Menopause is a universal and natural biological transition, yet its experience is deeply personal.
For many, the journey involves more than just the cessation of menstrual periods, it’s a complex interplay of physical and emotional changes driven by shifting hormones.
In the United States alone, approximately 6.000 women reach menopause every day, joining a global community expected to reach nearly 500 million by 2030, according to a report on the global impacts of menopause.
This guide moves beyond hot flashes to offer a comprehensive, evidence-based exploration of the full spectrum of menopause symptoms.
We will delve into natural, holistic strategies for managing everything from weight gain and sleep disturbances to mood swings and brain fog.
By understanding the underlying causes and exploring effective, science-backed natural remedies, you can navigate this transition with greater comfort, confidence, and well-being.
In This Article
What Exactly is Menopause and What Causes Its Symptoms?
Menopause is officially diagnosed after you’ve gone 12 consecutive months without a menstrual period.
It’s not an illness but a natural stage of life marking the end of your reproductive years.
The average age for menopause in the United States is 51, but the transition can begin years earlier.
The symptoms associated with this phase are primarily caused by the decline in reproductive hormones produced by the ovaries.
The Three Stages: Perimenopause, Menopause, and Postmenopause
The menopausal journey is a gradual process, typically divided into three distinct stages:
- Perimenopause: Meaning “around menopause”, this transitional phase can begin in your 40s, or even late 30s, and lasts an average of four years, though it can range from a few months to a decade. During this time, estrogen levels fluctuate unpredictably, causing the first signs of menopausal symptoms like irregular periods, hot flashes, and sleep problems.
- Menopause: This is the specific point in time when you have had no menstrual period for 12 straight months. At this stage, the ovaries have stopped releasing eggs and produce very little estrogen.
- Postmenopause: This refers to the years following menopause. Menopausal symptoms may continue for some time, but for many women, they begin to ease. However, due to lower estrogen levels, the risk for certain health conditions, such as osteoporosis and heart disease, increases.
The Hormonal Rollercoaster: Estrogen, Progesterone, and Their Impact
The vast array of menopause symptoms stems from the declining production of two key hormones: estrogen and progesterone.
- Estrogen: This is the primary female hormone. It regulates the menstrual cycle and affects the reproductive system, urinary tract, heart, blood vessels, bones, skin, hair, and brain. As estrogen levels drop, you may experience hot flashes, vaginal dryness, bladder issues, and changes in skin elasticity.
- Progesterone: This hormone helps prepare the uterus for pregnancy and regulates the menstrual cycle. Fluctuations and eventual decline in progesterone can contribute to irregular periods and may affect sleep and mood.
This hormonal shift doesn’t happen overnight. The erratic fluctuations during perimenopause are what often cause the most disruptive symptoms, as the body struggles to adapt to its new hormonal environment. As confirmed by leading institutions like the Mayo Clinic, this transition is a natural decline, but its effects can significantly impact daily life.
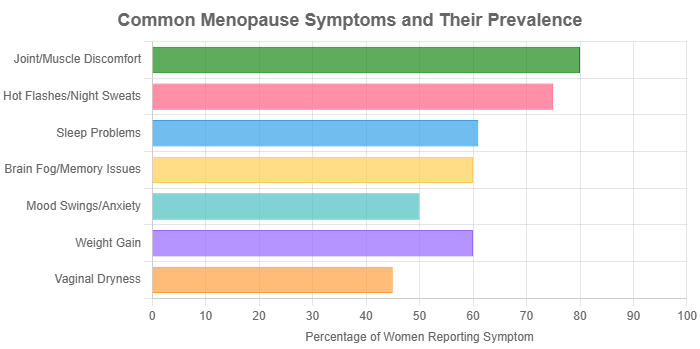
Data synthesized from sources including the International Menopause Society, WHO, and major health clinics.
How Can I Naturally Manage Hot Flashes and Night Sweats?
Hot flashes (or flushes) are the most frequently reported menopause symptom, characterized by a sudden feeling of intense heat, often accompanied by a flushed face and sweating.
When they occur at night, they are called night sweats and can severely disrupt sleep.
Lifestyle Adjustments: The First Line of Defense
Before turning to supplements or therapies, simple lifestyle changes can provide significant relief. The Office on Women’s Health recommends a proactive approach:
- Identify and Avoid Triggers: Keep a journal to track what might be setting off your hot flashes. Common culprits include stress, caffeine, alcohol, spicy foods, and hot environments.
- Dress in Layers: Wearing layers allows you to remove clothing quickly when you feel a hot flash coming on. Opt for natural, breathable fabrics like cotton and linen.
- Stay Cool: Keep your bedroom cool at night, use a fan, and sip on ice water throughout the day. A “chill pillow” or cooling mattress pad can also be beneficial.
- Maintain a Healthy Weight: Research suggests that women with a higher body mass index (BMI) may experience more frequent and severe hot flashes.
Evidence-Based Herbal Supplements: Black Cohosh and Isoflavones
Many women seek natural remedies for hot flashes. While the market is flooded with options, a few have been studied more extensively.
It’s crucial to approach supplements with caution and consult a healthcare provider.
- Black Cohosh (Cimicifuga racemosa): This is one of the most studied herbs for menopause. A review of several clinical trials published in the Journal of Menopausal Health suggests its effectiveness in treating menopausal symptoms. However, results are mixed, and it may not work for everyone. It should be used with caution in individuals with liver problems.
- Soy Isoflavones: These are plant-based compounds that have a weak estrogen-like effect on the body. Found in soy products (tofu, edamame, soy milk) and supplements, they may help reduce the severity and frequency of hot flashes. A systematic review in the journal Nutrients found that isoflavones significantly lowered hot flash frequency.
Mind-Body Therapies: The Power of Acupuncture and CBT
Managing hot flashes isn’t just about physical remedies, your mental state plays a significant role.
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body. A meta-analysis published in the International Journal of Women’s Health and Reproduction Sciences concluded that acupuncture can significantly reduce menopausal vasomotor symptoms, including hot flashes and night sweats, compared to no treatment.
- Cognitive Behavioral Therapy (CBT): CBT is a type of talk therapy that helps you change unhelpful thinking patterns and behaviors. Research has shown that CBT can reduce the distress caused by hot flashes and improve sleep. A study highlighted by PMC found that CBT effectively reduced the subjective frequency of night sweats.
Why Am I Gaining Weight and What Can I Do About It?
Many women notice an increase in weight, particularly around the abdomen, during the menopausal transition.
This is often frustratingly referred to as “menopause belly”.
This shift is not just due to aging but is directly linked to hormonal changes.
Understanding “Menopause Belly”: Hormones, Metabolism, and Fat Distribution
The weight gain experienced during menopause is multifactorial:
- Hormonal Shifts: The decline in estrogen causes the body to store fat differently, shifting it from the hips and thighs to the abdominal area. This visceral fat is not only a cosmetic concern but is also linked to a higher risk of cardiovascular disease and type 2 diabetes.
- Slowing Metabolism: As we age, our metabolism naturally slows down. The loss of muscle mass, which is accelerated by declining estrogen, further reduces the rate at which your body burns calories.
- Increased Insulin Resistance: Changes in hormone levels can make the body’s cells less responsive to insulin, leading to higher blood sugar and a greater tendency to store fat.
The Role of Diet: Embracing the Mediterranean Approach
While no magic diet exists, certain eating patterns are particularly beneficial during menopause.
The Mediterranean diet consistently comes out on top in scientific research.
A systematic review in the journal Nutrients (2024) suggests that menopausal women following a Mediterranean diet may experience benefits such as reduced blood pressure, lower triglycerides, and better weight management.
This diet emphasizes:
- Whole Foods: Fruits, vegetables, whole grains, legumes, nuts, and seeds.
- Healthy Fats: Olive oil as the primary source of fat, along with avocados and fatty fish.
- Lean Protein: Fish and poultry in moderation, with limited red meat.
- Phytoestrogens: Foods like flaxseeds, chickpeas, and lentils contain plant estrogens that may help buffer some hormonal symptoms.
The Importance of Exercise: Combining Cardio and Strength Training
Exercise is non-negotiable for managing weight, overall health, and many menopause symptoms. A combination of approaches is most effective:
- Cardiovascular Exercise: Activities like brisk walking, jogging, swimming, or cycling help burn calories, improve heart health, and boost mood. Aim for at least 150 minutes of moderate-intensity cardio per week.
- Strength Training: This is crucial for combating muscle loss. Lifting weights, using resistance bands, or doing bodyweight exercises (like squats and push-ups) builds lean muscle mass, which in turn boosts your metabolism. The British Menopause Society emphasizes strength exercise as a key component of long-term weight management.
What are the Best Natural Solutions for Sleep Problems During Menopause?
Sleep disturbances are a hallmark of the menopausal transition.
According to a study in Sleep Medicine Clinics, the most common complaint is frequent nighttime awakenings.
This can be caused by night sweats, anxiety, or the hormonal changes themselves.
Creating a Sleep-Friendly Environment and Routine
Good sleep hygiene is the foundation for better rest:
- Consistent Schedule: Go to bed and wake up at the same time every day, even on weekends.
- Cool, Dark, and Quiet: Optimize your bedroom for sleep. Use blackout curtains, a white noise machine, and keep the temperature cool (around 65°F or 18°C).
- Limit Screen Time: The blue light from phones, tablets, and TVs can interfere with the production of melatonin, the sleep hormone. Avoid screens for at least an hour before bed.
- Mindful Wind-Down: Create a relaxing pre-sleep ritual, such as taking a warm bath, reading a book, listening to calm music, or practicing gentle stretching.
Herbal Aids for Sleep: Valerian, Chamomile, and More
Several herbs have traditionally been used to promote sleep and relaxation.
While more research is needed, many women find them helpful.
- Valerian Root: Often used for insomnia and anxiety, valerian may help you fall asleep faster and improve sleep quality.
- Chamomile: Typically consumed as a tea, chamomile contains an antioxidant called apigenin, which binds to specific receptors in your brain that may decrease anxiety and initiate sleep.
- Lemon Balm: A member of the mint family, lemon balm is known for its calming effects and is often used to reduce stress and improve sleep.
Addressing Night Sweats to Improve Sleep Quality
If night sweats are the primary cause of your sleep disruption, addressing them directly is key.
All the strategies for managing hot flashes—such as avoiding triggers, dressing in breathable sleepwear, and using cooling bedding—will also help reduce nighttime awakenings.
How Can I Cope with Mood Swings, Anxiety, and Brain Fog?
The emotional and cognitive changes are some of the most challenging menopause symptoms, often proving just as difficult as the physical ones.
Fluctuating hormones can impact neurotransmitters in the brain, leading to irritability, anxiety, feelings of sadness, and difficulty with memory and focus (often called “brain fog“).
Cognitive Behavioral Therapy (CBT) for Emotional Regulation
CBT is not just for hot flashes, it is a highly effective, non-hormonal treatment for the mood-related symptoms of menopause.
A 2024 study published in Journal of Affective Disorders found that CBT led to significant reductions in both depressed mood and anxiety symptoms in menopausal women.
It works by helping you identify and challenge negative thought patterns that contribute to feelings of anxiety and low mood.
Nutritional Support for Brain Health
What you eat can have a profound effect on your brain function and mood.
- Omega-3 Fatty Acids: Found in fatty fish (salmon, mackerel), walnuts, and flaxseeds, omega-3s are critical for brain health and have anti-inflammatory properties that may help with mood.
- B Vitamins: Vitamins B6, B12, and folate are essential for neurotransmitter production. Deficiencies can be linked to depression and cognitive decline. Good sources include leafy greens, eggs, and legumes.
- Phytoestrogens: As mentioned earlier, foods rich in phytoestrogens (like soy and flax) may offer some mood-stabilizing benefits due to their weak estrogenic activity.
The Mental Benefits of Mindfulness and Regular Exercise
Physical activity is a powerful tool for mental health.
Exercise releases endorphins, which have mood-boosting effects.
Activities like yoga and tai chi are particularly beneficial as they combine physical movement with mindfulness and deep breathing, which can calm the nervous system and improve focus.
What Natural Treatments Exist for Vaginal Dryness and Discomfort?
Vaginal atrophy, or the thinning, drying, and inflammation of the vaginal walls, is a common and often under-reported symptom of menopause.
It’s caused by the drop in estrogen and can lead to pain during intercourse (dyspareunia), itching, and an increased risk of urinary tract infections.
Over-the-Counter Solutions: Moisturizers vs. Lubricants
These are effective, non-hormonal first-line treatments:
- Vaginal Moisturizers: These are used regularly (every 2-3 days) to restore moisture to the vaginal tissues, not just during sexual activity. They provide ongoing relief from general dryness and itching.
- Vaginal Lubricants: These are used at the time of sexual activity to reduce friction and pain. Water-based or silicone-based lubricants are recommended.
The Role of Phytoestrogens and Vitamin E
Some natural compounds may help improve vaginal health.
A review in PMC noted that treatments including Vitamin E and Vitamin D have been used to improve vaginal atrophy.
Applying Vitamin E oil (from a capsule) directly to the vagina or using suppositories may provide relief for some women.
Similarly, a diet rich in phytoestrogens may help maintain tissue elasticity.
The Importance of Pelvic Floor Health
The pelvic floor muscles support the bladder, uterus, and bowel.
Weakening of these muscles due to age and hormonal changes can exacerbate urinary and vaginal symptoms.
Regular pelvic floor exercises (Kegels) can strengthen these muscles, improving bladder control and potentially increasing blood flow to the pelvic region, which can help with lubrication and arousal.
What are the Long-Term Health Considerations After Menopause?
The decline in estrogen has implications beyond the immediate menopause symptoms.
It’s a critical time to focus on preventive health to reduce the risk of chronic conditions.
Protecting Your Bones: Preventing Osteoporosis
Estrogen plays a vital role in maintaining bone density.
Its decline leads to accelerated bone loss, increasing the risk of osteoporosis—a condition where bones become weak and brittle. To protect your bones:
- Calcium and Vitamin D: These two nutrients work together. Calcium is the building block of bone, and Vitamin D is necessary for its absorption. Aim for 1.200 mg of calcium and 800-1.000 IU of Vitamin D per day from diet and/or supplements.
- Weight-Bearing Exercise: Activities like walking, jogging, dancing, and strength training stimulate bone-forming cells, helping to maintain bone density.
Supporting Cardiovascular Health
Estrogen has a protective effect on the heart and blood vessels.
After menopause, a woman’s risk of heart disease rises to equal that of a man’s. Key preventive strategies include:
- Heart-Healthy Diet: The Mediterranean diet is excellent for cardiovascular health, as it helps manage cholesterol, blood pressure, and inflammation.
- Regular Exercise: Cardio and strength training are both essential for maintaining a healthy heart.
- Don’t Smoke: Smoking is a major risk factor for heart disease.
- Manage Stress: Chronic stress can contribute to high blood pressure and other heart disease risk factors.
Comparative Table of Natural Remedies for Menopause Symptoms
This table summarizes some of the natural approaches discussed, their primary targets, and the level of scientific evidence supporting them.
| Remedy/Approach | Primary Target Symptoms | Level of Evidence | Key Considerations |
|---|---|---|---|
| Lifestyle Adjustments | Hot Flashes, Sleep, Weight, Mood | High | Foundation of any management plan. Requires consistency. |
| Mediterranean Diet | Weight Gain, Heart Health, Mood, Overall Well-being | High | A sustainable long-term eating pattern, not a short-term diet. |
| Strength Training | Weight Gain, Bone Health, Metabolism, Mood | High | Crucial for preserving muscle mass. Aim for 2-3 sessions per week. |
| Cognitive Behavioral Therapy (CBT) | Hot Flashes (distress), Mood Swings, Anxiety, Insomnia | High | Requires a trained therapist. Can be done online or in person. |
| Acupuncture | Hot Flashes, Sleep, Mood | Moderate | More effective than no treatment. Find a licensed practitioner. |
| Soy Isoflavones | Hot Flashes, Vaginal Dryness, Bone Health | Moderate | Results vary. Choose whole soy foods over processed supplements. |
| Black Cohosh | Hot Flashes, Night Sweats | Mixed | Some studies show benefit, others don’t. Consult a doctor, especially if you have liver issues. |
| Vaginal Moisturizers | Vaginal Dryness, Painful Sex | High | Safe and effective first-line treatment. Use regularly. |
Frequently Asked Questions (FAQ) About Menopause Symptoms
- How long do menopause symptoms last?
The duration varies greatly. Perimenopausal symptoms can last for an average of 4-7 years, but some women experience them for a decade or more. For many, symptoms like hot flashes lessen in severity after menopause. - Can I still get pregnant during perimenopause?
Yes. As long as you are still having periods, even if they are irregular, pregnancy is possible. It’s recommended to continue using contraception until you have gone 12 full months without a period. - Are natural remedies safe?
“Natural” does not always mean “safe”. Herbal supplements can interact with medications and have side effects. It is essential to discuss any supplements with your healthcare provider before starting them. - Is hormone replacement therapy (HRT) my only other option?
No. While HRT is an effective treatment for many, there are also non-hormonal prescription medications (like certain antidepressants) that can help with hot flashes and mood symptoms, in addition to the natural strategies outlined here. - Why is my anxiety worse during menopause?
Hormonal fluctuations, particularly of estrogen and progesterone, can disrupt the balance of mood-regulating neurotransmitters in the brain. Combined with life stressors and poor sleep, this can heighten feelings of anxiety. - Is it normal to feel so forgetful?
Yes, “brain fog” is a very common complaint. Difficulties with short-term memory, focus, and finding the right words are often reported. Improving sleep, managing stress, and regular exercise can help. - Does menopause cause depression?
While menopause itself doesn’t directly cause clinical depression, the risk is higher during this transition. If you feel persistently sad, hopeless, or lose interest in activities you once enjoyed, it’s crucial to seek professional help. - Will my sex drive return after menopause?
It varies. Some women find their libido decreases due to vaginal dryness or hormonal changes. Others feel more sexually liberated without the fear of pregnancy. Addressing physical discomfort and communicating with your partner are key.
Conclusion
Navigating the full range of menopause symptoms requires a holistic and personalized approach.
While hot flashes often take center stage, this transition impacts nearly every aspect of a woman’s physical and emotional health.
By focusing on foundational lifestyle strategies—a nutrient-dense diet, consistent exercise, stress management, and good sleep hygiene—you can build a strong base for well-being.
Evidence-based natural remedies, from mind-body therapies like CBT to targeted supplements, can offer additional layers of support.
The key is to become an informed advocate for your own health, to understand the changes your body is undergoing, and to work with healthcare providers to create a management plan that feels right for you.
Menopause is not an ending, but a new chapter—one that you can enter with strength, knowledge, and confidence.

