Irritable Bowel Syndrome (IBS) is a common and often frustrating gastrointestinal disorder characterized by abdominal pain, bloating, gas, and changes in bowel habits. Affecting an estimated 25 to 45 million people in the United States, it can significantly impact daily life, yet it remains widely misunderstood.
Unlike inflammatory bowel disease (IBD), IBS does not cause visible damage to the digestive tract, making it a “functional” disorder—the problem lies in how the gut works, not its structure.
This guide provides a comprehensive, evidence-based overview of Irritable Bowel Syndrome, moving beyond the basics to offer actionable strategies for management. We will explore the different types of IBS, delve into the latest research on its causes, and break down the most effective dietary, medical, and lifestyle interventions.
By the end of this article, you will have a clear roadmap to better understand and manage your IBS symptoms.
In This Article
What is Irritable Bowel Syndrome (IBS)?
Irritable Bowel Syndrome is a chronic condition affecting the large intestine. It’s defined by a group of symptoms that occur together, primarily abdominal pain linked to bowel movements.
The key feature of IBS is that these symptoms exist without any signs of physical damage or disease in the gut, which can be confirmed through diagnostic tests like a colonoscopy.
A Functional Disorder, Not a Disease
The term functional gastrointestinal disorder is crucial to understanding IBS. It means that while the digestive system looks perfectly normal on examination, it doesn’t function correctly.
The communication between the brain, nervous system, and the gut is disrupted, leading to the uncomfortable symptoms that define the condition.
This is why it’s often referred to as a disorder of the “brain-gut interaction”.
The Brain-Gut Axis: A Two-Way Street
The brain and the gut are in constant communication through a network of nerves, hormones, and chemicals. This connection, known as the brain-gut axis, is vital for healthy digestion.
In people with IBS, this communication system is hypersensitive and poorly regulated.
Stress or anxiety can trigger gut symptoms, and conversely, gut problems can lead to increased stress and anxiety.
This creates a vicious cycle that can make managing Irritable Bowel Syndrome challenging.
Understanding this connection is the first step toward effective, holistic treatment.
What Are the Main Symptoms of Irritable Bowel Syndrome?
The symptoms of Irritable Bowel Syndrome can vary widely from person to person and can even change over time for the same individual.
However, a core set of symptoms is common to most diagnoses.
Core Symptoms: Pain, Bloating, and Gas
The hallmark symptom of IBS is recurrent abdominal pain or cramping. This pain is typically related to bowel movements—it may improve after a bowel movement or worsen beforehand.
The location and intensity of the pain can vary.
Bloating and gas are also extremely common. Many people with IBS report feeling uncomfortably full or swollen, especially as the day progresses.
This can be due to increased gas production or, more often, impaired transit of gas through the intestines.
Changes in Bowel Habits
Beyond pain, the most defining feature of IBS is a change in bowel habits. This can manifest as:
- Diarrhea: Frequent, loose, watery stools, often with a sense of urgency.
- Constipation: Infrequent stools that are hard, lumpy, and difficult to pass, often accompanied by a feeling of incomplete evacuation.
- Alternating Diarrhea and Constipation: Periods of constipation followed by episodes of diarrhea.
- Mucus in the stool: Some individuals may notice a whitish mucus in their bowel movements.
How is Irritable Bowel Syndrome Diagnosed?
There is no single test to definitively diagnose Irritable Bowel Syndrome. Instead, diagnosis is based on a careful review of your symptoms, medical history, and a physical exam.
Doctors use specific criteria to identify a pattern consistent with IBS while ruling out other, more serious conditions.
The Rome IV Criteria Explained
Gastroenterologists often use the Rome IV criteria to diagnose IBS. According to these guidelines, a diagnosis of IBS requires recurrent abdominal pain, on average, at least one day per week in the last three months, associated with two or more of the following:
- Pain is related to defecation (either improves or worsens).
- Associated with a change in stool frequency.
- Associated with a change in stool form (appearance).
These criteria must be fulfilled for the last three months with symptom onset at least six months before diagnosis. This helps distinguish IBS from temporary digestive upset.
Ruling Out Other Conditions (Red Flag Symptoms)
Because IBS symptoms can overlap with other conditions like celiac disease, inflammatory bowel disease (Crohn’s or ulcerative colitis), or even colon cancer, a doctor may order tests to rule them out. This is especially important if you have “red flag” symptoms, which include:
- Unexplained weight loss
- Rectal bleeding or blood in the stool
- Fever
- Nighttime diarrhea that awakens you from sleep
- Iron deficiency anemia
- A family history of IBD or colorectal cancer
If these are present, your doctor will likely recommend further testing, such as blood tests, stool tests, or a colonoscopy.
What Are the Different Types of IBS?
IBS is not a one-size-fits-all condition. It is categorized into subtypes based on the predominant bowel habit.
This classification helps guide treatment, as therapies that work for one type may not be effective for another.
The type is determined by the consistency of your stools on days with abnormal bowel movements, often using the Bristol Stool Form Scale.
| IBS Subtype | Description | Common Stool Characteristics (Bristol Scale) | Primary Challenge |
|---|---|---|---|
| IBS with Constipation (IBS-C) | On days with at least one abnormal bowel movement, more than 25% of stools are hard or lumpy, and less than 25% are loose or watery. | Type 1 (separate hard lumps) and Type 2 (lumpy, sausage-shaped). | Infrequent, painful bowel movements; straining; feeling of incomplete evacuation. |
| IBS with Diarrhea (IBS-D) | On days with at least one abnormal bowel movement, more than 25% of stools are loose or watery, and less than 25% are hard or lumpy. | Type 6 (fluffy pieces) and Type 7 (watery, no solid pieces). | Urgency; frequent bowel movements; fear of accidents in public. |
| IBS with Mixed Bowel Habits (IBS-M) | On days with at least one abnormal bowel movement, more than 25% of stools are hard or lumpy, and more than 25% are loose or watery. | Alternating between Type 1/2 and Type 6/7. | Unpredictability; switching between constipation and diarrhea, sometimes within the same day. |
| IBS Unsubtyped (IBS-U) | Patients meet the diagnostic criteria for IBS but their bowel habits do not fit into the C, D, or M categories. | Variable, does not meet criteria for other subtypes. | Inconsistent symptoms that are difficult to categorize and treat. |
What Causes Irritable Bowel Syndrome?
The exact cause of Irritable Bowel Syndrome is unknown, but it is believed to be multifactorial, involving a combination of genetic and environmental factors.
Research has identified several key mechanisms that likely contribute to the development of IBS symptoms.
Gut Motility Issues
Motility refers to the muscular contractions that move food through the digestive tract. In IBS, these contractions can be abnormal.
In IBS-D, contractions may be too fast and strong, leading to diarrhea. In IBS-C, they may be too slow and weak, causing constipation.
Visceral Hypersensitivity
This is a key concept in IBS. It means that the nerves in the gut are overly sensitive.
People with IBS may experience pain and bloating from normal amounts of gas or stool that would not bother someone without the condition.
This heightened pain perception is a central feature of the disorder.
Gut Microbiome Imbalance
The gut is home to trillions of bacteria, fungi, and viruses, collectively known as the gut microbiome.
Research indicates that the composition of this microbiome in people with IBS may differ from that of healthy individuals.
This imbalance, or dysbiosis, can affect digestion, gas production, and immune function in the gut.
Post-Infectious IBS (PI-IBS)
A significant number of IBS cases begin after a severe bout of gastroenteritis (a stomach bug) caused by bacteria or a virus.
This is known as Post-Infectious IBS (PI-IBS). The infection may trigger long-term changes in the gut lining, immune system, and nerve function, leading to persistent IBS symptoms.
The Role of Stress and Early Life Events
While stress doesn’t cause IBS, it is a major trigger for symptom flare-ups.
The brain-gut axis ensures that psychological stress directly impacts gut function.
Furthermore, individuals who have experienced significant stress or trauma, especially in early life, have a higher risk of developing IBS.
How Can Diet and Nutrition Help Manage IBS Symptoms?
For many people with Irritable Bowel Syndrome, dietary changes are the cornerstone of symptom management.
Identifying and avoiding trigger foods can provide significant relief. The most evidence-based dietary approach for IBS is the low-FODMAP diet.
The Low-FODMAP Diet: A Deep Dive
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols.
These are types of short-chain carbohydrates that are poorly absorbed in the small intestine.
When they reach the large intestine, they are rapidly fermented by gut bacteria, producing gas.
They also draw water into the bowel, which can cause bloating, pain, and diarrhea.
The low-FODMAP diet involves three phases:
- Elimination: A strict 2-6 week period where all high-FODMAP foods are removed from the diet.
- Reintroduction: Systematically reintroducing FODMAP groups one by one to identify personal triggers and tolerance levels.
- Personalization: Creating a long-term, modified diet that avoids only the specific FODMAPs that trigger symptoms.
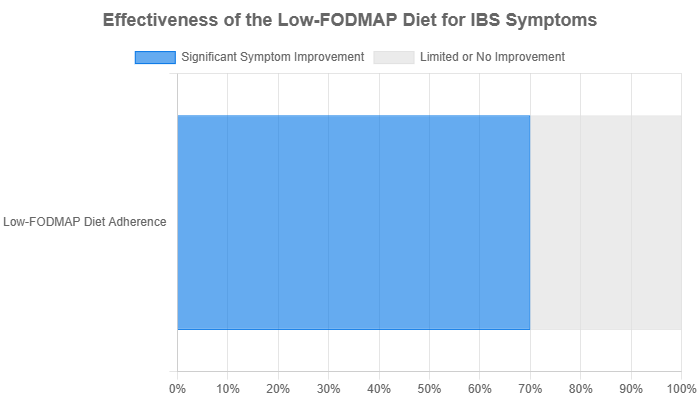
Studies have shown this diet to be highly effective. A systematic review published in the journal Nutrients found that up to 70% of IBS patients experience significant symptom relief while following a low-FODMAP diet under professional guidance.
Other Dietary Strategies
- Fiber Management: For IBS-C, slowly increasing soluble fiber (like psyllium, oats, and citrus) can help soften stool. For IBS-D, insoluble fiber (like wheat bran and whole grains) can sometimes worsen symptoms.
- Avoiding Gluten: Some people with IBS, even without celiac disease, find their symptoms improve on a gluten-free diet. This may be due to a non-celiac gluten sensitivity or because many gluten-containing grains are also high in FODMAPs.
- Identifying Common Triggers: Keeping a food and symptom diary can help identify other common triggers like caffeine, alcohol, spicy foods, and high-fat meals.
What Are the Medical Treatment Options for IBS?
When diet and lifestyle changes aren’t enough, medication can play an important role in managing moderate to severe Irritable Bowel Syndrome symptoms.
Treatments are typically targeted to the patient’s specific subtype and most bothersome symptoms.
Medications for IBS-C
- Fiber Supplements: Psyllium (Metamucil) is often a first-line recommendation.
- Osmotic Laxatives: Polyethylene glycol (Miralax) draws water into the colon to soften stool.
- Prescription Medications: Drugs like Lubiprostone (Amitiza), Linaclotide (Linzess), and Plecanatide (Trulance) work by increasing fluid in the intestines and speeding up transit.
Medications for IBS-D
- Anti-diarrheals: Loperamide (Imodium) can help control diarrhea but doesn’t address pain or bloating.
- Bile Acid Sequestrants: Cholestyramine can help in cases where bile acid malabsorption contributes to diarrhea.
- Prescription Medications: Rifaximin (Xifaxan), an antibiotic, can help by altering gut bacteria. Eluxadoline (Viberzi) and Alosetron (Lotronex, for women only) work on gut receptors to slow contractions and reduce pain.
Medications for Abdominal Pain and Bloating
- Antispasmodics: Medications like Dicyclomine (Bentyl) can help reduce muscle spasms in the colon, easing pain.
- Low-Dose Antidepressants: Tricyclic antidepressants (TCAs) like amitriptyline and selective serotonin reuptake inhibitors (SSRIs) can help manage pain by acting on the nerve signals between the brain and gut. A 2024 study in The Lancet confirmed that low-dose amitriptyline is an effective treatment for IBS.
Are There Effective Lifestyle and Alternative Therapies?
A holistic approach that combines medical treatment with lifestyle changes often yields the best results for managing Irritable Bowel Syndrome.
These therapies focus on the brain-gut axis and overall well-being.
The Power of Probiotics: Choosing the Right Strain
Probiotics are live microorganisms that can provide health benefits by improving gut bacteria balance.
Their effectiveness in IBS can be strain-specific. Some research suggests that certain strains, particularly those containing Bifidobacterium (like B. infantis) and some combinations, may help reduce bloating and overall symptoms.
It’s often recommended to try a specific probiotic for at least four weeks to assess its effect.
Stress Management Techniques
Given the strong link between stress and IBS flare-ups, managing stress is critical. Effective techniques include:
- Cognitive Behavioral Therapy (CBT): A type of psychotherapy that helps change negative thought patterns and behaviors related to symptoms.
- Gut-Directed Hypnotherapy: Involves hypnosis focused on calming the gut and reducing hypersensitivity.
- Mindfulness and Meditation: Practices that can lower stress and improve pain perception.
- Yoga and Tai Chi: Gentle mind-body exercises that combine movement, breathing, and meditation.
The Importance of Exercise
Regular physical activity is beneficial for everyone, but it can be particularly helpful for IBS.
Low-to-moderate intensity exercise, like walking, swimming, or cycling, can help regulate bowel movements (especially for IBS-C), reduce stress, and alleviate bloating and gas.
Living with IBS: Practical Tips and Patient Experiences
Managing a chronic condition like Irritable Bowel Syndrome goes beyond diet and medication.
It involves developing practical strategies to navigate daily life and building a strong support network.
Creating a Symptom Diary
Keeping a detailed diary of your food intake, stress levels, activities, and symptoms is one of the most powerful tools for managing IBS.
Over time, patterns will emerge that can help you and your doctor identify your specific triggers and tailor your management plan more effectively.
Navigating Social Situations
Eating out and social events can be a source of anxiety. Patient communities, like those on Reddit, often share helpful tips:
- Plan Ahead: Look at menus online before you go to a restaurant.
- Communicate: Don’t be afraid to ask for simple modifications to your meal.
- Eat a Small, Safe Meal Beforehand: This can reduce the pressure to eat something that might trigger symptoms.
- Focus on the Company: Remember that social events are about more than just food.
Building a Support System
Living with IBS can feel isolating. Connecting with others who understand can make a huge difference.
This can include talking to trusted friends and family, joining a support group, or participating in online forums.
A good relationship with a knowledgeable and empathetic healthcare provider is also essential.
Frequently Asked Questions (FAQ) about Irritable Bowel Syndrome
1. Can IBS turn into cancer?
No. Irritable Bowel Syndrome does not cause inflammation or changes in bowel tissue and does not increase your risk of colorectal cancer. However, symptoms can overlap, so it’s vital to get a proper diagnosis.
2. Is IBS a lifelong condition?
For most people, IBS is a chronic condition that requires long-term management. However, symptoms can fluctuate and may improve or even disappear for periods of time. Effective management can significantly reduce its impact on your life.
3. Can children get IBS?
Yes, IBS can affect children and adolescents. The symptoms are similar to those in adults, primarily recurrent abdominal pain and altered bowel habits. Diagnosis and management should always be overseen by a pediatrician or pediatric gastroenterologist.
4. Does stress cause IBS?
Stress does not cause IBS, but it is a major trigger that can worsen or provoke symptoms. The strong connection between the brain and the gut means that psychological distress can directly impact gut function and sensitivity.
5. What is the difference between IBS and IBD?
IBS is a functional disorder with no visible damage to the gut. IBD (Inflammatory Bowel Disease), which includes Crohn’s disease and ulcerative colitis, is an autoimmune disease characterized by chronic inflammation and physical damage to the digestive tract.
6. Should I take a probiotic for my IBS?
Probiotics may help some individuals, but their effectiveness varies. Research suggests certain strains of Bifidobacterium and Lactobacillus may be beneficial. It’s best to consult your doctor and try one for at least a month to see if it helps.
7. Can I drink coffee with IBS?
Caffeine can stimulate the colon, which may worsen diarrhea and cramping in some people with IBS, particularly IBS-D. It’s a common trigger, so it’s worth eliminating it temporarily to see if your symptoms improve.
8. Is there a cure for Irritable Bowel Syndrome?
Currently, there is no cure for IBS. However, a combination of dietary changes, lifestyle adjustments, stress management, and targeted medications can effectively manage symptoms and allow individuals to lead full, active lives.
Conclusion
Managing Irritable Bowel Syndrome is a journey of self-discovery and partnership with your healthcare team.
While the path can be challenging, significant progress has been made in understanding and treating this complex condition.
From evidence-based dietary strategies like the low-FODMAP diet to targeted medications and powerful mind-body therapies, there are more tools available than ever before.
The key is a personalized, multi-faceted approach. By tracking your symptoms, identifying your unique triggers, and working with a doctor to build a comprehensive management plan, you can take control of your digestive health and dramatically improve your quality of life.
If you are experiencing symptoms of Irritable Bowel Syndrome, the most important step is to speak with a healthcare professional for an accurate diagnosis.
Don’t hesitate to seek help and start your journey toward feeling better today.

