Meniere’s disease is a chronic disorder of the inner ear characterized by spontaneous episodes of vertigo, fluctuating hearing loss, tinnitus, and a sensation of fullness in the ear.
This condition, which typically affects only one ear, can be debilitating due to the unpredictable nature of its attacks.
According to the National Institute on Deafness and Other Communication Disorders (NIDCD), an estimated 615.000 individuals in the United States are affected by Meniere’s disease, with around 45.500 new cases diagnosed each year.
While there is no cure, a comprehensive understanding of the disease is the first step toward effective management.
The journey for those with Meniere’s disease is often marked by uncertainty and a significant impact on quality of life.
The sudden onset of severe dizziness can disrupt work, social activities, and daily routines, leading to anxiety and stress.
This in-depth guide is designed to demystify Meniere’s disease, providing a clear, authoritative overview of its symptoms, underlying causes, the latest diagnostic techniques, and a full spectrum of treatment options—from lifestyle adjustments to cutting-edge research.
By exploring this complex condition, we aim to empower patients and their families with the knowledge needed to navigate their diagnosis and reclaim control over their lives.
In This Article
What Exactly is Meniere’s Disease?
Meniere’s disease, first described by French physician Prosper Menière in 1861, is a disorder of the inner ear that disrupts the body’s sense of balance and hearing.
It is medically known as idiopathic endolymphatic hydrops, a term that points to its core pathological feature: an abnormal accumulation of fluid, called endolymph, within the inner ear’s membranous labyrinth.
This fluid buildup creates excess pressure, interfering with the normal balance and hearing signals sent from the inner ear to the brain.
The inner ear is a complex system of tubes and sacs, known as the labyrinth. It contains the organs for both hearing (the cochlea) and balance (the semicircular canals and otolith organs).
In a healthy ear, the endolymph fluid volume is tightly regulated.
In Meniere’s disease, this regulation fails, leading to a condition called endolymphatic hydrops.
This distention and pressure fluctuation is believed to be the direct cause of the disease’s hallmark symptoms.
As described by Johns Hopkins Medicine, Meniere’s disease is fundamentally a balance disorder caused by an abnormality in the labyrinth. The fluid buildup can trigger severe vertigo, hearing loss, and other distressing symptoms without warning.
While it is considered a lifelong, chronic condition, the severity and frequency of symptoms can vary dramatically among individuals and over the course of a person’s life.
Many people experience periods of remission, where symptoms subside for months or even years.
The condition most often affects only one ear (unilateral), but bilateral involvement can occur, sometimes developing years after the initial onset.
According to the NIDCD, bilateral Meniere’s disease may affect 15% to 25% of individuals with the disorder.
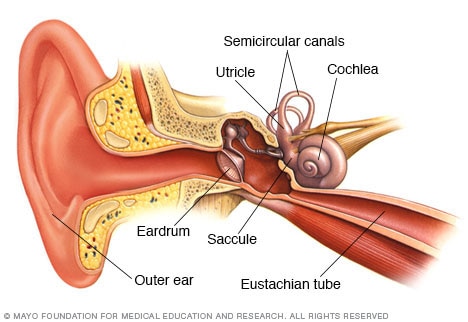
The inner ear contains the labyrinth, where fluid buildup associated with Meniere’s disease occurs, affecting both hearing (cochlea) and balance (semicircular canals).
How Common is Meniere’s Disease?
While Meniere’s disease is one of the more well-known inner ear disorders, it is relatively uncommon.
Epidemiological data can vary widely across studies, partly due to differing diagnostic criteria and geographical locations. However, several key statistics provide a general picture of its prevalence.
- U.S. Prevalence: The NIDCD and the American Hearing Research Foundation (AHRF) estimate that approximately 615.000 people in the United States have Meniere’s disease. This represents about 0.2% of the U.S. population.
- Annual Incidence: Around 45.500 new cases are diagnosed each year in the U.S.
- Global Variation: Reported prevalence rates worldwide show significant variation, ranging from as low as 3.5 per 100.000 to as high as 513 per 100.000 people, as noted in a review published in StatPearls. This discrepancy highlights the ongoing challenges in accurately diagnosing and tracking the condition.
- Age of Onset: Meniere’s disease can develop at any age, but it most commonly begins between the ages of 40 and 60. It is considered rare in children.
- Gender: Some studies suggest a slightly higher prevalence in females, but the distribution is generally considered to be fairly equal between men and women.
It’s important to note that while these numbers classify Meniere’s as a rare disorder, its impact is profound.
The unpredictable nature of the attacks means that even with a relatively low prevalence, it causes a significant societal and personal burden, affecting productivity, mental health, and overall quality of life.
What are the Core Symptoms of Meniere’s Disease?
Meniere’s disease is defined by a specific cluster of symptoms that occur in episodes or “attacks”.
While not every person experiences all symptoms, a diagnosis typically requires the presence of a characteristic combination.
The four classic, or cardinal, symptoms are:
1. Spontaneous, Episodic Vertigo
This is often the most debilitating symptom. Vertigo is not just dizziness, it’s a distinct sensation of spinning or rotational movement, as if you or the room around you is moving.
Key features of Meniere’s-related vertigo include:
- Sudden Onset: Attacks can start without any warning.
- Duration: An episode of vertigo typically lasts from 20 minutes to 12 hours, but never more than 24 hours.
- Severity: The spinning sensation can be so intense that it leads to severe nausea, vomiting, sweating, and loss of balance, making it impossible to stand or walk.
- Drop Attacks (Tumarkin’s Otolithic Crisis): In some cases, individuals may experience sudden falls without losing consciousness. These “drop attacks” are thought to be caused by an abrupt mechanical shift in the otolith organs of the inner ear.
2. Fluctuating Hearing Loss
Hearing loss in Meniere’s disease is sensorineural, meaning it originates in the inner ear.
It has several distinct characteristics:
- Fluctuation: Especially in the early stages, hearing ability may come and go. Hearing often worsens during or just before an attack and may improve afterward.
- Low-Frequency Loss: Initially, the hearing loss primarily affects low-pitched sounds. This can make it difficult to hear deep voices or background noise.
- Progression: Over many years, the hearing loss can become more severe and permanent, eventually affecting all frequencies.
3. Tinnitus
Tinnitus is the perception of sound in the ear when no external sound is present.
In Meniere’s disease, tinnitus is often described as:
- Sound Quality: A low-pitched roaring, hissing, buzzing, or ringing sound.
- Fluctuation: The loudness of the tinnitus often increases before or during a vertigo attack.
- Persistence: While it may fluctuate, for many, tinnitus becomes a constant companion between attacks.
4. Aural Fullness
This is a sensation of pressure, blockage, or fullness within the affected ear.
It is often compared to the feeling of having water in the ear or the pressure changes experienced during an airplane’s ascent or descent.
This feeling frequently precedes a vertigo attack.
According to the Mayo Clinic, a person with Meniere’s disease will typically experience at least two to three of these core symptoms at once during an attack. Between episodes, some people may be completely symptom-free, while others are left with persistent tinnitus and hearing loss.
What Causes Meniere’s Disease? The Unfolding Mystery
Despite being recognized for over 160 years, the exact cause of Meniere’s disease remains unknown, or idiopathic.
However, the scientific community agrees that the symptoms are a direct result of endolymphatic hydrops—the buildup of endolymph fluid in the inner ear.
The central question is: what causes this fluid imbalance in the first place?
Research has moved beyond a single-cause theory and now points to Meniere’s disease as a complex, multifactorial condition where several factors may converge to trigger the disease.
A 2025 review in Frontiers in Neurology titled “A modern conceptual framework for study and treatment of Meniere’s disease“ highlights this shift, emphasizing the need to segregate patients into subtypes based on underlying causes.
Here are the leading theories and contributing factors currently under investigation:
1. Anatomical and Drainage Issues
The traditional theory posits a mechanical problem.
The endolymphatic sac, part of the inner ear, is responsible for regulating endolymph volume and pressure.
It’s thought that poor fluid drainage, perhaps due to a blockage, an anatomical abnormality of the temporal bone, or an underdeveloped vestibular aqueduct, could lead to fluid accumulation.
2. Genetic Predisposition
Evidence for a genetic link is growing.
Meniere’s disease can run in families, with about 5-10% of cases being familial.
Recent genomic studies are identifying specific genes that may increase susceptibility.
A 2024 study in BMC Genomics, “The genomic landscape of Ménière’s disease”, identified several high-priority genes (like MYO6, OTOGL, and TRIOBP) involved in cochlear function, cell adhesion, and energy maintenance that are implicated in the disease.
This research opens the door for future genetic screening and targeted therapies.
3. Autoimmune and Inflammatory Responses
This is one of the most active areas of research.
A significant portion of Meniere’s patients also have autoimmune disorders like rheumatoid arthritis or lupus.
A 2025 review in Frontiers in Immunology, “Immunological mechanisms in Meniere’s disease”, details how immune dysregulation may be a central driver.
The theory suggests that the body’s own immune system mistakenly attacks inner ear structures, causing inflammation.
This inflammation can disrupt the delicate fluid balance and damage sensory cells.
Researchers have found elevated levels of pro-inflammatory cytokines (like TNF-α, IL-1β, and IL-6) and immune cells in the inner ears of Meniere’s patients.
4. Viral Infections
Past viral infections, such as those from the herpes simplex virus (HSV), varicella-zoster virus (VZV, which causes chickenpox and shingles), or cytomegalovirus (CMV), are considered potential triggers.
The virus may lie dormant in the nerve cells of the inner ear and reactivate later in life, causing inflammation and damage that leads to endolymphatic hydrops.
5. Allergies
A link between allergies and Meniere’s disease has been observed.
Allergic reactions can cause inflammation and fluid shifts throughout the body, and it’s plausible that these reactions could specifically affect the inner ear in susceptible individuals, exacerbating symptoms or triggering attacks.
6. Vascular Issues
Some researchers propose that constricted blood vessels in the inner ear, similar to what occurs in migraine headaches, could compromise blood flow.
This ischemia (lack of oxygen) could damage the tissues responsible for maintaining fluid balance, leading to hydrops.
The high rate of comorbidity between Meniere’s disease and vestibular migraine lends support to this theory.
In all likelihood, Meniere’s disease is not caused by a single factor but by a combination of these elements.
A person might have a genetic predisposition that, when combined with a viral infection or an autoimmune response, finally triggers the onset of the disease.
How Does Meniere’s Disease Progress Over Time?
Meniere’s disease is a chronic condition, but its course is highly variable and often unpredictable.
The disease typically evolves through different stages, and understanding this progression can help manage expectations and treatment.
Early Stage
In the initial years, the disease is often characterized by sudden, severe, and unpredictable attacks of vertigo.
These episodes can be frequent and are usually accompanied by fluctuating hearing loss, tinnitus, and aural fullness.
Between attacks, many individuals feel completely normal, and their hearing may return to its baseline.
This “on-off” nature is one of the most challenging aspects of the early stage.
Mid Stage
As the disease progresses, the character of the symptoms may change.
The vertigo attacks might become less severe or less frequent.
However, the hearing loss and tinnitus often become more constant and less likely to fluctuate.
The hearing loss may start to become permanent, and periods of remission between attacks may shorten.
Late Stage
After 5 to 15 years, many patients enter a “burnout” phase.
In this stage, the severe, spontaneous vertigo attacks often cease or become rare.
This is believed to happen because the balance function in the affected ear has been significantly and permanently damaged.
While the terrifying vertigo may be gone, it is often replaced by chronic, less intense balance problems, such as a constant feeling of unsteadiness, especially in the dark or on uneven surfaces.
The hearing loss in the affected ear is typically severe and permanent at this point, and tinnitus is usually constant.
Bilateral Progression
A significant concern for many with unilateral Meniere’s is the risk of it developing in the other ear.
The rate of progression to bilateral disease varies widely in studies, from 13% to as high as 50% over a lifetime.
A 2024 study in Frontiers in Neurology noted that in some cases, the second ear becomes involved within two years, while for others it may take five years or more.
There is no definitive way to predict who will develop bilateral disease.
It’s a crucial point of experience for patients: while the terrifying, room-spinning vertigo may lessen over time, the trade-off is often a permanent decline in hearing and a shift to chronic instability. This evolution requires a corresponding shift in management strategies, from acute attack treatment to long-term vestibular rehabilitation and hearing amplification.
Who is at Risk for Developing Meniere’s Disease?
While the definitive cause of Meniere’s disease is not yet known, research has identified several factors that may increase a person’s risk of developing the condition.
These risk factors align with the leading theories about its underlying causes.
- Age: The most significant risk factor is age. Meniere’s disease is most likely to appear in adults between 40 and 60 years old.
- Family History (Genetics): Having a close relative with Meniere’s disease increases your risk. As noted in StatPearls, about 10% of cases in people of European descent are familial, suggesting a polygenic disorder.
- Autoimmune Disorders: People with existing autoimmune conditions, such as rheumatoid arthritis, systemic lupus erythematosus, or ankylosing spondylitis, have a higher risk. This supports the theory that immune system dysfunction plays a role.
- Migraine: There is a strong association and symptomatic overlap between Meniere’s disease and vestibular migraine. Individuals who suffer from migraines may be more susceptible.
- Previous Ear Trauma or Infection: A history of a major ear infection or physical trauma to the head or ear could potentially damage inner ear structures, predisposing an individual to the fluid regulation problems seen in Meniere’s.
- Allergies: Severe allergies, particularly those affecting the upper respiratory system, may be a contributing factor due to the inflammatory response they trigger.
How is Meniere’s Disease Diagnosed?
There is no single, definitive test for Meniere’s disease.
The diagnosis is primarily clinical, made by an otolaryngologist (ENT) or a neurotologist based on a patient’s medical history, symptoms, and the exclusion of other conditions.
The American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) and the Bárány Society have established specific diagnostic criteria to standardize the process.
Diagnostic Criteria for Definite Meniere’s Disease
According to the consensus criteria, a diagnosis of definite Meniere’s disease requires:
- Two or more spontaneous episodes of vertigo, each lasting 20 minutes to 12 hours.
- Audiometrically documented low- to mid-frequency sensorineural hearing loss in the affected ear on at least one occasion before, during, or after one of the vertigo episodes.
- Fluctuating aural symptoms (hearing loss, tinnitus, or fullness) in the affected ear.
- Symptoms not better accounted for by another vestibular diagnosis.
A diagnosis of probable Meniere’s disease may be made if a patient has the characteristic vertigo episodes and fluctuating aural symptoms, but the hearing loss has not yet been documented on an audiogram.
Diagnostic Tests
To confirm the diagnosis and rule out other causes, a doctor will order a battery of tests:
Hearing Tests (Audiometry)
This is a crucial test to document the characteristic hearing loss.
An audiogram measures your ability to hear sounds at different pitches and volumes.
For Meniere’s, it will typically show a low-frequency sensorineural hearing loss in the affected ear, which helps distinguish it from age-related hearing loss (which affects high frequencies) or conductive hearing loss.
Balance Tests (Vestibular Function Tests)
These tests assess the function of the balance portion of the inner ear.
A reduced balance response in one ear is a common finding in Meniere’s disease.
- Electronystagmography (ENG) or Videonystagmography (VNG): This test measures involuntary eye movements (nystagmus) in response to stimuli. Electrodes (ENG) or goggles (VNG) are placed around the eyes while warm and cool water or air is introduced into the ear canal. This caloric stimulation should trigger a balance respons, abnormalities can indicate inner ear damage.
- Rotary Chair Testing: You sit in a computer-controlled chair that moves slowly back and forth. This test also measures eye movements to assess how your inner ear and brain are coordinating balance. It can help differentiate between an inner ear problem and a brain-related issue.
- Vestibular Evoked Myogenic Potentials (VEMP): This test measures the function of the otolith organs (utricle and saccule). It uses sound to stimulate the inner ear and records the resulting muscle response in the neck or under the eyes. It can show characteristic changes in Meniere’s disease.
- Video Head Impulse Test (vHIT): This newer test uses a high-speed camera to measure eye movements in response to quick, unpredictable head turns. It directly assesses the function of the semicircular canals.
- Computerized Dynamic Posturography (CDP): This test evaluates your balance system as a whole (vision, inner ear, and sensation from the feet). You stand on a platform that moves, and the test measures your ability to maintain balance under various conditions.
Other Tests to Rule Out Other Conditions
Symptoms of Meniere’s disease can mimic other serious conditions. Therefore, imaging is often necessary.
- Magnetic Resonance Imaging (MRI): A head MRI with contrast is essential to rule out other causes of vertigo and hearing loss, such as a vestibular schwannoma (acoustic neuroma) or multiple sclerosis (MS).
- Auditory Brainstem Response (ABR): This test measures the electrical activity of the hearing nerve and brain pathways. It can help differentiate between a problem in the inner ear versus the auditory nerve itself.
What are the Latest Advances in Diagnosing Meniere’s Disease?
For decades, Meniere’s disease was a purely clinical diagnosis, relying on patient-reported symptoms and the exclusion of other disorders.
A major breakthrough in recent years has been the ability to directly visualize the underlying pathology—endolymphatic hydrops—using advanced imaging techniques.
Visualizing Endolymphatic Hydrops with MRI
High-resolution Magnetic Resonance Imaging (MRI) protocols can now make endolymphatic hydrops visible.
This has been a paradigm shift, moving Meniere’s from a diagnosis of exclusion to one that can be supported by objective, anatomical evidence.
As explained by Radiopaedia.org and confirmed in multiple research articles, the technique typically involves administering a gadolinium-based contrast agent, either intravenously or directly into the middle ear (intratympanic).
The contrast agent diffuses into the perilymph fluid but not the endolymph.
On delayed imaging (usually 4 hours or more after injection), the fluid-filled spaces can be distinguished:
- The perilymphatic space (containing perilymph) will appear bright.
- The endolymphatic space (containing endolymph) will appear dark.
In a patient with Meniere’s disease, the dark endolymphatic space (particularly in the cochlea and vestibule) will be visibly enlarged or distended compared to the bright perilymphatic space.
This provides direct visual confirmation of hydrops.
A 2025 multicenter study published in Diagnostic and Interventional Radiology highlighted the development of a diagnostic model based on MRI, underscoring its growing importance in clinical practice. While not yet a routine test everywhere, this advanced MRI is becoming a powerful tool for confirming the diagnosis, especially in atypical cases.
This ability to visualize hydrops is not just diagnostic, it’s also helping researchers better understand the disease, correlate the degree of hydrops with symptom severity, and evaluate the effectiveness of treatments aimed at reducing fluid volume.
How is Meniere’s Disease Treated? A Stepwise Approach
There is no cure for Meniere’s disease, so treatment focuses on managing symptoms and improving quality of life.
The approach is typically stepwise, starting with the least invasive options and progressing to more aggressive treatments if symptoms are not controlled.
The primary goals are to reduce the frequency and severity of vertigo attacks, preserve hearing, and minimize tinnitus.
| Treatment Tier | Intervention | Primary Goal | Pros | Cons |
|---|---|---|---|---|
| First-Line (Conservative) | Dietary & Lifestyle Changes (Low-sodium diet, limit caffeine/alcohol, stress management) | Reduce fluid retention and attack triggers. | Non-invasive, safe, empowers patient. | Requires significant commitment; effectiveness varies. |
| First-Line (Medical) | Diuretics (“water pills”) | Reduce overall body fluid, including in the inner ear. | Can reduce frequency/severity of attacks. | Side effects (e.g., electrolyte imbalance); requires monitoring. |
| Acute Attack Medication | Vestibular Suppressants (e.g., meclizine, diazepam), Anti-emetics (e.g., promethazine) | Stop vertigo and nausea during an attack. | Effective for immediate symptom relief. | Cause drowsiness; not for long-term use; do not prevent attacks. |
| Second-Line (Minimally Invasive) | Intratympanic Steroid Injections | Reduce inner ear inflammation and vertigo. | Good vertigo control with minimal risk to hearing. | May require multiple injections; effects can be temporary. |
| Third-Line (Destructive) | Intratympanic Gentamicin Injections | Ablate (destroy) vestibular cells to stop vertigo. | Highly effective for vertigo control (~90%). | Significant risk of permanent hearing loss (up to 30%). Reserved for severe cases. |
| Rehabilitative | Vestibular Rehabilitation Therapy (VRT) | Train the brain to compensate for balance deficits. | Improves balance and stability, especially between attacks or after other procedures. | Less effective for acute, episodic vertigo; requires patient participation. |
| Surgical (Non-Destructive) | Endolymphatic Sac Decompression | Relieve pressure by draining excess fluid. | Aims to preserve hearing and balance function. | Controversial efficacy; success rates vary widely (60-80%). |
| Surgical (Destructive) | Labyrinthectomy or Vestibular Nerve Section | Permanently stop vertigo signals from the affected ear. | Highest success rate for eliminating vertigo (>95%). | Labyrinthectomy causes total hearing loss in the ear. Nerve section is a major neurosurgical procedure. Reserved for most severe, intractable cases. |
Comparing Meniere’s Disease with Similar Conditions
The symptoms of Meniere’s disease can overlap with other vestibular disorders.
A correct diagnosis is critical. Here’s a comparison table to help differentiate them:
| Feature | Meniere’s Disease | Vestibular Migraine | Benign Paroxysmal Positional Vertigo (BPPV) | Labyrinthitis / Vestibular Neuritis |
|---|---|---|---|---|
| Vertigo Duration | 20 minutes to 12 hours | 5 minutes to 72 hours | Seconds to 1 minute | Days to weeks (constant, then improves) |
| Vertigo Trigger | Spontaneous | Spontaneous, or classic migraine triggers (stress, foods) | Specific head movements (e.g., rolling over in bed) | Spontaneous, often follows a viral illness |
| Hearing Symptoms | Yes: Fluctuating hearing loss, tinnitus, aural fullness | Sometimes (sound sensitivity), but no documented hearing loss | No | Yes (Labyrinthitis): Sudden hearing loss. No (Neuritis): Balance only. |
| Other Symptoms | Nausea, vomiting | Headache, light/sound sensitivity, visual aura | Nausea | Severe nausea, vomiting, imbalance |
| Underlying Cause | Endolymphatic hydrops | Neurological (related to migraine mechanisms) | Dislodged otoconia (calcium crystals) in semicircular canals | Inflammation of inner ear or vestibular nerve, usually viral |
What is the Meniere’s Disease Diet and Does It Work?
One of the cornerstones of conservative management for Meniere’s disease is dietary modification.
The goal of the “Meniere’s disease diet” is to stabilize fluid levels in the body, thereby reducing fluid pressure in the inner ear.
While evidence for its effectiveness is largely anecdotal, many patients report a significant reduction in symptoms by adhering to these guidelines.
The core principles of the diet are:
- Strict Sodium Restriction: This is the most important component. High sodium intake causes the body to retain water, which can increase endolymphatic pressure. The recommendation is to limit sodium intake to 1.500-2.000 milligrams per day. This requires avoiding processed foods, canned soups, fast food, and table salt, and carefully reading food labels.
- Consistent Fluid Intake: It’s crucial to drink an adequate and consistent amount of water throughout the day (e.g., 6-8 glasses). Dehydration can cause the body to retain fluid, and drinking too much at once can cause fluid shifts. The key is consistency.
- Limit or Avoid Caffeine: Caffeine is a stimulant and a diuretic, and its vasoconstrictive properties can potentially reduce blood flow to the inner ear. Its effects on fluid balance can be a trigger for some individuals.
- Limit or Avoid Alcohol: Alcohol can negatively affect inner ear fluid volume and metabolism. It can also act as a direct trigger for vertigo and migraine.
- Avoid MSG (Monosodium Glutamate): Some patients report that MSG, a common food additive, can trigger their symptoms.
- Manage Sugar Intake: Large spikes in blood sugar and insulin can affect fluid and electrolyte balance. Eating regular, balanced meals can help regulate this.
Adherence to this diet requires significant lifestyle changes, but for many, it is a powerful, non-invasive tool for gaining some control over their symptoms.
Living with Meniere’s Disease: Managing Daily Life and Mental Health
The impact of Meniere’s disease extends far beyond its physical symptoms.
The sheer unpredictability of the attacks can create a constant state of anxiety and fear.
As the Cleveland Clinic aptly describes it, “Having Ménière’s disease may feel like you’re being stalked by a disease that jumps out at you when you least expect it”.
This psychological burden is a critical aspect of the condition.
A 2025 study in the journal Psychosocial Status and Quality of Life in Patients With Ménière’s Disease found that the prevalence of anxiety and depression is significantly higher in Meniere’s patients compared to the general population.
Managing this aspect is just as important as treating the physical symptoms.
Strategies for Coping:
- Stress Management: Stress is a major trigger for Meniere’s attacks. Techniques such as psychotherapy (especially Cognitive Behavioral Therapy), mindfulness, meditation, and yoga can be highly effective in managing stress and reducing attack frequency.
- Create a Safe Environment: During an attack, rest is essential. Lie down on a firm surface and focus on a fixed object. Prepare a “go-bag” with acute medications, water, and a sick bag for when you are away from home.
- Plan for Safety: Modify your home to reduce the risk of falls (e.g., remove tripping hazards, install grab bars). Discuss driving safety with your doctor.
- Seek Support: Connecting with others who understand the condition can be immensely helpful. Support groups, either online or in-person, provide a space to share experiences and coping strategies.
- Educate Family and Friends: Help your loved ones understand the condition. Explain what happens during an attack and how they can best support you.
- Vestibular Rehabilitation Therapy (VRT): A physical therapist specializing in VRT can teach you exercises to help your brain adapt to the distorted balance signals from your inner ear. This is particularly useful for managing chronic imbalance between attacks.
What is the Latest Research on Meniere’s Disease?
The field of Meniere’s disease research is more active than ever, with breakthroughs in genetics, immunology, and therapeutics offering new hope.
The focus has shifted from a one-size-fits-all approach to precision medicine, aiming to subtype the disease and target its specific underlying causes.
Key Research Areas:
- Genetics and Genomics: Led by researchers like Professor Jose Antonio Lopez-Escamez, large-scale genomic studies are identifying the genetic architecture of Meniere’s. The 2024 whole genome sequencing study identified 481 high-priority genes and pathways related to cell adhesion and energy maintenance in the inner ear. This work is paving the way for genetic screening and the development of targeted gene therapies.
- Immunology and Inflammation: Research is intensely focused on the inflammatory pathways that contribute to Meniere’s. Studies are profiling the specific cytokines and immune cells involved. The 2025 review on immunological mechanisms discusses how a shift toward a pro-inflammatory M1 macrophage phenotype and the activation of Th17 cells contribute to inner ear damage. This is leading to trials of emerging immunotherapies, including biologics and inflammasome inhibitors, to calm this targeted inflammation.
- Novel Therapeutics: Pharmaceutical companies are developing new drugs. One promising candidate is SPI-1005, an oral medication that has shown in Phase 3 trials to significantly improve hearing loss and tinnitus in Meniere’s patients, as announced by Sound Pharmaceuticals. This represents one of the first potential new treatments to show efficacy for the auditory symptoms of the disease.
- Improved Diagnostics: The NIDCD is supporting research to develop better diagnostic tools, including new ways to measure motion perception and techniques to detect the earliest signs of the disease before it progresses. The refinement of MRI techniques to visualize hydrops is a major part of this effort, allowing for a more objective diagnosis.
These advancements signal a paradigm shift in how Meniere’s disease is understood and treated, moving toward a future where therapies can be personalized to a patient’s specific disease subtype.
Frequently Asked Questions (FAQ)
1. Can Meniere’s disease go away on its own?
Meniere’s disease is a chronic condition with no cure. However, many people experience spontaneous remission, where vertigo attacks stop for long periods. The underlying condition remains, and hearing loss and tinnitus may persist or progress.
2. Is Meniere’s disease fatal?
No, Meniere’s disease is not fatal. Its primary danger comes from the risk of falls and accidents during severe vertigo attacks, particularly “drop attacks”. Managing the condition is focused on symptom control and safety.
3. Can I drive if I have Meniere’s disease?
Driving safety is a major concern. You should not drive during an acute vertigo attack or if you feel dizzy. Discuss your specific symptoms and local regulations with your doctor to determine if and when it is safe for you to drive.
4. Does stress cause Meniere’s disease?
Stress does not cause Meniere’s disease, but it is a very common and powerful trigger for attacks. Effectively managing stress through therapy, meditation, or other relaxation techniques is a key part of controlling the disease’s symptoms.
5. Will I go completely deaf from Meniere’s disease?
While Meniere’s disease causes progressive sensorineural hearing loss in the affected ear, it rarely leads to total deafness. The hearing loss is typically severe to profound. If the disease becomes bilateral, the impact on hearing is more significant.
6. Is flying in an airplane safe with Meniere’s disease?
Flying is generally safe, but pressure changes during takeoff and landing can trigger symptoms like aural fullness or dizziness for some. Using earplugs designed for pressure regulation or taking a decongestant may help.
7. What is the difference between dizziness and vertigo?
Dizziness is a general term for feelings of lightheadedness, faintness, or unsteadiness. Vertigo is a specific type of dizziness characterized by a rotational or spinning sensation, where you feel that you or your surroundings are moving.
8. Can Meniere’s disease affect both ears?
Yes. While it usually starts in one ear, Meniere’s can become bilateral over time. Estimates vary, but it may affect the second ear in 15-40% of patients, sometimes years after the initial onset.
Conclusion
Meniere’s disease is a complex and often frustrating journey, marked by the unpredictable nature of its symptoms.
While there is currently no cure, a diagnosis is not the end of the road.
As we’ve explored, a wealth of strategies exists to manage this condition, from foundational lifestyle and dietary changes to advanced medical and surgical interventions.
The future is bright, with ongoing research rapidly uncovering the genetic and immunological roots of the disease, paving the way for more targeted and effective therapies.
The most powerful tool you have is knowledge. By understanding your symptoms, identifying your triggers, and working closely with a knowledgeable healthcare team, you can significantly reduce the impact of Meniere’s disease on your life.
Building a strong support system and prioritizing your mental health are equally crucial steps in navigating the challenges of this chronic condition.
Your journey is unique. We encourage you to take this information to your doctor to create a personalized management plan. If you have experience with Meniere’s disease, please consider sharing your story or tips in the comments below to help others in this community.
Medical Disclaimer: The information on this page is for educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.

