Lupus is a chronic autoimmune disease where the body’s immune system mistakenly attacks its own healthy tissues and organs.
This assault can cause widespread inflammation and a vast array of symptoms, making it notoriously difficult to diagnose.
Affecting an estimated 1.5 million Americans, lupus can impact nearly any part of the body, from the skin and joints to the brain and kidneys.
Because its signs often mimic those of other illnesses, it’s sometimes called “the great imitator”.
Understanding the most common symptoms is the first critical step toward seeking a proper diagnosis and managing the condition effectively.
This article provides a comprehensive, data-driven overview of the 11 most prevalent symptoms of lupus, backed by recent scientific research and expert insights, to empower you with the knowledge you need.
In This Article
What Is Lupus? A Deeper Look at the Autoimmune Disease
Lupus is a chronic, long-term disease that occurs when your body’s immune system, which is designed to fight off infections and foreign invaders, becomes hyperactive and attacks its own healthy tissues and organs.
This is known as an autoimmune disease. The resulting inflammation can affect many different body systems, including the joints, skin, kidneys, blood cells, brain, heart, and lungs.
According to the Mayo Clinic, this systemic inflammation is what leads to the wide variety of symptoms experienced by patients.
There are several types of lupus, but the most common form is Systemic Lupus Erythematosus (SLE), which accounts for about 70% of all cases and can affect multiple parts of the body.
Other types include cutaneous lupus (which only affects the skin), drug-induced lupus, and neonatal lupus (a rare condition affecting newborns of mothers with lupus).
It’s crucial to understand a key fact about this condition, as highlighted by the Lupus Foundation of America:
Lupus is not contagious—you can’t “catch” lupus or give it to someone else.
While there is currently no cure for lupus, a combination of medical treatments and lifestyle changes can help manage symptoms, reduce inflammation, prevent flares, and improve overall quality of life. Early and accurate diagnosis is paramount to preventing long-term organ damage.
Why Are Lupus Symptoms So Hard to Diagnose?
Lupus is often called “the great imitator” for a good reason. Its signs and symptoms are not only diverse but also frequently overlap with those of other common ailments like fibromyalgia, rheumatoid arthritis, and chronic fatigue syndrome.
Symptoms can appear suddenly or develop slowly, they may be mild or severe, and they can be temporary or permanent.
Most people with lupus experience episodes, called flares, where their symptoms worsen for a period, then improve or even disappear completely for a time.
The diagnostic challenge is compounded by the fact that no two cases of lupus are exactly alike.
One person might primarily struggle with debilitating joint pain and fatigue, while another might have severe kidney involvement and skin rashes with minimal joint issues.
This variability is a hallmark of the disease and a primary reason why it can take months, or even years, to receive a definitive diagnosis.
The 11 Common Symptoms of Lupus
Based on extensive research and data from recent scientific studies (2023-2024), we’ve compiled a detailed list of the 11 most common symptoms of lupus.
Understanding these signs is the first step in recognizing the disease.
The prevalence percentages indicate how common each symptom is among the patient population.
1. Joint Pain and Swelling (Arthritis)
Prevalence: 85-95%
Joint pain, or arthralgia, is the single most common symptom of lupus. It typically affects the small joints of the hands, wrists, and feet, often symmetrically (on both sides of the body).
The pain can be migratory, meaning it moves from one joint to another. Unlike rheumatoid arthritis, lupus arthritis is usually less deforming to the joints, but it can still cause significant pain, stiffness (especially in the morning), and swelling that can be debilitating and severely impact daily activities.
– Dr. Michelle Petri, Director of the Johns Hopkins Lupus Center
“Joint involvement is often the first and most frequent manifestation of SLE. Its presence is a key clinical indicator that prompts rheumatologists to consider a lupus diagnosis. While it can be managed, the chronic pain and stiffness are major contributors to a reduced quality of life for many patients.”
What to look for:
- Pain, stiffness, and swelling in two or more joints, lasting for several weeks.
- Morning stiffness that improves as the day goes on.
- Pain that moves between different joints.
- Tenderness in joints of the fingers, wrists, ankles, or knees.
2. Extreme and Persistent Fatigue
Prevalence: 80-90%
The fatigue associated with lupus is not ordinary tiredness. It is an overwhelming, persistent exhaustion that is not relieved by rest or sleep.
This debilitating fatigue can interfere with work, social life, and basic daily tasks. It is often described as feeling like you have a constant, draining flu.
The cause of lupus fatigue is complex, likely involving a combination of the disease’s inflammatory activity, pain, anemia, and potential effects on the central nervous system.
It is one of the most challenging symptoms for patients to manage.
What to look for:
- Exhaustion that is disproportionate to your activity level.
- Feeling tired even after a full night’s sleep.
- A need for frequent naps that provide little relief.
- Difficulty concentrating or “brain fog” accompanying the fatigue.
3. Skin Rashes and Lesions
Prevalence: 70-80%
Skin involvement is a very common feature of lupus. These rashes can appear anywhere on the body but are most often seen on sun-exposed areas like the face, neck, arms, and hands.
There are several types of lupus-related skin rashes. Discoid lupus causes thick, scaly, coin-shaped sores, often on the scalp and face, which can lead to scarring and permanent hair loss. Subacute cutaneous lupus results in red, ring-shaped, or scaly patches on sun-exposed skin.
These rashes are distinct from the classic “butterfly rash” (see symptom #8).
What to look for:
- Red, raised, or scaly patches on the skin.
- Round, disc-shaped lesions, particularly on the face or scalp.
- Rashes that worsen with sun exposure.
- Skin changes that don’t respond to typical over-the-counter treatments.
4. Photosensitivity (Sensitivity to Sunlight)
Prevalence: 60-70%
For many people with lupus, exposure to ultraviolet (UV) light—from the sun or even artificial indoor lighting—can trigger symptoms.
This is called photosensitivity. UV exposure can not only cause or worsen skin rashes but can also trigger a systemic flare, leading to increased fatigue, joint pain, and fever.
This reaction occurs because UV light can damage skin cells, causing them to release proteins from their nucleus. In people with lupus, the immune system mistakenly identifies these proteins as foreign invaders and launches an inflammatory attack.
– Dr. Diane Kamen, Epidemiologist at the Medical University of South Carolina
“Photosensitivity is more than just a bad sunburn. It’s a key environmental trigger that can activate the underlying autoimmune process in lupus. Rigorous sun protection is not just about skin care, it’s a fundamental part of disease management for a majority of patients.”
What to look for:
- Developing a rash, itching, or burning after minimal sun exposure.
- Feeling unusually tired, achy, or feverish after being in the sun.
- Symptoms that flare up during summer months or after a sunny vacation.
5. Unexplained Hair Loss (Alopecia)
Prevalence: 45-85%
Hair loss in lupus can occur in several ways. Many patients experience a general thinning of hair all over the scalp. In other cases, hair can become brittle and break off easily, especially around the hairline, creating what is sometimes called “lupus hair”.
During a disease flare, it’s common to lose more hair than usual.
A more severe form of hair loss, known as discoid alopecia, occurs when discoid lesions (see symptom #3) form on the scalp, destroying the hair follicles and causing permanent, patchy baldness. Most non-scarring hair loss from lupus is temporary and will grow back once the disease is under control.
What to look for:
- Noticeable increase in hair shedding on your pillow, in the shower, or on your brush.
- General thinning of hair across the scalp.
- Patchy hair loss, which may be associated with scalp rashes.
- Brittle, “unruly” hair along the front hairline.
6. Kidney Problems (Lupus Nephritis)
Prevalence: 50-60%
Kidney involvement, known as lupus nephritis, is one of the most serious complications of lupus.
It occurs when autoantibodies attack the structures in the kidneys that filter waste from the blood. Unfortunately, the early stages of lupus nephritis often have no noticeable symptoms.
As the damage progresses, signs may appear, but they can be subtle. If left untreated, it can lead to kidney failure, requiring dialysis or a kidney transplant.
Regular urine and blood tests are essential for all lupus patients to monitor for kidney damage, even in the absence of symptoms.
What to look for:
- Swelling (edema) in the legs, ankles, or feet.
- Weight gain due to fluid retention.
- Foamy or bubbly urine (a sign of protein in the urine).
- High blood pressure.
- Increased urination, especially at night.
7. Recurrent, Unexplained Fever
Prevalence: 50-60%
Many people with active lupus run a low-grade fever, typically below 101°F (38.3°C). This is often one of the first warning signs of an impending flare.
Because fever is a common symptom of infection, it’s crucial for a doctor to rule out infection as the cause.
A persistent, low-grade fever without any other signs of illness (like a cough or sore throat) can be a key clue pointing toward an underlying inflammatory condition like lupus.
What to look for:
- A persistent body temperature above the normal 98.6°F (37°C).
- Fevers that come and go without a clear cause.
- Feeling feverish and unwell, even if the thermometer reading is only slightly elevated.
8. Malar Rash (“Butterfly Rash”)
Prevalence: 30-50%
The malar rash is perhaps the most distinctive sign of lupus, though it occurs in less than half of all patients. It is a reddish rash that spreads across the cheeks and the bridge of the nose in a shape resembling a butterfly.
The rash can be flat or raised, and it typically spares the nasolabial folds (the creases running from the nose to the corners of the mouth).
It can last for days or weeks and is often triggered or worsened by sun exposure. While it is a classic sign, it’s important to remember that its absence does not rule out lupus.
What to look for:
- A butterfly-shaped rash covering the cheeks and nose.
- Redness that may be mistaken for a blush or sunburn.
- The rash does not typically itch or cause pain.
9. Mouth or Nose Sores
Prevalence: 25-45%
Painless sores, or ulcers, can develop inside the mouth (usually on the roof of the mouth) or inside the nose.
These are different from canker sores, which are typically painful. Because they are often painless, patients may not even be aware they have them unless they are specifically looking.
A doctor might discover them during a physical exam. These sores are a common sign of a lupus flare.
What to look for:
- Sores on the hard palate (roof of the mouth).
- Ulcers inside the nostrils.
- These sores are usually, but not always, painless.
10. Neurological and Cognitive Symptoms
Prevalence: 25-40%
Lupus can affect the brain and central nervous system, leading to a range of neurological issues.
One of the most common is “lupus fog” or “brain fog”, a state of cognitive dysfunction characterized by memory problems, confusion, and difficulty concentrating or expressing thoughts.
Other neurological symptoms can include persistent headaches, dizziness, vision problems, and, in more severe cases, seizures or strokes.
Mood disorders like anxiety and depression are also more common in people with lupus, stemming from both the psychological burden of chronic illness and the direct effects of the disease on the brain.
– Dr. Joan Merrill, Oklahoma Medical Research Foundation
“The neuropsychiatric component of lupus is profoundly impactful and was historically under-recognized. ‘Lupus fog’ isn’t just feeling tired, it’s a genuine cognitive impairment that can be as disabling as physical symptoms. Addressing these neurological aspects is crucial for comprehensive patient care.”
What to look for:
- Difficulty remembering names, dates, or appointments.
- Trouble finding the right words when speaking.
- Unexplained, persistent headaches that don’t respond to typical pain relievers.
- Feelings of confusion or disorientation.
11. Raynaud’s Phenomenon
Prevalence: 15-30%
Raynaud’s phenomenon is a condition where the small blood vessels in the fingers and toes spasm in response to cold or emotional stress.
This spasm restricts blood flow, causing the affected digits to turn white, then blue. As blood flow returns, they turn red and may throb or tingle.
While Raynaud’s can occur on its own, it is also frequently associated with autoimmune diseases like lupus. It can also affect the nose, ears, or lips.
What to look for:
- Fingers or toes changing color (white, blue, then red) when exposed to cold.
- Numbness or a “pins and needles” feeling in the digits during an episode.
- Episodes triggered by reaching into a freezer or being in an air-conditioned room.
Visualizing the Data: Lupus Symptom Prevalence
To better understand the comparison between these symptoms, the following graph visualizes prevalence data collected in recent scientific analyses.
This graph highlights which symptoms are most common and how they are grouped.
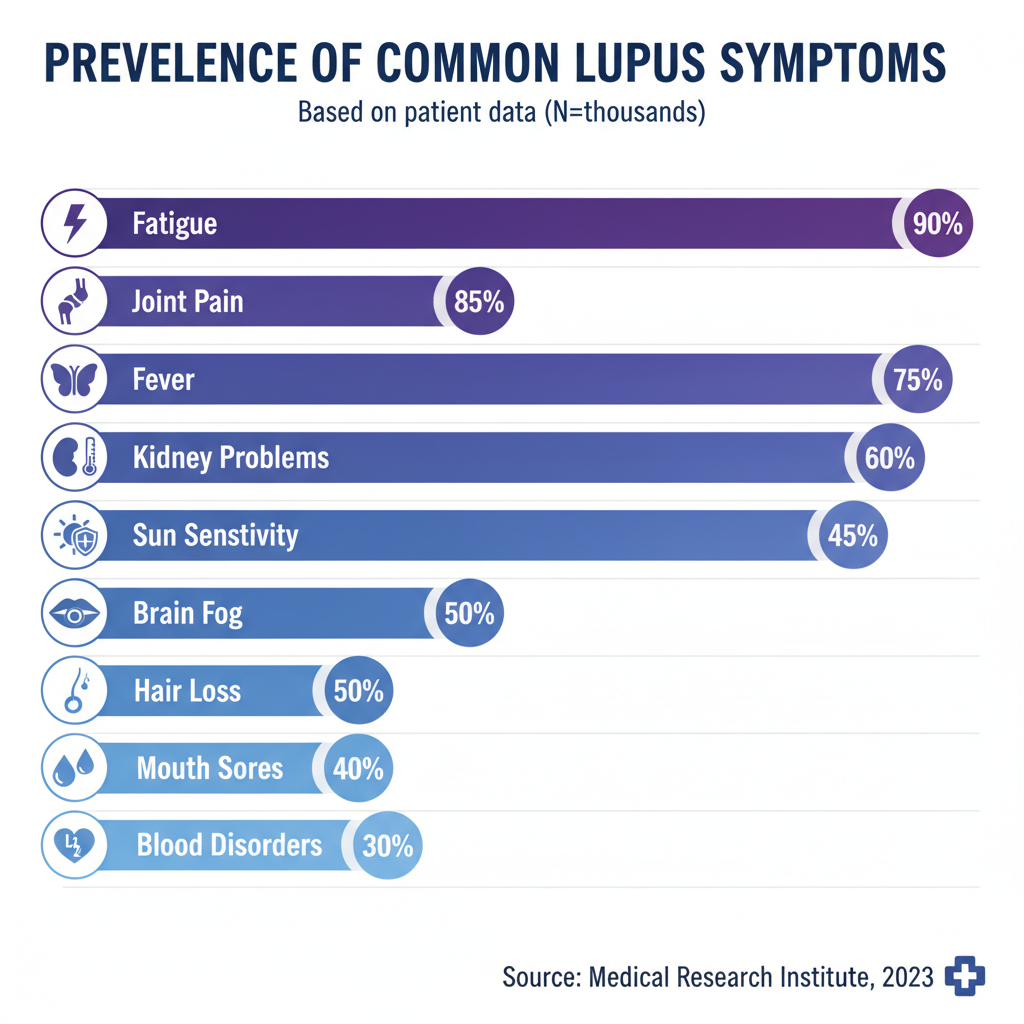
Chart 1: Prevalence of the 11 Common Symptoms of Lupus. This chart clearly shows that joint pain and extreme fatigue are the most widespread symptoms, affecting over 80% of patients. Cutaneous (skin) symptoms are also very common, while Raynaud’s Phenomenon is less frequent but still significant.
What Causes Lupus?
The exact cause of lupus remains unknown. However, researchers believe it’s a combination of genetics, hormones, and environmental factors.
As noted by the Lupus Foundation of America, the disease tends to run in families, suggesting a genetic predisposition.
People born with this tendency may develop lupus after encountering an environmental trigger.
- Genetics: While there is no single “lupus gene”, scientists have identified several genes that may increase a person’s risk.
- Hormones: Lupus is far more common in women than men, particularly during their childbearing years. This has led researchers to believe that female hormones like estrogen may play a role in the disease’s development.
- Environmental Triggers: Certain factors in the environment can trigger the onset of lupus or cause a flare in someone who already has the disease. Common triggers include:
- Sunlight (UV light): As mentioned, this is a major trigger for many.
- Infections: Viruses like Epstein-Barr or cytomegalovirus have been linked to lupus onset.
- Medications: Certain prescription drugs, particularly some blood pressure medications, anti-seizure drugs, and antibiotics, can cause drug-induced lupus.
- Stress: Severe emotional or physical stress can also trigger a flare.
How Is Lupus Diagnosed?
Diagnosing lupus is a complex process that involves several steps, as no single test can confirm the disease.
A rheumatologist, a doctor specializing in diseases of the joints and muscles, typically makes the diagnosis.
- Medical History and Symptom Review: The doctor will ask detailed questions about your symptoms, their duration, and any patterns you’ve noticed. Using a checklist of the 11 symptoms described above is a common practice.
- Physical Examination: The doctor will look for physical signs of lupus, such as skin rashes, mouth sores, and joint swelling or tenderness.
- Laboratory Tests:
- Antinuclear Antibody (ANA) Test: This is a key screening test. A positive ANA test means your immune system is producing autoantibodies, a hallmark of autoimmune disease. While most people with lupus have a positive ANA, a positive test alone doesn’t mean you have lupus, as it can be positive in other conditions or even in healthy individuals.
- Other Antibody Tests: If the ANA is positive, more specific antibody tests (like anti-dsDNA and anti-Smith) are performed, which are more specific to lupus.
- Complete Blood Count (CBC): This can reveal anemia (low red blood cells) or low white blood cell or platelet counts, which are common in lupus.
- Urine and Kidney Function Tests: These are used to check for kidney involvement (lupus nephritis).
- Biopsy: In some cases, a small piece of tissue from the skin (for a rash) or kidney may be removed and examined under a microscope to look for signs of autoimmune damage.
To aid in this process, the Lupus Foundation of America offers a helpful resource. You can use their “Could It Be Lupus?” questionnaire to document your symptoms before your doctor’s appointment.
When to See a Doctor: Recognizing the Patterns
It’s important to consult a healthcare professional if you experience a combination of the symptoms described in this article, especially if they are persistent, recurrent, or unexplained.
While having one symptom, like fatigue or joint pain, is common and can be caused by many things, a pattern of multiple symptoms is more concerning.
You should make an appointment with your doctor if you experience:
- An unexplained rash, particularly a butterfly-shaped rash on your face or a rash that worsens with sun exposure.
- Persistent joint pain and stiffness, especially if it affects multiple joints.
- Overwhelming fatigue that doesn’t improve with rest, combined with other symptoms like fever or joint pain.
- Any combination of two or more of the 11 symptoms listed above that lasts for more than a few weeks.
Come to your appointment prepared. Keeping a symptom diary can be incredibly helpful for your doctor. The table below provides a simple template you can use.
Lupus Symptom Tracker Table
Use this table to track your symptoms over time. Note the date, the symptom you’re experiencing, its severity (on a scale of 1-10), and any potential triggers.
This can provide valuable information for your doctor.
| Date | Symptom | Severity (1-10) | Duration | Potential Triggers (e.g., sun, stress, lack of sleep) |
|---|---|---|---|---|
| Example: 2025-10-20 | Joint pain (wrists, knees) & Fatigue | 7 | All day | Long day in the sun yesterday |
Frequently Asked Questions About Lupus
What are the very first signs of lupus?
There is no single first sign. Early symptoms vary widely but often include extreme fatigue, joint pain, and skin rashes like the butterfly rash. These early signs are generally the same as the common symptoms of the disease and can develop slowly over time.
Can you have lupus without the butterfly rash?
Yes. The classic butterfly (malar) rash is a distinctive sign but occurs in less than 50% of people with lupus. Many patients are diagnosed without ever developing this specific rash, instead presenting with other symptoms like joint pain, fatigue, or kidney problems.
Is lupus contagious?
No, lupus is not contagious. It is an autoimmune disease, meaning it is caused by a malfunction of your own immune system. You cannot “catch” it from someone or give it to someone else through any form of contact.
How is lupus treated?
There is no cure, but treatments focus on managing symptoms, reducing inflammation, and preventing flares. Common medications include anti-inflammatories (NSAIDs), corticosteroids, antimalarials (like hydroxychloroquine), and immunosuppressants. Lifestyle changes like sun protection and stress management are also key.
What are the different types of lupus?
The most common type is Systemic Lupus Erythematosus (SLE), which affects multiple body parts. Other types include Cutaneous Lupus (affects only the skin), Drug-Induced Lupus (caused by certain medications and usually resolves when the drug is stopped), and Neonatal Lupus (a rare condition in newborns).
Does lupus get worse over time?
Lupus is a chronic disease with periods of illness (flares) and wellness (remission). For some, the disease can become more severe over time, potentially leading to organ damage. However, with modern treatments and careful management, many people can control their symptoms and prevent progression.
Can stress trigger a lupus flare?
Yes, both physical and emotional stress are well-known triggers for lupus flares. Managing stress through techniques like mindfulness, exercise, and adequate rest is an important part of living with lupus and can help reduce the frequency and severity of flares.
Who is most at risk for developing lupus?
Lupus can affect anyone, but it is most common in women of childbearing age (15-44). It is also more prevalent and often more severe in women of color, particularly African American, Hispanic, Asian, and Native American women.
Conclusion
Lupus is a complex and multifaceted autoimmune disease, and its ability to mimic other conditions makes it a challenge to identify.
However, by understanding the 11 most common symptoms—from the near-universal joint pain and fatigue to the distinctive butterfly rash and serious kidney complications—you are better equipped to recognize potential warning signs in yourself or a loved one.
Remember that symptoms vary greatly from person to person, and having one or more of these signs does not automatically mean you have lupus. The key is to observe patterns and combinations of symptoms that are persistent and unexplained.
If you are experiencing several of the symptoms discussed in this article, do not ignore them. Schedule an appointment with a healthcare professional to discuss your concerns. Early diagnosis and treatment are the most powerful tools available to manage lupus effectively, prevent long-term damage, and maintain the best possible quality of life.
We encourage you to share this article to help raise awareness. If you have a personal experience with lupus or a question, please consider leaving a comment below to contribute to our community of support and knowledge.

