Periodontitis is a serious gum infection that progresses through four distinct stages, potentially leading to tooth and bone loss if left untreated.
This condition is far more common than many realize. According to the Centers for Disease Control and Prevention (CDC), an alarming 47.2% of adults aged 30 years and older have some form of periodontal disease.
This advanced form of gum disease doesn’t just harm your mouth, the bacteria responsible can enter your bloodstream and contribute to other serious health issues, including heart and respiratory diseases.
Understanding the progression of this silent disease is the first and most critical step toward prevention and successful treatment.
This comprehensive guide will walk you through each of the 4 stages of periodontitis, detailing the symptoms to watch for, the underlying causes, and the most effective treatments available to protect your oral and overall health.
Continue reading to empower yourself with the knowledge to fight back against gum disease.
In This Article
What is Periodontitis and Why Does it Matter?
Periodontitis, often called gum disease, is a severe infection of the gums that damages the soft tissue and, without treatment, can destroy the bone that supports your teeth.
The name itself, periodontitis (per-e-o-don-TIE-tis), breaks down into “peri” (around), “odont” (tooth), and “itis” (inflammation). It is, quite literally, inflammation around the tooth.
This condition begins with a sticky, bacteria-laden film called plaque. If not removed daily, plaque hardens into tartar, which irritates the gums and causes a mild, reversible form of gum disease called gingivitis.
However, if this inflammation is allowed to persist, it progresses into periodontitis. The gums begin to pull away from the teeth, forming spaces called “pockets”.
These pockets become infected, and as the disease advances, they deepen, leading to the destruction of gum tissue and bone.
Ultimately, this can cause teeth to loosen and either fall out or require extraction.
Why does this matter beyond losing a tooth? The implications of untreated periodontitis extend far beyond your mouth.
The chronic inflammation puts a strain on your immune system, and the bacteria from the infected gums can enter your bloodstream.
Research has established strong links between periodontitis and a host of systemic health problems, including:
- Coronary artery disease
- Respiratory disease
- Rheumatoid arthritis
- Problems controlling blood sugar in diabetes
- Complications during pregnancy, such as preterm birth and low birth weight
Therefore, treating periodontitis is not just about saving your teeth—it’s about protecting your overall health and well-being.
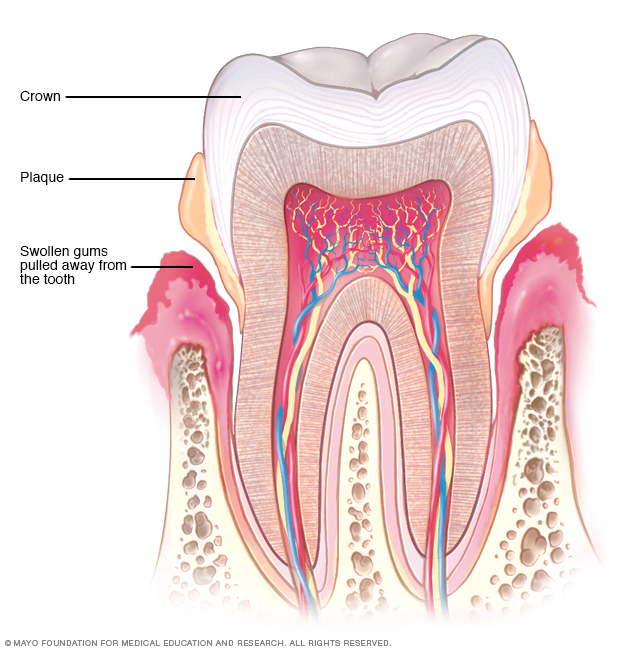
An illustration showing how plaque buildup leads to swollen, receding gums—a hallmark of periodontitis.
The 4 Stages of Periodontitis: A Detailed Breakdown
Periodontitis doesn’t appear overnight. It’s a progressive disease that worsens over time if not addressed.
Understanding its stages is crucial for recognizing the signs early and seeking timely treatment.
The progression is generally classified into four stages, starting with its precursor, gingivitis.
Stage 1: Gingivitis (Inflammation)
Gingivitis is the earliest and only reversible stage of gum disease. It is characterized by inflammation of the gingiva (the part of the gum around the base of your teeth).
At this stage, the infection has not yet reached the bone, and no irreversible damage has occurred.
- Key Signs: The most common sign is gums that bleed easily when you brush or floss. You might see a pinkish tint on your toothbrush or in the sink. Gums may also appear red and swollen or puffy, and you might experience persistent bad breath.
- Cause: Gingivitis is caused by the accumulation of plaque along the gumline. If you don’t brush and floss effectively, this bacterial film irritates the gum tissue, triggering an inflammatory response from your immune system.
- Pocket Depth: In a healthy mouth, the small groove between the gum and tooth (sulcus) measures 1-3 millimeters. In gingivitis, this depth may remain the same, but inflammation is present.
- Reversibility: The good news is that gingivitis can typically be reversed with a professional dental cleaning and a consistent, thorough home care routine of brushing and flossing.
Stage 2: Early Periodontitis
If gingivitis is left untreated, the inflammation progresses and the disease enters its second stage: early periodontitis.
At this point, the damage becomes irreversible, as the infection starts to destroy the bone that supports the teeth.
- Key Signs: The inflammation becomes more pronounced. Gums may start to pull away, or recede, from the teeth. This creates small pockets between the teeth and gums. These pockets trap plaque and food debris, making them impossible to clean with a regular toothbrush. Bleeding during brushing and flossing is more consistent.
- Pocket Depth: The pockets deepen to 4-5 millimeters. This is a clear diagnostic sign that the disease has progressed beyond gingivitis.
- Damage: Your immune system continues to fight the bacteria, but the toxins produced by the bacteria, combined with the body’s own inflammatory response, begin to break down the connective tissue and bone that hold your teeth in place. This is the beginning of bone loss.
- Treatment: While the bone loss is not reversible, the disease’s progression can be halted with non-surgical treatment, typically a deep-cleaning procedure called scaling and root planing.
Stage 3: Moderate Periodontitis
In the third stage, the infection deepens, causing more significant and widespread damage.
The symptoms become more noticeable and can start to affect your daily life.
- Key Signs: You may experience increased gum recession, making your teeth appear longer. The pockets are now deeper, and you might notice pus between your teeth and gums. Teeth may begin to feel slightly loose or shift their position. Pain or tenderness around the gums or when chewing is common, as is persistent and severe bad breath.
- Pocket Depth: Probing depths measure 6-7 millimeters, indicating significant tissue and bone loss.
- Damage: There is moderate bone loss, and the support for the teeth is substantially weakened. The infection can also trigger a more widespread inflammatory response throughout your body, increasing the risk of systemic health problems.
- Treatment: Scaling and root planing is still the first line of defense, but surgical intervention, such as flap surgery, may be required to effectively clean the deep pockets and halt further bone destruction.
Stage 4: Advanced Periodontitis
This is the most severe stage of the disease, with extensive damage to the supporting structures of the teeth.
At this point, tooth loss is a very real and imminent risk.
- Key Signs: The connective tissues that hold the teeth in place are severely deteriorated. The gums, bones, and other tissues are destroyed. You will likely experience severe pain while chewing, major gum recession, significant tooth mobility (very loose teeth), and a foul taste in your mouth.
- Pocket Depth: Pockets are typically deeper than 7 millimeters.
- Damage: Over 50% of the supporting bone has been lost. Teeth may shift dramatically, affecting your bite and ability to eat. Without aggressive treatment, teeth will likely fall out or need to be extracted by a dentist.
- Treatment: Treatment is complex and often involves extensive surgical procedures, such as flap surgery, bone grafting to try and regenerate lost bone, or extractions and replacement with dental implants, bridges, or dentures. The primary goal is to control the infection and save any remaining viable teeth.
What are the Common Symptoms of Periodontitis?
The symptoms of periodontitis vary depending on the stage of the disease, but they often develop slowly and can be subtle in the early stages.
This is why regular dental checkups are so important. If you notice any of the following signs, it’s crucial to see a dentist as soon as possible.
Symptoms Related to Your Gums:
- Swollen, puffy, or tender gums.
- Gums that are bright red, dark red, or even purplish.
- Gums that bleed easily during brushing or flossing (you might see a pink-tinged toothbrush).
- Spitting out blood after brushing.
- Receding gums, which make your teeth look longer than normal.
- Pus appearing between your teeth and gums.
Symptoms Related to Your Teeth:
- Teeth that are loose or shifting in position.
- New spaces or black triangles developing between your teeth.
- Pain or sensitivity when chewing.
- A change in the way your teeth fit together when you bite.
- Tooth loss.
Other General Symptoms:
- Persistent bad breath (halitosis) that doesn’t go away with brushing or mouthwash.
- A foul or unpleasant taste in your mouth.
When to See a Dentist: Healthy gums are firm, fit snugly around the teeth, and don’t bleed. If you notice any of the symptoms listed above, don’t wait. Make an appointment with your dentist immediately. The sooner you get care for periodontitis, the better your chances of reversing the damage or halting its progression.
What Causes Periodontitis to Develop?
In almost all cases, the development of periodontitis starts with plaque.
While our mouths are home to hundreds of types of bacteria, they only become harmful when conditions allow them to multiply dramatically.
This typically happens as a result of poor oral hygiene. Here is the step-by-step progression from a healthy mouth to one with periodontitis:
- Plaque Forms on Your Teeth: When starches and sugars from the food you eat interact with the bacteria naturally present in your mouth, they form a sticky, colorless film called plaque. Plaque constantly forms on your teeth. Brushing twice a day and flossing once a day removes it, but it begins to re-form quickly.
- Plaque Hardens into Tartar (Calculus): If plaque is not removed, it can harden under your gumline into a substance called tartar. Tartar is a mineralized deposit that is much harder and more difficult to remove than plaque. It acts as a rough, porous surface that attracts even more plaque and bacteria.
- Tartar Cannot Be Removed at Home: Once tartar has formed, you cannot get rid of it by brushing and flossing. It requires a professional dental cleaning by a dentist or dental hygienist. The longer tartar and plaque remain on your teeth, the more damage they do.
- Plaque Causes Gingivitis: The bacteria in plaque and tartar produce toxins that irritate the gums, causing inflammation. This initial stage of gum disease is called gingivitis. The gums become red, swollen, and may bleed easily.
- Ongoing Inflammation Causes Periodontitis: If gingivitis is not treated, the persistent inflammation triggers a chronic immune response. This response, meant to fight the infection, starts to break down the tissues and bone that support the teeth. Deep pockets form between the gums and teeth, which fill with more plaque, tartar, and bacteria. These deep infections lead to the loss of tissue and bone, and eventually, tooth loss.
Are You at Risk? Key Risk Factors for Periodontitis
While plaque is the primary cause of periodontitis, certain factors can significantly increase your risk of developing the disease, accelerate its progression, or make treatment less successful. These include:
- Smoking or Chewing Tobacco: This is one of the most significant risk factors for periodontitis. Smoking weakens your immune system’s ability to fight off gum infection and also makes it harder for your gums to heal after being damaged.
- Poor Oral Health Habits: Inconsistent brushing and flossing are the most direct contributors to plaque buildup.
- Gingivitis: Untreated gingivitis will almost always progress to periodontitis.
- Diabetes (especially Type 2): The relationship between diabetes and periodontitis is a two-way street. Periodontitis can make it harder to control blood sugar, and high blood sugar levels can lower the body’s ability to fight infection, making gum disease more severe.
- Hormonal Changes: Changes in hormones during pregnancy, menopause, or menstruation can make gums more sensitive and susceptible to inflammation.
- Genetics: Some individuals are simply more genetically predisposed to developing gum disease.
- Obesity: Research shows a link between obesity and an increased risk of gum disease.
- Conditions that Lower Immunity: Diseases like HIV/AIDS, leukemia, and cancer treatments can compromise the immune system and make infections like periodontitis worse.
- Certain Medications: Some drugs can reduce the flow of saliva (dry mouth), which is protective against plaque. Other medications can cause abnormal gum tissue growth, making them harder to clean.
- Poor Nutrition: A diet lacking in essential nutrients, particularly vitamin C, can impair the body’s ability to heal.
- Recreational Drug Use: Smoking marijuana or vaping can also contribute to gum problems.
How is Periodontitis Diagnosed by a Dentist?
A thorough dental examination is the only way to diagnose periodontitis and determine its stage.
Your dentist or dental hygienist will perform several tests, which are usually painless, to assess the health of your gums and the supporting structures of your teeth.
| Diagnostic Test | How It’s Done | Why It’s Done |
|---|---|---|
| Gum Examination & Probing | The dentist or hygienist will examine your gums for signs of inflammation, such as redness, swelling, and bleeding. They will then use a tiny ruler called a “periodontal probe” to gently measure the depth of the pockets around each tooth. | This is the key test to distinguish gingivitis from periodontitis. In a healthy mouth, pocket depths are 1-3 millimeters. Deeper pockets (4mm or more) are a definitive sign of periodontitis and bone loss. |
| Medical and Dental History Survey | Your dental team will ask you questions about your symptoms, oral hygiene habits, and overall health. It’s crucial to inform them about any medical conditions you have or medications you take. | This helps identify risk factors, such as smoking or diabetes, that can contribute to gum disease and may influence the treatment plan. |
| Dental X-Rays | X-ray images of your teeth and jaw are taken. These can include a full mouth series or specific images of areas of concern. | X-rays are essential for visualizing what cannot be seen with the naked eye. They clearly show the extent of bone loss around the teeth, which is a critical factor in staging the severity of the periodontitis. |
Based on these findings, your dentist can diagnose the presence and stage of periodontitis.
In more advanced or complex cases, they may refer you to a periodontist, a dentist who specializes in the prevention, diagnosis, and treatment of gum disease.
What are the Treatment Options for Periodontitis?
The main goal of periodontitis treatment is to control the infection, halt the progression of the disease, and restore gum health.
The type of treatment will vary depending on the stage of the disease.
All treatment plans require the patient to commit to excellent daily oral care at home to ensure long-term success.
Non-Surgical Treatments (For Early to Moderate Stages)
For gingivitis and early-to-moderate periodontitis, non-surgical approaches are often sufficient.
- Professional Dental Cleaning: For gingivitis, a standard professional cleaning to remove plaque and tartar above and just below the gumline may be all that is needed, along with improved home care.
- Scaling and Root Planing: This is a deep-cleaning, non-surgical procedure and the gold standard for treating periodontitis.
- Scaling: The dentist or hygienist removes all the plaque and tartar from above and below the gumline, cleaning all the way down to the bottom of the pocket.
- Root Planing: The root surfaces of the teeth are smoothed out. This helps prevent bacteria from re-attaching and allows the gums to heal and reattach more firmly to the teeth.
- Antibiotics: In some cases, especially with persistent infections, your dentist may prescribe antibiotics to help control the bacteria. These can be in the form of an oral tablet or capsule, a medicated mouthwash, or a gel or antibiotic chip that is placed directly into the periodontal pocket after deep cleaning.
Surgical Treatments (For Moderate to Advanced Stages)
If deep pockets remain after scaling and root planing, or if there is significant bone loss, surgical treatment may be necessary.
- Flap Surgery (Pocket Reduction Surgery): In this procedure, the periodontist makes tiny incisions in your gum so that a section of gum tissue can be lifted back, exposing the roots for more effective scaling and root planing. After the area is thoroughly cleaned, the gums are sutured back in place, fitting more snugly around the tooth. This reduces the pocket depth, making the area easier to keep clean.
- Bone Grafting: If periodontitis has destroyed the bone surrounding your tooth root, a bone graft may be performed. This involves placing natural or synthetic bone material in the area of bone loss. The graft serves as a scaffold on which your own body can regenerate new bone, which helps to stabilize the tooth. This is often done in conjunction with flap surgery.
- Soft Tissue Grafts: Gum recession can expose the roots of your teeth. To cover the exposed roots and reinforce thin gum tissue, a graft can be taken from the roof of your mouth or another source and stitched into place. This reduces sensitivity and protects the roots from decay.
- Guided Tissue Regeneration (GTR): This procedure stimulates bone and gum tissue growth. Done in combination with flap surgery, a small piece of mesh-like fabric is inserted between the bone and gum tissue. This barrier keeps the gum tissue from growing into the area where bone should be, allowing the bone and connective tissue to regrow and better support the teeth.
The Importance of Ongoing Maintenance
Periodontitis is a chronic disease, meaning it can recur if not properly managed.
After successful treatment, you will need to follow a schedule of regular maintenance appointments (periodontal maintenance), typically every three to four months.
These visits are more in-depth than standard cleanings and are essential for preventing the disease from returning.
How Can You Prevent Periodontitis?
The best way to deal with periodontitis is to prevent it from ever starting.
Prevention is based on a lifelong commitment to good oral hygiene and regular professional care.
- Brush Your Teeth Thoroughly: Brush for two minutes, at least twice a day—once in the morning and once before bed. Use a soft-bristled toothbrush and a fluoride toothpaste. Consider an electric toothbrush, which many studies show is more effective at removing plaque.
- Floss Daily (or Use an Interdental Cleaner): Flossing is not optional. It removes plaque and food particles from between your teeth and under the gumline, where your toothbrush can’t reach. If you find flossing difficult, ask your dentist about alternatives like interdental brushes, soft picks, or a water flosser.
- Get Regular Dental Visits: See your dentist and hygienist for regular checkups and professional cleanings, usually every 6 to 12 months. If you have risk factors for periodontitis, you may need cleanings more frequently.
- Quit Smoking: If you smoke or use tobacco products, quitting is one of the most important things you can do for your gum health and overall health.
- Manage Systemic Health: Keep conditions like diabetes under control, eat a balanced diet, and manage stress. A healthy body supports a healthy mouth.
What are the Systemic Health Complications of Periodontitis?
The impact of advanced gum disease is not confined to the mouth.
The chronic inflammation and bacteria associated with periodontitis can have serious consequences for the rest of your body.
The bacteria can enter the bloodstream through the inflamed gum tissue and travel to other organs, triggering inflammation and contributing to a variety of health problems.
Strong scientific evidence links periodontitis to the following conditions:
- Coronary Artery Disease and Stroke: The chronic inflammation from periodontitis is linked to the development of atherosclerotic plaques in the arteries, increasing the risk of heart attack and stroke.
- Diabetes: The relationship is bidirectional. Periodontitis makes it more difficult for individuals with diabetes to control their blood sugar, and poorly controlled diabetes makes gum disease more severe.
- Respiratory Disease: Bacteria from the mouth can be inhaled into the lungs, potentially causing or worsening conditions like pneumonia and chronic obstructive pulmonary disease (COPD).
- Rheumatoid Arthritis: Periodontitis and rheumatoid arthritis are both chronic inflammatory diseases. Research suggests that the mechanism of tissue destruction in both conditions is similar, and having one may increase the risk and severity of the other.
- Pregnancy Complications: Pregnant women with periodontitis may have an increased risk of delivering their baby prematurely or having a baby with a low birth weight.
Treating periodontitis is a crucial step in reducing systemic inflammation and lowering the risk of these associated health complications.
Frequently Asked Questions About Periodontitis
1. Can periodontitis be cured?
Gingivitis, the first stage, is completely curable. However, the damage from periodontitis (bone and tissue loss) is largely irreversible without surgical intervention. Treatment can successfully stop the disease’s progression and manage it as a chronic condition, preventing further damage and tooth loss.
2. Is periodontitis contagious?
The bacteria that cause periodontitis can be passed from person to person through saliva (e.g., by sharing utensils or kissing). However, simply being exposed to the bacteria doesn’t mean you will develop the disease. Your own oral hygiene, genetics, and risk factors play a much larger role.
3. What does periodontitis look like?
In its early stages, it may just look like red, slightly swollen gums that bleed. In advanced stages, it looks like gums that have pulled far away from the teeth, making teeth appear long. You may also see pus, and teeth may look crooked or have gaps between them.
4. How long does it take to treat periodontitis?
Treatment time varies widely. Non-surgical scaling and root planing may involve one to four appointments, with a follow-up evaluation a few weeks later. Surgical treatments require more time for healing. Importantly, management is lifelong, requiring diligent home care and regular maintenance visits.
5. Can you have periodontitis without any pain?
Yes, absolutely. Periodontitis is often called a “silent” disease because pain is typically not a symptom until the disease is in its advanced stages. This is why you can’t rely on pain as a warning sign, regular dental checkups are essential for early detection.
6. What is the difference between gingivitis and periodontitis?
Gingivitis is inflammation of the gums only, with no bone loss, and it is reversible. Periodontitis is when the inflammation has spread to destroy the underlying bone and connective tissue. This damage is not reversible on its own and requires professional treatment to manage.
7. Does mouthwash help with periodontitis?
Over-the-counter cosmetic mouthwashes mainly mask bad breath. Therapeutic, antiseptic mouthwashes can help reduce plaque and gingivitis. However, no mouthwash can treat existing periodontitis, as it cannot reach deep into the pockets. It is only an adjunct to mechanical cleaning (brushing and flossing).
8. Is an electric or manual toothbrush better for periodontitis?
Many studies have shown that oscillating-rotating electric toothbrushes are generally more effective at removing plaque and reducing gingivitis than manual brushes. However, proper technique is the most important factor, and a manual brush used correctly can also be very effective.
Taking Control
Periodontitis is a serious, progressive disease, but it is also largely preventable and manageable.
By understanding the four stages—from reversible gingivitis to advanced periodontitis—you can recognize the early warning signs and take action before irreversible damage occurs.
The journey from plaque to tooth loss is a path that can be interrupted at any stage with the right intervention.
Remember, your oral health is a mirror of your overall health. A commitment to diligent daily care, combined with regular professional checkups, is your best defense.
Don’t ignore bleeding gums or other symptoms, assuming they will go away on their own.
Your clear call-to-action: If you have noticed any of the symptoms discussed in this article, or if it has been a while since your last dental visit, schedule an appointment with your dentist today. Taking control of your gum health is one of the most important investments you can make in your long-term well-being.
Found this article helpful? Share it with your friends and family to spread awareness about the importance of gum health.
Disclaimer
The information provided in this article is for educational and informational purposes only and does not constitute medical advice. It is not a substitute for professional diagnosis, treatment, or advice from a qualified healthcare provider. Always seek the advice of your dentist or other qualified health professional with any questions you may have regarding a medical condition.
References
- Periodontitis – Symptoms and causes. (2025). Mayo Clinic.
- Gum (Periodontal) Disease. (2025). National Institute of Dental and Craniofacial Research (NIDCR).
- Periodontitis. (2025). Healthline.
- Hajishengallis, G., & Chavakis, T. (2021). Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nature Reviews Immunology, 21(7), 426–440.

