate problems are more likely to develop and progress.
Combining a healthy diet with regular exercise is the most effective strategy for achieving and maintaining a healthy body mass index (BMI).
Screening and Diagnosis
Early detection is the most powerful weapon against serious prostate disease.
Modern diagnostics involve a combination of blood tests, physical exams, and advanced imaging, guided by a principle of shared decision-making between the patient and doctor.
The Role of the PSA Test
The prostate-specific antigen (PSA) test is a blood test that measures the level of PSA, a protein produced by the prostate gland.
While elevated PSA can be a sign of prostate cancer, it is not a definitive diagnosis.
Other conditions, such as BPH and prostatitis, can also cause PSA levels to rise.
Current guidelines from organizations like the U.S. Preventive Services Task Force (USPSTF) recommend that men aged 55 to 69 make an individual decision about screening after discussing the potential benefits and harms with their doctor.
Routine screening is generally not recommended for men over 70.
This shared decision-making approach helps avoid over-diagnosis and over-treatment of slow-growing cancers that may never cause harm.
The Digital Rectal Exam (DRE)
During a digital rectal exam (DRE), a doctor inserts a gloved, lubricated finger into the rectum to feel the prostate gland.
This allows the doctor to check for abnormalities in its size, shape, and texture, such as hard lumps or nodules that could indicate cancer.
While the PSA test measures a blood marker, the DRE provides a physical assessment of the gland itself.
It is often performed alongside a PSA test as part of a comprehensive prostate health check-up.
Advanced Diagnostics
If initial tests like the PSA or DRE are abnormal, a doctor may recommend further investigation to get a clearer picture.
These can include:
- Transrectal Ultrasound (TRUS): Uses sound waves to create an image of the prostate.
- Magnetic Resonance Imaging (MRI): A more detailed imaging test that can help identify suspicious areas within the prostate, often used to guide a biopsy.
- Biopsy: The only way to definitively diagnose prostate cancer. During a biopsy, small samples of prostate tissue are removed with a needle and examined under a microscope for cancer cells.
Prostate Health by the Numbers
Visualizing the data helps to contextualize the prevalence and impact of prostate conditions.
The following charts and table provide a snapshot of the current landscape.
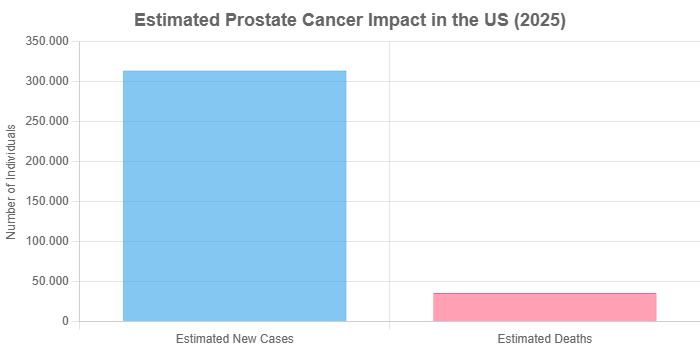
Data Source: American Cancer Society, 2025 Estimates
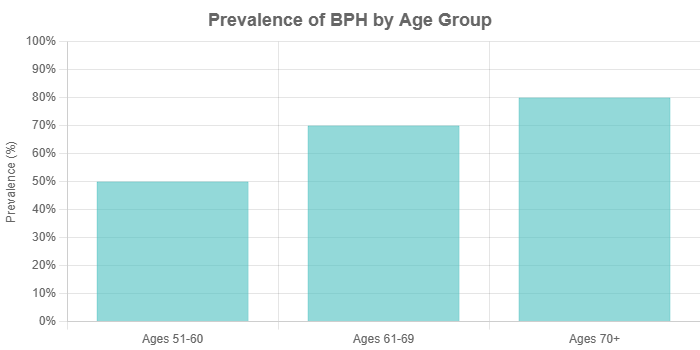
Data Source: Yale Medicine
Table: Comparing Common Prostate Conditions
| Feature | Benign Prostatic Hyperplasia (BPH) | Prostatitis | Prostate Cancer |
|---|---|---|---|
| Nature of Condition | Non-cancerous enlargement of the prostate. | Inflammation or infection of the prostate. | Malignant (cancerous) growth of cells. |
| Common Symptoms | Weak urine stream, frequent urination, nocturia, incomplete emptying. | Pelvic pain, painful urination/ejaculation, fever (in acute cases). | Often no symptoms in early stages, later can mimic BPH symptoms. |
| Primary Cause | Aging and hormonal changes. | Bacterial infection or unknown inflammatory causes. | Genetic mutations leading to uncontrolled cell growth. |
| Typical Age Group | Most common in men over 50. | Can affect men of all ages. | Risk increases significantly after age 50, average diagnosis at 67. |
| Cancer Risk | Does not increase cancer risk. | No direct link, but chronic inflammation is a risk factor for cancer in general. | Is cancer. Can be slow-growing or aggressive. |
Your Prostate Health Questions Answered
Here are concise answers to some of the most frequently asked questions about prostate health.
1. Does frequent ejaculation help the prostate?
Some studies have suggested a correlation between higher ejaculation frequency and a lower risk of prostate cancer, but the evidence is not definitive. It is not considered a primary prevention strategy.
2. Can supplements like saw palmetto improve prostate health?
While popular for BPH symptoms, large-scale clinical trials have generally shown that saw palmetto is no more effective than a placebo. Always consult your doctor before taking any supplements.
3. Is prostate cancer always slow-growing?
No. While many prostate cancers are indolent (slow-growing) and may not require immediate treatment, some forms are aggressive and can spread quickly. A biopsy and Gleason score help determine the cancer’s aggressiveness.
4. What is a “normal” PSA level?
There is no single “normal” PSA level. What’s normal varies with age, prostate size, and other factors. Doctors look more at the trend of PSA levels over time (PSA velocity) rather than a single number.
5. Can I prevent BPH completely?
Since BPH is largely tied to aging, it cannot be completely prevented. However, a healthy lifestyle, including diet, exercise, and weight management, may help manage symptoms and slow its progression.
6. Does having BPH increase my risk of prostate cancer?
No. BPH and prostate cancer are separate conditions that can coexist. Having an enlarged prostate does not increase your risk of developing prostate cancer.
7. What is the Gleason score?
The Gleason score is a grading system used to determine the aggressiveness of prostate cancer found on a biopsy. Scores range from 6 (low-grade) to 10 (high-grade), helping guide treatment decisions.
8. How often should I get a prostate exam?
This should be a personalized decision made with your doctor, based on your age, risk factors (like family history and race), and personal preferences, typically starting with a discussion around age 50-55.
Conclusion
Prostate health is a journey, not a destination.
It requires ongoing attention, awareness, and a partnership with your healthcare provider.
By understanding the function of the prostate, recognizing the early warning signs of potential issues, and embracing a proactive lifestyle, you can significantly improve your odds of maintaining a healthy prostate long into the future.
Remember that knowledge is power.
The key takeaways are simple but profound: listen to your body, adopt a healthy diet and exercise routine, and engage in open, informed discussions with your doctor about screening.
Don’t hesitate to seek medical advice for any concerns—early detection and action are your best allies.

