Experiencing memory loss can be unsettling, sparking fears about aging and serious conditions.
However, memory lapses can stem from many sources, ranging from normal, manageable age-related changes and treatable medical conditions to more serious neurodegenerative diseases like Alzheimer’s.
Understanding the cause is the first step toward managing symptoms and seeking appropriate care.
While it’s a significant concern, it’s important to know that not all forgetfulness signals a dire diagnosis.
According to the Alzheimer’s Association, while over 11% of people age 65 and older have Alzheimer’s dementia, many instances of forgetfulness are due to reversible causes.
This guide will help you distinguish normal forgetfulness from concerning symptoms, explore surprising reversible causes of memory loss like stress and medications, clarify the differences between conditions like Mild Cognitive Impairment (MCI) and dementia, and provide a clear action plan for when and how to seek medical help.
This guide will walk you through the possibilities, helping you understand the changes you’re experiencing and what steps to take next.
In This Article
Is My Memory Loss Just a Normal Part of Aging?
One of the most common anxieties surrounding memory is whether a lapse is a normal “senior moment” or a sign of something more serious.
The distinction is crucial. While some cognitive changes are a natural part of the aging process, significant memory loss that disrupts daily life is not.
Defining Normal Age-Related Forgetfulness
As we grow older, our brains change, and it can take longer to learn new information or recall familiar names and words.
This is often referred to as age-associated memory impairment.
According to the National Institute on Aging, these typical changes are generally manageable and do not prevent you from living a full, independent life.
Examples of normal age-related memory changes include:
- Occasionally forgetting a name or an appointment, but remembering it later.
- Sometimes misplacing things like glasses or keys.
- Finding you need to make lists more often to remember tasks.
- Experiencing a “tip-of-the-tongue” phenomenon, where you struggle to find the right word but it comes to you eventually.
These moments can be frustrating, but they don’t typically signal a significant decline in your ability to work, maintain relationships, or manage your day-to-day responsibilities.
What’s Happening in the Aging Brain?
The aging process brings subtle physiological changes to the brain.
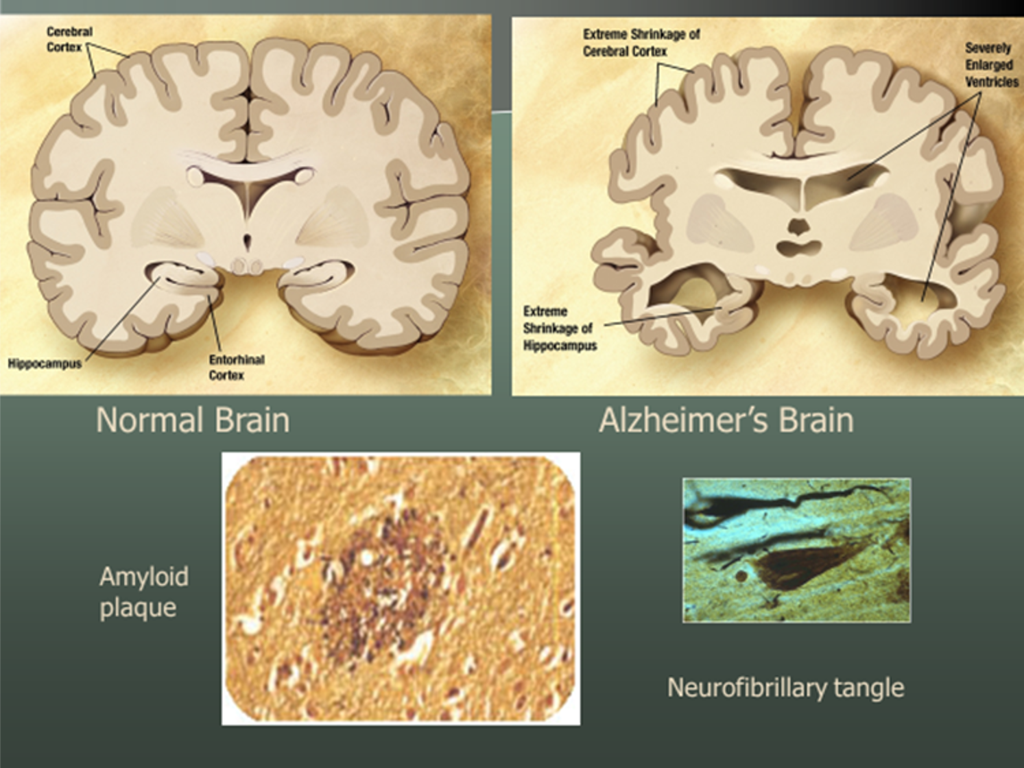
The hippocampus and other brain regions involved in learning and memory can experience some shrinkage.
Hormones and proteins that protect and repair brain cells and stimulate neural growth may also decline.
Furthermore, blood flow to the brain can decrease.
These physical changes can slow down cognitive processing, making it harder to multitask or retrieve information as quickly as you did when you were younger.
It’s not that the information is gone, but rather that the brain’s filing and retrieval system has become slightly less efficient.
Comparative Table: Normal Aging vs. Cause for Concern
To help clarify the difference, it’s useful to compare typical age-related changes with the more concerning symptoms that may indicate a condition like dementia.
This table, based on guidance from health organizations like the Mayo Clinic and the Alzheimer’s Association, provides a scannable overview.
| Symptom / Behavior | Normal Age-Related Change | Potential Sign of a Problem |
|---|---|---|
| Forgetting Things | Occasionally forgetting names or appointments but remembering them later. | Forgetting recently learned information, important dates, or asking for the same information repeatedly. |
| Problem-Solving | Making an occasional error when balancing a checkbook. | Trouble following a familiar recipe or keeping track of monthly bills. |
| Daily Tasks | Sometimes needing help to use the settings on a microwave. | Difficulty completing familiar tasks at home, work or leisure. |
| Losing Things | Misplacing things from time to time and being able to retrace steps to find them. | Putting things in unusual places (e.g., wallet in the freezer) and being unable to find them. |
| Judgment | Making a bad decision once in a while. | Showing consistently poor judgment, especially with money or personal hygiene. |
| Mood & Personality | Sometimes feeling weary of work or social obligations. | Withdrawing from social activities, showing changes in mood like confusion, suspicion, depression or anxiety. |
Could My Lifestyle or a Medical Condition Be the Culprit? (Reversible Causes)
Before jumping to conclusions about dementia, it’s vital to explore the many reversible factors that can cause memory loss.
Many people are surprised to learn that their forgetfulness is a symptom of a treatable condition.
Addressing these underlying issues can often lead to a significant improvement in cognitive function.
Emotional and Mental Health: Stress, Anxiety and Depression
The mind and body are deeply connected. Emotional distress can take a significant toll on your cognitive abilities.
When you are under chronic stress or experiencing anxiety, your brain is flooded with the stress hormone cortisol.
Research has shown that prolonged exposure to high cortisol levels can damage and shrink the hippocampus, the brain’s memory center.
This makes it difficult to form new memories or retrieve old ones.
Similarly, depression can cause memory loss by disrupting brain circuits responsible for attention and focus.
If you can’t concentrate on information, you can’t encode it into memory effectively.
This can manifest as what feels like short-term memory loss.
The good news is that treating the underlying depression or anxiety often restores cognitive function.
The Critical Role of Sleep
Sleep is not a passive state, it’s when your brain works hard to consolidate memories, moving them from fragile, short-term storage to more robust, long-term storage.
When you don’t get enough quality sleep, this crucial process is impaired.
You might wake up feeling foggy and find it hard to concentrate or remember new things.
A particularly common and underdiagnosed culprit is sleep apnea, a condition where breathing repeatedly stops and starts during sleep.
This deprives the brain of oxygen and severely fragments sleep.
The Mayo Clinic notes that untreated sleep apnea can significantly affect memory, but these effects can often be improved with treatment, such as using a CPAP (Continuous Positive Airway Pressure) machine.

Medications That Can Affect Memory
A surprising number of common prescription and over-the-counter medications can interfere with memory.
They can cause confusion, fogginess, or forgetfulness as a side effect.
If your memory problems started after beginning a new medication, it’s a crucial piece of information to discuss with your doctor.
Classes of drugs that may affect memory include:
- Anticholinergics: These drugs block acetylcholine, a key neurotransmitter for memory and learning. They are found in some medications for incontinence, COPD and allergies.
- Benzodiazepines: Used for anxiety and insomnia (e.g., Xanax, Valium), these can interfere with the transfer of information from short-term to long-term memory.
- Opioid Painkillers: These can cause drowsiness and mental fog, impacting memory.
- Certain Antidepressants: Some older tricyclic antidepressants can have anticholinergic effects.
- Sleep Aids: Both prescription and over-the-counter sleep aids can cause next-day grogginess and memory issues.
Important Disclaimer: Never stop taking a prescribed medication without consulting your doctor. Abruptly stopping some drugs can be dangerous. Discuss your concerns with your healthcare provider, who can determine if an alternative medication or a dosage adjustment is appropriate.
Nutritional and Vitamin Deficiencies
Your brain requires a steady supply of nutrients to function optimally.
A deficiency in Vitamin B-12 is a well-known cause of reversible memory problems.
Vitamin B-12 is essential for maintaining healthy nerve cells. A deficiency can lead to nerve damage that mimics dementia symptoms.
This is particularly common in older adults, as the ability to absorb B-12 from food can decrease with age.
Vegetarians and vegans are also at higher risk.
A simple blood test can detect a B-12 deficiency, which can often be corrected with supplements or injections.
Other Reversible Medical Conditions
Several other medical issues can present with dementia-like symptoms, including memory loss:
- Hypothyroidism: An underactive thyroid gland can slow down the body’s metabolism, including brain processes, leading to forgetfulness and mental sluggishness.
- Minor Head Injury: A fall or accident, even without loss of consciousness, can cause temporary memory problems.
- Infections: Certain infections, such as a urinary tract infection (UTI) in older adults, can cause sudden confusion and memory issues, a state known as delirium.
- Brain Tumors: While rare, a tumor can press on brain areas responsible for memory, causing symptoms.
Alcohol and Substance Use
Excessive alcohol consumption can directly interfere with short-term memory, causing “blackouts”.
Over the long term, chronic alcohol abuse can lead to serious and sometimes permanent brain damage, including conditions like Wernicke-Korsakoff syndrome, which severely impairs memory.
Alcohol can also cause memory loss by interacting with medications.
Reducing or eliminating alcohol can often improve cognitive function.
What Is Mild Cognitive Impairment (MCI)?
Between the poles of normal age-related forgetfulness and severe dementia lies a condition known as Mild Cognitive Impairment (MCI).
This “in-between” stage is a common source of concern and confusion, as it represents a decline that is noticeable but not yet debilitating.
Defining the Symptoms of MCI
MCI is characterized by a measurable decline in at least one cognitive area, such as memory, language, or judgment, that is greater than what’s expected for a person’s age and education level.
However, as the Mayo Clinic explains, these cognitive changes are not severe enough to interfere with independent daily activities.
A person with MCI might forget conversations or appointments more frequently, but they can still manage their finances, drive, and live on their own.
The experience of living with or caring for someone with MCI can be frustrating.
As one caregiver on the Mayo Clinic Connect forum shared, the subtlety of the decline can make it difficult to get a definitive diagnosis, as the individual may still perform well on simple in-office cognitive tests, leaving families feeling unheard.
Does MCI Always Lead to Dementia?
A diagnosis of MCI understandably raises fears about the future.
While it is true that individuals with MCI have an increased risk of progressing to dementia, particularly Alzheimer’s disease, this is not an inevitable outcome.
For some people, MCI remains stable for years. In other cases, especially when the MCI is linked to a reversible cause like depression, medication side effects, or sleep apnea, the cognitive decline may improve or even resolve once the underlying issue is treated.
This is why a thorough medical evaluation for MCI is so critical—it offers a window of opportunity for intervention.
How Is Dementia Different from Normal Memory Loss?
While “dementia” is often used interchangeably with “memory loss”, the terms are not synonymous.
Understanding dementia as a clinical syndrome is key to recognizing its gravity and distinguishing it from the more benign forms of forgetfulness.
Understanding Dementia: An Umbrella Term for Symptoms
Dementia is not a single disease. It is an umbrella term used to describe a set of symptoms caused by various disorders affecting the brain.
These symptoms involve a decline in mental ability severe enough to interfere with daily life.
As the National Institute on Aging clarifies, memory loss is a common symptom, but it is not the only one.
Other symptoms include difficulties with:
- Language: Trouble finding the right words or understanding conversations.
- Reasoning and Judgment: Difficulty with planning, organizing, or making decisions.
- Visual Perception: Problems judging distances or identifying objects.
- Attention and Focus: Inability to concentrate or follow a multi-step task.
Unlike normal age-related memory changes, dementia is progressive, meaning the symptoms start slowly and gradually worsen over time.
Alzheimer’s Disease: The Most Common Cause
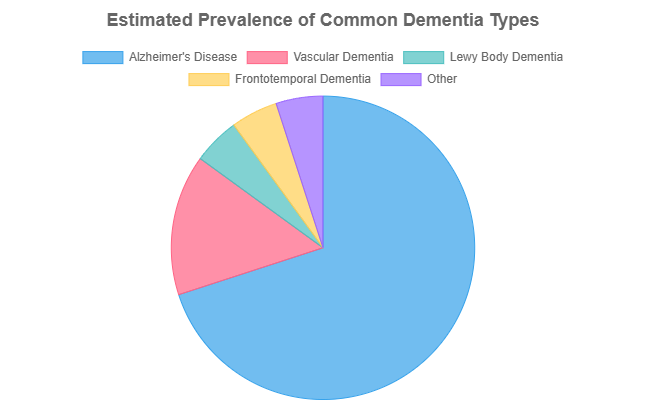
Alzheimer’s disease is the most common cause of dementia, accounting for an estimated 60-80% of cases.
It is a progressive brain disorder that slowly destroys memory and thinking skills.
The disease is characterized by two hallmark pathologies: amyloid plaques (clumps of protein that build up between nerve cells) and tau tangles (twisted fibers of another protein that build up inside cells).
These plaques and tangles disrupt communication between neurons and trigger an inflammatory response, eventually leading to cell death and brain shrinkage.
Vascular Dementia: The Link to Brain Blood Flow
Vascular dementia is the second most common type. It is caused by conditions that damage blood vessels in the brain and disrupt the flow of blood and oxygen, such as a major stroke or multiple small, often unnoticed, strokes.
Symptoms can appear suddenly after a stroke or develop gradually over time.
The pattern of symptoms depends on which part of the brain is affected. Adding to the complexity, recent research demonstrates that different patterns of cerebral blood flow (CBF) can indicate different subtypes of cognitive decline.
A study published in Dementia and Geriatric Cognitive Disorders Extra used machine learning to identify distinct CBF patterns in patients with memory loss, suggesting that imaging blood flow could have clinical utility in diagnosing and subtyping conditions like Alzheimer’s and vascular dementia .
Other Common Dementias
Several other diseases also cause dementia, each with unique features:
- Lewy Body Dementia (LBD): This condition is characterized by the presence of abnormal protein deposits called Lewy bodies. In addition to memory loss, LBD often involves significant fluctuations in attention and alertness, visual hallucinations, and movement symptoms similar to Parkinson’s disease.
- Frontotemporal Dementia (FTD): FTD refers to a group of disorders caused by the progressive loss of nerve cells in the brain’s frontal or temporal lobes. Unlike Alzheimer’s, FTD often strikes at a younger age and typically causes dramatic changes in personality, behavior and language skills before significant memory loss occurs.
Mixed Dementia
In many older adults, it is common for the brain changes of more than one type of dementia to be present simultaneously—a condition known as mixed dementia.
For example, a person may have the plaques and tangles of Alzheimer’s disease along with the blood vessel damage of vascular dementia.
The presence of multiple pathologies can result in a more severe and rapid decline than either condition would cause alone.
When and How to Seek Medical Help
Recognizing that memory changes are interfering with your life is the first step.
The next, and most crucial, is to seek a professional medical evaluation.
This can be an intimidating process, but being prepared can empower you to get the answers and support you need.
When Should I See a Doctor About Memory Loss?
It’s time to make an appointment if you or your loved ones notice symptoms that go beyond occasional forgetfulness.
According to the Alzheimer’s Association, you should seek help if memory problems are causing concern. Key red flags include:
- Memory loss that disrupts your daily life (e.g., affecting your job or ability to manage finances).
- Frequently asking the same questions or repeating stories.
- Difficulty completing familiar tasks, like following a recipe or driving to a known location.
- Getting lost in familiar places or feeling disoriented about time and place.
- Family or friends have expressed concern about your memory.
- Noticeable changes in mood, personality, or judgment.
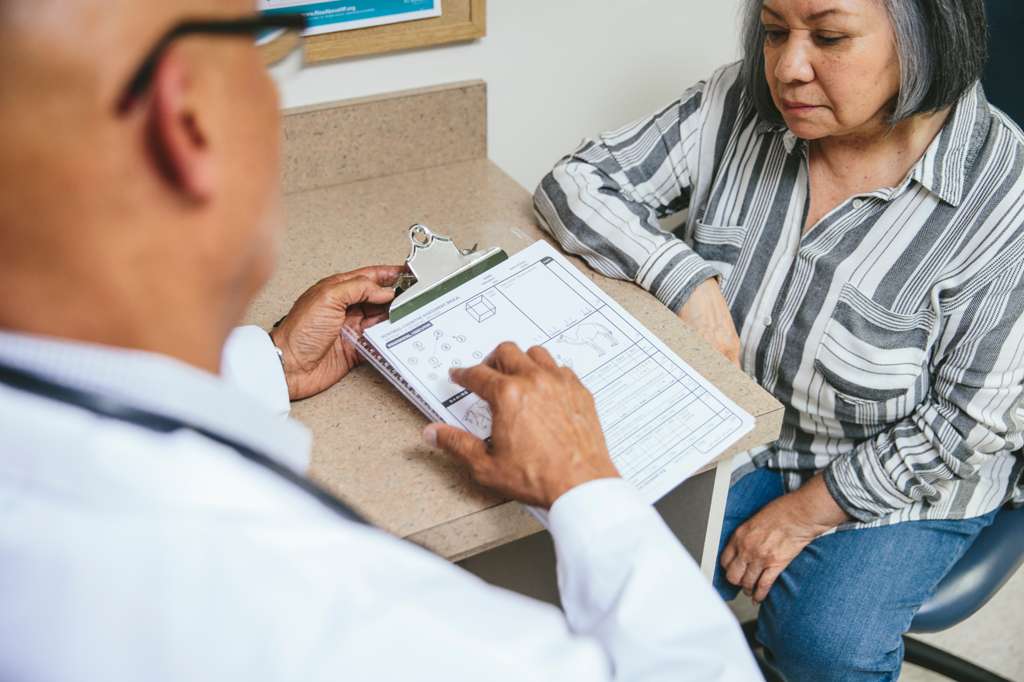
How Do I Prepare for a Doctor’s Visit?
A productive doctor’s visit starts with good preparation. Your doctor will need detailed information to assess your situation.
It’s recommended to bring a trusted family member or friend who can provide observation and support.
What to Track and Bring:
- A list of all medications: Include prescriptions, over-the-counter drugs, vitamins, and supplements, along with their dosages.
- A log of symptoms: Write down specific examples of memory lapses or other cognitive difficulties. When did they start? How often do they happen?
- Medical history: Be ready to discuss your personal and family medical history, including any history of dementia, heart disease, or stroke.
- Recent life events: Mention any recent illnesses, injuries, or major stressful events.
- A list of questions: Prepare questions in advance so you don’t forget to ask them.
Questions to Ask Your Doctor:
Empower yourself by asking direct questions. Consider these starters:
- “Are my symptoms consistent with normal aging, or could this be something more?”
- “Could any of my current health conditions or medications be causing or contributing to my memory loss?”
- “What tests do you recommend to help determine the cause?”
- “Based on my symptoms, should I see a specialist, such as a neurologist or geriatrician?”
- “What resources are available to help me and my family?”
How Do Doctors Diagnose the Cause of Memory Loss?
There is no single test for memory loss. A diagnosis is a process of elimination, aimed at identifying the underlying cause, whether it’s reversible or progressive.
The Diagnostic Process:
The evaluation typically begins with a thorough medical history and a physical exam.
The core of the assessment often involves cognitive and neuropsychological testing.
These tests use a series of questions and simple tasks to evaluate memory, problem-solving skills, language, and other cognitive functions.
This helps the doctor gauge the severity and pattern of the impairment.
The Role of Lab Tests and Brain Imaging:
To rule out reversible causes, your doctor will likely order blood tests to check for vitamin B-12 deficiency, thyroid problems, and other metabolic issues.
Brain imaging, such as a CT scan or MRI, can help identify evidence of strokes, tumors, fluid buildup, or patterns of brain shrinkage (atrophy) that might suggest a specific type of dementia.
Why an Early and Accurate Diagnosis Is Crucial:
While the prospect of a diagnosis can be frightening, obtaining one early is incredibly beneficial. It allows you to:
- Get treatment for reversible conditions: Identifying and treating a condition like sleep apnea or a vitamin deficiency can potentially restore your cognitive function.
- Begin treatments to manage symptoms: For progressive dementias, an early diagnosis allows you to start medications and therapies that may help manage symptoms and preserve function for a time.
- Plan for the future: It provides an opportunity to make important legal, financial, and long-term care decisions while you are still able to do so.
- Access support: You and your family can connect with resources and support services, such as those offered by the Alzheimer’s Association.
What Are the Treatments and Strategies for Managing Memory Loss?
The approach to managing memory loss depends entirely on its cause.
While there is no “cure” for many forms of memory loss, a wide range of treatments, strategies, and lifestyle changes can help manage symptoms, support brain health, and improve quality of life.
Addressing Reversible Causes
As discussed earlier, if your memory loss is caused by an underlying medical condition, treatment is focused on that specific issue.
This is the most optimistic scenario for memory loss treatment. For example:
- Vitamin B-12 deficiency is treated with supplements or injections.
- Hypothyroidism is managed with thyroid hormone medication.
- Sleep apnea is treated with a CPAP device or other interventions.
- Medication-induced memory loss may be resolved by switching to a different drug under a doctor’s supervision.
Medications for Dementia
For progressive dementias like Alzheimer’s disease, there is currently no cure.
However, several medications are approved by the FDA to help manage cognitive and behavioral symptoms.
Cholinesterase inhibitors (e.g., donepezil) can help with memory and thinking for a time by boosting levels of a key neurotransmitter.
Other medications may target specific pathologies, such as amyloid plaques.
These drugs do not stop or reverse the disease, but they can slow the progression of symptoms in some individuals, providing valuable time.
The Power of Lifestyle Interventions
Regardless of the cause of memory loss, a brain-healthy lifestyle is a cornerstone of management and prevention.
Evidence strongly suggests that what’s good for the heart is good for the brain.
- Physical Exercise: Regular aerobic exercise increases blood flow to the brain, which delivers vital oxygen and nutrients. It has been shown to help maintain brain function and may reduce the risk of cognitive decline.
- Healthy Diet: Diets rich in fruits, vegetables, whole grains, and healthy fats, such as the Mediterranean or MIND diets, have been linked to better cognitive outcomes and a lower risk of dementia.
- Mental Engagement: The “use it or lose it” principle applies to the brain. Staying mentally active by learning new skills, playing challenging games, reading, or engaging in hobbies can help build cognitive reserve.
- Social Connection: Maintaining strong social ties and engaging in community activities is associated with a lower risk of cognitive decline. Social interaction challenges the brain and can help reduce stress.
The Future of Treatment: A Glimpse into Research
The field of neuroscience is advancing rapidly, offering hope for more effective treatments in the future.
Scientists are exploring innovative approaches that go beyond managing symptoms to targeting the root causes of neurodegeneration.
For instance, one promising area of research involves using exosomes—tiny vesicles released by cells that can carry proteins and other molecules.
A 2025 review in the Journal of Molecular Neuroscience highlights how stem cell-derived exosomes may help clear harmful amyloid proteins and reduce inflammation in the brain.
This research suggests that exosome-based therapeutics could one day become a transformative approach in Alzheimer’s therapy .
While still in the research phase, such advancements underscore the importance of continued scientific investment.
Frequently Asked Questions (FAQ)
1. Can stress cause permanent memory loss?
Chronic stress can damage the brain’s memory center, but this is often not permanent. Managing stress through therapy, exercise, and relaxation techniques can improve focus and memory function. Permanent damage from stress alone is rare.
2. What is the difference between short-term and long-term memory loss?
Short-term memory loss involves forgetting recent events, like what you just ate. Long-term memory loss affects recall of past events, facts, and skills. Conditions like Alzheimer’s typically impact short-term memory first.
3. At what age is memory loss considered normal?
Mild forgetfulness, like taking longer to recall a name, can be a normal part of aging, often starting in one’s 50s or 60s. However, memory loss that disrupts daily life is not normal at any age and warrants a doctor’s visit.
4. Can memory loss be reversed?
Yes, when memory loss is caused by treatable factors like vitamin deficiencies (B-12), thyroid problems, sleep apnea, depression, or medication side effects, it can often be reversed or significantly improved by addressing the underlying issue.
5. How can I improve my memory naturally?
A brain-healthy lifestyle is key. This includes regular physical exercise, a balanced diet (like the Mediterranean diet), getting quality sleep, staying socially active, and challenging your mind with new activities like learning an instrument or language.
6. Does COVID-19 cause memory loss or “brain fog”?
Yes, many people report “brain fog“, including memory problems and difficulty concentrating, after a COVID-19 infection. The exact causes are still being studied, but it’s believed to be related to inflammation, vascular issues, or a direct viral effect on the brain.
7. What is often the first sign of dementia?
For Alzheimer’s disease, the most common type of dementia, the first sign is typically difficulty remembering newly learned information. For other dementias, like FTD, the first signs might be changes in personality or behavior.
8. Is there a single blood test for Alzheimer’s?
While there is no single diagnostic blood test yet, new blood tests that can detect biomarkers like amyloid and tau are becoming available. They are used to help confirm a diagnosis made through a comprehensive clinical evaluation, not as a standalone test.
Conclusion
Memory loss exists on a wide spectrum, from the normal, minor frustrations of aging to the life-altering symptoms of dementia.
This guide has shown that many causes are treatable, and that even for progressive conditions, there are effective strategies for management and support.
The most critical takeaway is that distinguishing between these possibilities requires professional medical guidance.
Experiencing changes in your memory can be deeply unsettling, but ignoring them out of fear or uncertainty is not the answer.
Seeking clarity is a proactive and positive step toward taking control of your health.
An accurate diagnosis is the essential key that unlocks the door to the right support, appropriate treatment, and peace of mind for you and your family.
If you are concerned about your memory or the memory of a loved one, the most important step is to schedule an appointment with a doctor.
We invite you to share your experiences or questions in the comments below to connect with others who may be on a similar journey. Your story could provide comfort and insight to someone else navigating these same concerns.

