Fibromyalgia is a chronic disorder characterized by widespread musculoskeletal pain, profound fatigue and sleep disturbances.
This condition affects how your brain and spinal cord process pain signals, amplifying painful sensations.
Affecting an estimated 4 million adults in the U.S. alone, or about 2% of the adult population, fibromyalgia can significantly impact daily life.
However, a diagnosis is not the end of the road, it’s the beginning of a journey toward understanding and managing your symptoms.
This comprehensive guide will walk you through the complexities of fibromyalgia, from its underlying mechanisms and diagnosis to a full spectrum of treatment and management strategies designed to help you regain control and improve your quality of life.
In This Article
What is Fibromyalgia, Really? Beyond the Basic Definition
While often defined by its symptoms, understanding fibromyalgia requires looking deeper into how the central nervous system functions.
It’s not a disease of the muscles, joints, or tissues themselves, but rather a disorder of pain processing.
Think of it as the body’s “volume knob” for pain being turned up too high.
The Science of Central Sensitization
The leading theory behind fibromyalgia is a phenomenon called central sensitization.
In this state, the central nervous system (the brain and spinal cord) becomes hypersensitive to stimuli.
As a result, things that shouldn’t be painful, like a gentle touch, can cause significant pain (a symptom known as allodynia).
Furthermore, things that are mildly painful to others can feel intensely painful (a symptom called hyperalgesia).
According to research published in StatPearls, this altered processing is linked to changes in neurotransmitters—the chemical messengers in the brain.
People with fibromyalgia often have elevated levels of pain-signaling chemicals (like glutamate and substance P) and lower levels of pain-inhibiting chemicals (like serotonin and norepinephrine).
Common Misconceptions: Is Fibromyalgia an Autoimmune Disease?
One of the most common questions is whether fibromyalgia is an autoimmune disease.
The answer is no. In autoimmune diseases like rheumatoid arthritis or lupus, the body’s immune system mistakenly attacks its own healthy tissues, causing inflammation and damage.
While fibromyalgia shares symptoms like pain and fatigue with autoimmune disorders, it does not cause inflammation or tissue damage.
This distinction is crucial for proper diagnosis and treatment.
However, it’s worth noting that having an autoimmune disease can be a risk factor for developing fibromyalgia.
Fibromyalgia by the Numbers: Key Statistics
Understanding the prevalence of fibromyalgia helps contextualize its impact:
- Prevalence: It affects approximately 2-4% of the global population. In the United States, this translates to about 4 million adults, according to the Centers for Disease Control and Prevention (CDC).
- Gender Disparity: Fibromyalgia is diagnosed far more often in women than in men. The National Fibromyalgia Association estimates that 75-90% of people with fibromyalgia are women.
- Age of Onset: While it can affect people of all ages, including children, it most commonly develops during middle age.
What Are the Core Symptoms of Fibromyalgia?
The symptoms of fibromyalgia are complex and can vary widely from person to person and even day to day.
However, a core set of symptoms defines the condition.
The Triad: Widespread Pain, Fatigue and Sleep Issues
The hallmark of fibromyalgia is a combination of three persistent symptoms:
- Widespread Pain: This is the defining symptom. The pain is typically described as a constant dull ache that has lasted for at least three months. To be considered widespread, the pain must occur on both sides of the body and both above and below the waist.
- Fatigue: This isn’t just normal tiredness. People with fibromyalgia often describe an overwhelming, debilitating fatigue that interferes with work, social, and personal activities. It can feel like having the flu all the time.
- Sleep Disturbances: Despite feeling exhausted, many people with fibromyalgia have trouble sleeping. They may wake up frequently during the night and often report waking up feeling unrefreshed, as if they haven’t slept at all.
Cognitive Dysfunction: Understanding ‘Fibro Fog’
Many individuals experience cognitive difficulties, commonly referred to as “fibro fog”.
This is not a formal medical term but is widely used to describe a range of issues, including:
- Difficulty concentrating or paying attention
- Short-term memory problems
- Slowness of thought or mental cloudiness
- Trouble finding the right words
Fibro fog can be just as frustrating and disabling as the physical pain, affecting performance at work and in daily tasks.
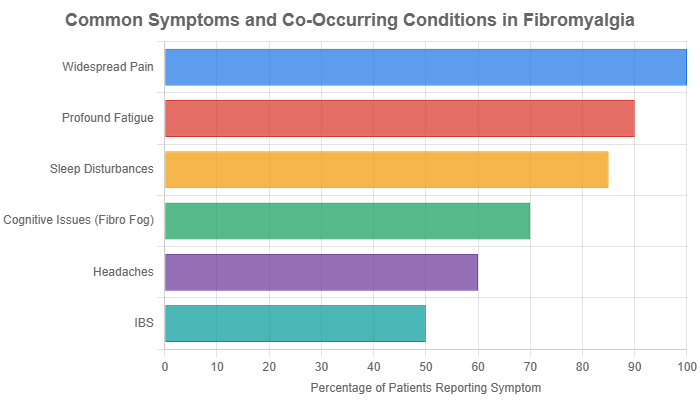
Other Common Symptoms and Co-occurring Conditions
Beyond the core symptoms, fibromyalgia is often associated with a host of other issues.
The Mayo Clinic notes that many people with fibromyalgia also have:
- Headaches, including migraines and tension headaches
- Irritable Bowel Syndrome (IBS)
- Painful bladder syndrome or interstitial cystitis
- Temporomandibular joint (TMJ) disorders
- Anxiety and depression
- Increased sensitivity to temperature, loud noises, and bright lights
How is Fibromyalgia Diagnosed in 2025?
Diagnosing fibromyalgia can be a lengthy process because there is no single lab test or imaging scan to confirm it.
The diagnosis is made clinically, based on patient-reported symptoms and by ruling out other conditions with similar symptoms.
The Evolution from Tender Points to Modern Criteria
For many years, diagnosis relied on the 1990 American College of Rheumatology (ACR) criteria, which involved a “tender point exam”.
A doctor would apply pressure to 18 specific points on the body and a diagnosis required pain in at least 11 of these points.
However, this method was subjective and failed to account for the severity of other key symptoms like fatigue and fibro fog.
A critical review of diagnostic criteria published in the journal Pain Research and Management highlights that the old tender point model was biased and often missed diagnosing men, who tend to have fewer tender points. This led to the development of more comprehensive criteria. Source: PMC
The 2016 ACR Criteria: WPI and SS Scale Explained
Today, doctors use the updated 2016 ACR criteria, which shift the focus from tender points to a more holistic view of the patient’s experience.
This system uses two scores:
- Widespread Pain Index (WPI): Patients indicate where they have felt pain in the last week across 19 different body areas. The score is the total number of painful areas (0-19).
- Symptom Severity (SS) Scale: Patients rate the severity of fatigue, waking unrefreshed, and cognitive symptoms on a scale of 0-3. An additional score (0-3) is given for the number of other general somatic symptoms. The total SS score ranges from 0-12.
A diagnosis of fibromyalgia is made if a person meets a specific combination of WPI and SS scores (e.g., WPI ≥ 7 and SS ≥ 5) and has had symptoms at a similar level for at least three months.
The Role of a Doctor and Ruling Out Other Conditions
A thorough medical history and physical exam are essential.
Your doctor will likely order blood tests to rule out other conditions that can mimic fibromyalgia, such as:
- Hypothyroidism (underactive thyroid)
- Rheumatoid arthritis
- Lupus
- Polymyalgia rheumatica
- Vitamin D deficiency
Once other conditions are excluded, and the symptom criteria are met, a diagnosis of fibromyalgia can be confidently made.
What Are the FDA-Approved Medications for Fibromyalgia Treatment?
While there is no cure for fibromyalgia, several medications are approved by the U.S. Food and Drug Administration (FDA) specifically to manage its symptoms.
The goal of fibromyalgia treatment with medication is to reduce pain and improve function.
Antidepressants: SNRIs (Duloxetine, Milnacipran)
Two of the three FDA-approved drugs are from a class of antidepressants called Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs).
They work by increasing the levels of serotonin and norepinephrine in the brain.
These neurotransmitters help regulate mood, but they are also crucial for modulating the body’s pain signals.
- Duloxetine (Cymbalta): Helps reduce pain and can also treat the anxiety or depression that often accompanies fibromyalgia.
- Milnacipran (Savella): Specifically approved for fibromyalgia pain, it works similarly to duloxetine but is not typically used as a general antidepressant.
Anti-Seizure Medications (Pregabalin)
The third FDA-approved medication was originally developed to treat seizures and nerve pain.
- Pregabalin (Lyrica): This drug is thought to work by calming overactive nerve cells that transmit pain signals. It can be particularly effective for the nerve-like pain (burning, tingling) that some people with fibromyalgia experience.
Off-Label and Other Pharmacological Options
Doctors may also prescribe other medications “off-label”, meaning they are not FDA-approved for fibromyalgia but have shown effectiveness in studies and clinical practice.
- Amitriptyline: An older tricyclic antidepressant that is often prescribed in low doses at bedtime to improve sleep and reduce pain.
- Gabapentin (Neurontin): Similar to pregabalin, it can help with pain and sleep.
- Cyclobenzaprine: A muscle relaxant that can help improve sleep quality when taken at night.
A 2024 review on the management of fibromyalgia emphasized that medication choices should be tailored to the patient’s most dominant symptoms, such as pain, sleep disturbance, or mood issues. Source: Management of Fibromyalgia: An Update – PMC
Which Lifestyle and Management Strategies Are Most Effective?
Medication is only one piece of the puzzle.
The most successful management plans for fibromyalgia are comprehensive and heavily feature non-pharmacological strategies.
These approaches empower you to take an active role in your health.
The Cornerstone of Management: Pacing and Activity Modification
One of the biggest challenges in fibromyalgia is the “push-crash” cycle.
On a good day, you might overdo it, leading to a severe flare-up of symptoms (a “crash”) that lasts for days.
Pacing is the strategy of breaking this cycle. It involves:
- Breaking tasks into smaller, manageable chunks.
- Taking scheduled rest breaks, even if you don’t feel tired.
- Learning to listen to your body and stopping *before* you hit your limit.
- Gradually increasing activity levels over time, rather than all at once.
Sleep Hygiene: Your Foundation for a Better Day
Improving sleep is critical for managing pain and fatigue. Good sleep hygiene practices include:
- Consistent Schedule: Go to bed and wake up at the same time every day, even on weekends.
- Relaxing Routine: Create a calming pre-sleep ritual, such as taking a warm bath, reading a book, or listening to quiet music.
- Optimize Your Environment: Keep your bedroom dark, quiet and cool. Avoid screens (phones, TVs, computers) for at least an hour before bed.
- Avoid Stimulants: Limit caffeine and alcohol, especially in the evening.
Stress Management Techniques (Mindfulness, CBT)
Stress is a major trigger for fibromyalgia flares.
Learning to manage it is essential. Techniques include:
- Cognitive Behavioral Therapy (CBT): A type of talk therapy that helps you identify and change negative thought patterns and behaviors related to pain and stress.
- Mindfulness and Meditation: Practices that train you to focus on the present moment without judgment, which can reduce the brain’s reactivity to pain signals.
- Deep Breathing Exercises: Simple, effective techniques to calm the nervous system.
How Can Exercise and Physical Therapy Help Manage Pain?
While it may seem counterintuitive to exercise when you’re in pain, regular physical activity is one of the most effective treatments for fibromyalgia.
The key is to start slow and choose the right kind of exercise.
Starting Slow: Low-Impact Aerobic Exercise
High-impact exercise can be too jarring.
Instead, focus on gentle, low-impact aerobic activities that get your heart rate up without stressing your joints. Examples include:
- Walking
- Swimming or water aerobics
- Biking on a stationary or recumbent bike
- Using an elliptical machine
The goal is to start with just 5-10 minutes a day and gradually increase the duration and frequency as you build tolerance.
Specialized Therapies: Aquatic Therapy and Tai Chi
Some forms of exercise have been particularly well-studied for fibromyalgia:
- Aquatic Therapy: Exercising in a warm water pool can be incredibly beneficial. The buoyancy of the water supports the body, reducing impact on joints, while the warmth helps relax muscles and ease pain.
- Tai Chi and Qigong: These ancient Chinese practices combine slow, gentle movements with deep breathing and meditation. Research has shown they can improve pain, fatigue, sleep and overall quality of life in people with fibromyalgia.
The Role of a Physical Therapist: Manual Therapy and More
A physical therapist who specializes in chronic pain can be an invaluable partner.
As outlined by the American Physical Therapy Association, they can create a personalized program that includes:
- Pain Education: Helping you understand how pain works in your body.
- Stretching and Strengthening Exercises: To improve flexibility and support your joints.
- Manual Therapy: Hands-on techniques to gently move joints and soft tissues to relieve stiffness and pain.
Does Diet Impact Fibromyalgia Symptoms?
While there is no specific “fibromyalgia diet”, many people find that their food choices can influence their symptoms.
The focus is generally on reducing inflammation and avoiding trigger foods.
Anti-Inflammatory and Antioxidant-Rich Diets
A diet rich in whole foods, similar to the Mediterranean diet, is often recommended. This involves eating:
- A variety of fruits and vegetables
- Lean proteins like fish and poultry
- Healthy fats from olive oil, nuts and avocados
- Whole grains
This eating pattern helps provide antioxidants that combat oxidative stress, which is thought to be elevated in fibromyalgia.
A 2024 review in *Nutrients* highlighted how dietary interventions can positively impact symptoms. Source: Diet and Lifestyle Modifications for Fibromyalgia – PMC
Exploring Low-FODMAP and Gluten-Free Approaches
Since many people with fibromyalgia also have IBS, some find relief with a low-FODMAP diet.
FODMAPs are types of carbohydrates that can be poorly absorbed, leading to gas, bloating and pain.
Similarly, some individuals with fibromyalgia report sensitivity to gluten even if they don’t have celiac disease, and a gluten-free diet may reduce their symptoms.
Key Supplements: Vitamin D, Magnesium and CoQ10
Deficiencies in certain nutrients are common in people with fibromyalgia.
While you should always talk to your doctor before starting supplements, some have shown promise:
- Vitamin D: Low levels are linked to widespread pain.
- Magnesium: Plays a role in muscle and nerve function.
- Coenzyme Q10 (CoQ10): An antioxidant that may help with fatigue.
| Treatment Approach | Primary Target Symptoms | Examples | Evidence Level |
|---|---|---|---|
| Pharmacological | Pain, Mood, Sleep | Pregabalin, Duloxetine, Amitriptyline | Strong |
| Exercise Therapy | Pain, Fatigue, Function, Mood | Aerobics, Aquatic Therapy, Tai Chi | Strong |
| Psychological Therapy | Pain Perception, Mood, Coping | Cognitive Behavioral Therapy (CBT), Mindfulness | Strong |
| Diet & Nutrition | Inflammation, Fatigue, Gut Health | Anti-inflammatory diet, Low-FODMAP | Moderate |
| Complementary | Pain, Stiffness, Relaxation | Acupuncture, Massage, Yoga | Moderate to Limited |
What Are the Promising Alternative and Complementary Therapies?
Many people with fibromyalgia turn to complementary and alternative medicine (CAM) to supplement their conventional treatment plan.
It’s crucial to discuss these options with your doctor to ensure they are safe and appropriate for you.
Acupuncture and Massage Therapy
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body. Some studies suggest it can help relieve pain and improve quality of life for people with fibromyalgia.
- Massage Therapy: Gentle massage can help reduce muscle tension, improve circulation and promote relaxation. Techniques like myofascial release may be particularly helpful for tender points.
Mind-Body Practices: Yoga and Meditation
Yoga combines physical postures, breathing exercises and meditation.
A gentle or restorative yoga practice can improve flexibility, reduce stress and ease pain.
Meditation, especially mindfulness meditation, has strong evidence for helping people change their relationship with chronic pain, reducing its emotional impact.
Emerging Research and Future Directions
The field of fibromyalgia research is active.
Scientists are exploring new drug targets, the role of the gut microbiome, neurostimulation techniques (like tDCS) and the potential genetic underpinnings of the condition.
Participating in clinical trials can be a way for patients to access novel treatments while contributing to scientific progress.
You can find active trials on websites like CenterWatch.
Frequently Asked Questions (FAQ)
What is the main cause of fibromyalgia?
The exact cause is unknown, but it’s believed to involve a combination of genetic predisposition, physical or emotional trauma, infections, and abnormalities in how the central nervous system processes pain. It is a disorder of central sensitization.
Can fibromyalgia go away?
Fibromyalgia is a chronic condition, meaning it is long-lasting and currently has no cure. However, with effective management strategies, many people can significantly reduce their symptoms and lead full, active lives. Symptoms can also fluctuate, with periods of remission.
Is fibromyalgia a disability?
Fibromyalgia can be disabling, and some people with severe symptoms qualify for disability benefits. The determination depends on how significantly the condition limits one’s ability to perform work-related tasks and daily activities.
What is the best pain relief for fibromyalgia?
There is no single “best” pain reliever. The most effective approach is typically a combination of treatments, including low-impact exercise, stress management, improved sleep, and FDA-approved medications like pregabalin or duloxetine, tailored to the individual.
What foods should you avoid with fibromyalgia?
While there’s no universal list, many people find relief by avoiding inflammatory foods like processed items, excessive sugar and unhealthy fats. Some also identify personal trigger foods, such as gluten, dairy or artificial sweeteners like aspartame.
How do you get diagnosed with fibromyalgia?
Diagnosis is made by a doctor based on your symptoms, a physical exam, and ruling out other conditions. It involves using the 2016 ACR criteria, which assess the number of painful areas (WPI) and the severity of other key symptoms (SS Scale).
Does stress make fibromyalgia worse?
Yes, stress is a very common and powerful trigger for fibromyalgia flares. Both physical and emotional stress can cause a significant increase in pain, fatigue, and other symptoms. This is why stress management is a cornerstone of treatment.
Is fibromyalgia genetic?
There appears to be a genetic component. Fibromyalgia tends to run in families, and having a close relative with the condition increases your risk. Researchers are studying specific genes that may be involved in pain processing and susceptibility.
Conclusion
Living with fibromyalgia is a marathon, not a sprint. It requires patience, self-compassion, and a proactive approach to management.
While the journey can be challenging, remember that you are not alone and that effective tools are available.
The most powerful strategy is a multi-faceted one that combines medical treatment with lifestyle adjustments, exercise and mental health support.
By understanding your condition, working closely with your healthcare team and advocating for your needs, you can navigate the complexities of fibromyalgia and build a life that is not defined by pain.
Take the first step today by discussing these strategies with your doctor and exploring the resources that feel right for you.

