Insulin is a crucial hormone produced by your pancreas that acts like a key, allowing glucose (sugar) from the food you eat to enter your body’s cells to be used for energy.
Without enough effective insulin, glucose builds up in your bloodstream, leading to serious health complications.
This fundamental process is vital for life, yet an astonishing 97.6 million American adults—more than 1 in 3—have prediabetes, a condition where this system begins to fail.
Understanding how insulin works is the first step toward protecting your metabolic health.
This comprehensive guide will demystify the world of insulin. We will explore its creation within the body, its precise mechanism of action, and what happens when the system goes awry, leading to conditions like insulin resistance and diabetes.
You will learn about the different types of therapeutic insulin, how they are diagnosed and administered, and, most importantly, the powerful, evidence-based steps you can take to prevent or even reverse insulin-related problems.
Read on to become empowered with the knowledge to manage your health effectively.
In This Article
What is Insulin and Why is It Essential?
At its core, insulin is a master metabolic hormone. Think of it as the body’s primary traffic controller for energy.
Its main job is to manage the levels of glucose in your bloodstream, ensuring that all your cells get the fuel they need to function while preventing the damaging effects of high blood sugar.
This hormone is so critical that without it, our bodies cannot properly use or store the energy we get from food, leading to a state of internal starvation even when we eat.
The Pancreas: The Body’s Insulin Factory
The journey of insulin begins deep within the abdomen in an organ called the pancreas.
Nestled behind the stomach, the pancreas has several functions, but for our purposes, its most important role is as an endocrine gland.
Within the pancreas are clusters of specialized cells known as the Islets of Langerhans. These islets are a mix of different cell types, each with a specific job:
- Beta cells: These are the stars of the show. They produce, store, and release insulin.
- Alpha cells: These cells produce glucagon, a hormone that has the opposite effect of insulin—it raises blood glucose levels when they get too low.
- Delta cells: These produce somatostatin, a hormone that helps regulate the activity of both beta and alpha cells.
With every meal, as your body digests carbohydrates and breaks them down into glucose, your blood glucose levels rise.
This signals the beta cells in your pancreas to release a precise amount of insulin into the bloodstream to manage this incoming fuel.
From Proinsulin to Insulin: A Molecular Journey
Inside the beta cells, insulin isn’t created in its final form. It starts as a larger, single-chain molecule called proinsulin.
This precursor molecule is then processed and cleaved (split) into two separate pieces:
- Insulin: The active hormone, ready to do its job.
- C-peptide: A connecting fragment that is released into the bloodstream in equal amounts to insulin.
While C-peptide doesn’t have a known hormonal function, it serves as an invaluable diagnostic tool.
Because it’s released alongside insulin, doctors can measure C-peptide levels in the blood to determine how much insulin a person’s pancreas is naturally producing.
This is especially useful in distinguishing between type 1 and type 2 diabetes and guiding treatment decisions.
The Key-Lock Mechanism: How Insulin Unlocks Cells
Once released, insulin travels through the bloodstream to nearly every cell in the body, including muscle, fat, and liver cells.
On the surface of these cells are insulin receptors. The interaction between insulin and its receptor is often described using a “key and lock” analogy:
- The Key: Insulin is the key.
- The Lock: The insulin receptor on the cell surface is the lock.
When the insulin “key” binds to the receptor “lock”, it triggers a cascade of signals inside the cell.
This signaling pathway instructs the cell to activate special glucose transporters (like GLUT4) which then move to the cell’s surface.
These transporters act like gates, opening up to allow glucose to move from the bloodstream into the cell, where it can be used immediately for energy or stored for later use.
This process efficiently lowers blood glucose levels back to a normal range.
How Does Insulin Work to Regulate Blood Sugar?
The body’s ability to maintain a stable blood glucose level, a state known as glucose homeostasis, is a delicate balancing act orchestrated primarily by insulin and its counter-regulatory hormone, glucagon.
This system works continuously, adapting to your body’s changing needs, whether you’ve just eaten a large meal or have been fasting overnight.
After a Meal: The Role of Insulin in Glucose Storage
When you eat a meal containing carbohydrates, your digestive system breaks them down into glucose, which is then absorbed into your bloodstream.
This causes a rise in blood glucose levels, which is the primary signal for the pancreas to release insulin.
The released insulin then performs several critical tasks:
- Promotes Glucose Uptake: As described earlier, insulin enables muscle and fat cells to take up glucose from the blood for immediate energy needs.
- Stimulates Glycogen Synthesis: Your liver and muscles can store excess glucose for later use. Insulin signals the liver to convert glucose into a storage form called glycogen. This process, known as glycogenesis, is like stocking up the pantry for when energy is needed later.
- Inhibits Glucose Production: To prevent blood sugar from rising too high, insulin also tells the liver to stop producing and releasing its own glucose (a process called gluconeogenesis).
- Promotes Fat Storage: If glycogen stores are full, insulin signals fat cells (adipocytes) to take up excess glucose and convert it into fatty acids, which are then stored as triglycerides. This is the body’s long-term energy reserve.
Between Meals: What Happens When Insulin Levels Fall?
As time passes after a meal, your cells use up the available glucose, and blood sugar levels begin to fall.
This drop in glucose signals the pancreas to decrease its insulin secretion.
As insulin levels decline, the balance of power shifts to the hormone glucagon, which is released by the alpha cells.
Glucagon’s job is to raise blood sugar levels by:
- Stimulating Glycogenolysis: Glucagon signals the liver to break down its stored glycogen back into glucose and release it into the bloodstream.
- Promoting Gluconeogenesis: Glucagon also encourages the liver to create new glucose from other sources, such as amino acids.
This elegant push-and-pull system between insulin and glucagon ensures that your brain and other vital organs have a constant supply of glucose, even when you are not eating.
The Difference in People with Type 1 vs. Type 2 Diabetes
Diabetes occurs when this finely tuned system breaks down. The two main types of diabetes involve different problems with insulin:
- Type 1 Diabetes: In this autoimmune condition, the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the pancreas produces little to no insulin. People with type 1 diabetes must take insulin via injections or a pump to survive, as their bodies have no way to get glucose into their cells.
- Type 2 Diabetes: This is the more common form. It begins with insulin resistance, where the body’s cells (in muscle, fat, and liver) don’t respond properly to insulin. Initially, the pancreas compensates by producing even more insulin to overcome this resistance. Over time, however, the beta cells can become exhausted and may eventually fail to produce enough insulin to keep blood glucose levels in a normal range.
As the American Diabetes Association explains, “People with type 2 diabetes make insulin, but their bodies don’t respond well to it. Some people with type 2 diabetes need diabetes pills or insulin shots to help their bodies use glucose for energy”.
What Happens When Your Body Doesn’t Respond to Insulin?
Imagine your cell’s “locks” becoming rusty and difficult to open. Even though you have plenty of insulin “keys”, they struggle to work effectively.
This is the essence of insulin resistance, a silent but dangerous condition that lays the groundwork for prediabetes and type 2 diabetes.
Defining Insulin Resistance and Prediabetes
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), insulin resistance is a condition in which cells in your muscles, fat, and liver don’t respond well to insulin.
As a result, your pancreas goes into overdrive, pumping out higher and higher amounts of insulin to force the resistant cells to take up glucose.
For a while, this compensation works, and blood glucose levels may remain in the normal range.
However, if this resistance continues or worsens, the pancreas may eventually be unable to keep up.
When that happens, blood glucose levels start to rise above normal, but not yet high enough to be classified as type 2 diabetes. This intermediate stage is known as prediabetes.
Who is at Risk for Developing Insulin Resistance?
While researchers don’t fully understand all the causes, certain factors significantly increase your chances of developing insulin resistance and prediabetes.
Some you can’t change, but many are within your control. Key risk factors include:
- Having overweight or obesity, especially with excess abdominal fat.
- Being age 35 or older, as risk increases with age.
- A family history of diabetes.
- Certain racial and ethnic groups, including African American, American Indian, Asian American, and Hispanic/Latino individuals.
- A sedentary lifestyle with little physical activity.
- A history of gestational diabetes during pregnancy or giving birth to a baby over 9 pounds.
- Having other health conditions like polycystic ovary syndrome (PCOS), high blood pressure, or unhealthy cholesterol levels.
- Smoking or exposure to secondhand smoke.
You may prevent insulin resistance and prediabetes by reaching and maintaining a healthy weight and being physically active. Image courtesy of NIDDK.
The Health Consequences of Untreated Insulin Resistance
Insulin resistance and prediabetes are not benign conditions. They are serious warning signs that your metabolic health is under strain.
If left unaddressed, they can lead to a host of health problems, including:
- Type 2 Diabetes: This is the most direct and well-known consequence.
- Heart Disease and Stroke: Insulin resistance is linked to high blood pressure, unhealthy cholesterol and triglyceride levels, and inflammation, all of which are major risk factors for cardiovascular disease.
- Metabolic Syndrome: A cluster of conditions (including a large waist size, high blood pressure, high blood sugar, and abnormal cholesterol/triglyceride levels) that dramatically increases your risk for heart disease, stroke, and diabetes.
- Nonalcoholic Fatty Liver Disease (NAFLD): A buildup of fat in the liver that can lead to inflammation and liver damage.
The good news is that prediabetes is often reversible. By making lifestyle changes, you can improve your body’s sensitivity to insulin and significantly lower your risk of progressing to type 2 diabetes.
What Are the Different Types of Insulin?
For individuals whose bodies do not produce enough insulin (type 1 diabetes) or cannot use it effectively (advanced type 2 diabetes), insulin therapy is a life-saving treatment.
Modern medicine offers a variety of insulin types, each designed with a different action profile to mimic the body’s natural insulin release as closely as possible.
Understanding Insulin Characteristics: Onset, Peak, and Duration
All types of therapeutic insulin are characterized by three key properties, as outlined by the American Diabetes Association:
- Onset: The length of time it takes for the insulin to reach the bloodstream and begin lowering blood glucose.
- Peak: The time at which the insulin is at its maximum strength and has its greatest effect on lowering blood glucose.
- Duration: The total length of time the insulin continues to work in the body.
Matching the right type of insulin to a person’s needs, meal schedule, and activity level is crucial for effective diabetes management.
Comparative Table of Insulin Types
To help understand the differences, here is a table summarizing the main categories of injectable insulin:
| Insulin Type | Onset | Peak | Duration | Common Examples |
|---|---|---|---|---|
| Rapid-Acting | ~15 minutes | 1-2 hours | 2-4 hours | lispro (Humalog, Admelog), aspart (NovoLog, Fiasp), glulisine (Apidra) |
| Short-Acting (Regular) | ~30 minutes | 2-3 hours | 3-6 hours | Human Regular (Humulin R, Novolin R) |
| Intermediate-Acting | 2-4 hours | 4-12 hours | 12-18 hours | NPH (Humulin N, Novolin N) |
| Long-Acting | Several hours | Minimal or no peak | Up to 24 hours | detemir (Levemir), glargine (Lantus, Basaglar) |
| Ultra Long-Acting | ~6 hours | No peak | 36 hours or longer | degludec (Tresiba), glargine U-300 (Toujeo) |
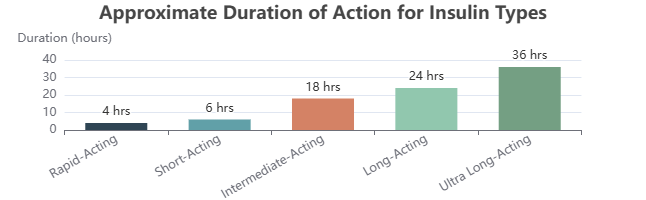
A visual comparison of the approximate duration of action for different insulin types.
A Closer Look at Each Type
- Rapid- and Short-Acting Insulin: Often called “mealtime” or “bolus” insulin, these are taken just before or with meals to cover the rise in blood sugar from food. Their fast action mimics the natural burst of insulin released by a healthy pancreas in response to eating.
- Intermediate-Acting Insulin: This type has a slower onset and a longer duration. It is often used to cover insulin needs for about half a day or overnight. Its pronounced peak, however, can increase the risk of hypoglycemia (low blood sugar) if not timed carefully with meals.
- Long- and Ultra Long-Acting Insulin: Known as “basal” or “background” insulin, these types are designed to provide a steady, continuous release of insulin over a 24-hour period or longer. They have little to no peak, which helps maintain stable blood sugar levels between meals and overnight, mimicking the pancreas’s constant low-level insulin secretion.
Special Formulations: Premixed and Inhaled Insulin
To simplify treatment regimens, some special formulations are available:
- Premixed Insulin: These products combine a rapid- or short-acting insulin with an intermediate-acting insulin in a single vial or pen. They offer convenience but less flexibility in adjusting doses.
- Inhaled Insulin (Afrezza): Approved in 2015, Afrezza is a rapid-acting inhaled insulin powder administered at the beginning of a meal. It begins working within 15 minutes and is out of the system in about 3 hours. It must be used in combination with an injectable long-acting insulin for people with type 1 diabetes.
How Are Prediabetes and Insulin Resistance Diagnosed?
One of the most challenging aspects of insulin resistance and prediabetes is that they usually have no symptoms.
A person can have one or both conditions for years without knowing it.
Therefore, diagnosis relies on proactive screening and specific blood tests, especially for individuals with known risk factors.
Why Insulin Resistance Itself Isn’t Routinely Tested
While there are complex tests to directly measure insulin resistance (like the euglycemic clamp), they are invasive, expensive, and primarily used in research settings.
For clinical purposes, health care professionals diagnose the consequences of insulin resistance—namely, high blood sugar—to identify prediabetes.

Health care professionals use blood tests to find out if you have prediabetes.
Key Blood Tests for Diagnosing Prediabetes
Your doctor can use one of three simple blood tests to determine if you have prediabetes.
The diagnostic criteria are based on guidelines from the American Diabetes Association:
- A1C Test (Hemoglobin A1c): This test measures your average blood glucose level over the past 2 to 3 months. It doesn’t require fasting.
- Normal: Below 5.7%
- Prediabetes: 5.7% to 6.4%
- Diabetes: 6.5% or higher
- Fasting Plasma Glucose (FPG) Test: This test measures your blood glucose after you have not eaten for at least 8 hours (usually overnight).
- Normal: 99 mg/dL or lower
- Prediabetes: 100 to 125 mg/dL
- Diabetes: 126 mg/dL or higher
- Oral Glucose Tolerance Test (OGTT): This test measures your blood glucose before and 2 hours after you drink a special sweet drink. It shows how your body processes glucose.
- Normal: 139 mg/dL or lower
- Prediabetes: 140 to 199 mg/dL
- Diabetes: 200 mg/dL or higher
Screening Recommendations: Who Should Get Tested and When?
The NIDDK recommends testing for prediabetes if you are age 35 or older. If you are younger than 35, you should be tested if you have overweight or obesity and one or more other risk factors for diabetes.
If your results are normal, testing should be repeated at least every 3 years. If you are diagnosed with prediabetes, you should be tested for type 2 diabetes every 1 to 2 years.
Can You Reverse Insulin Resistance and Prevent Type 2 Diabetes?
Absolutely. For many people, a diagnosis of prediabetes is a critical wake-up call and an opportunity to make powerful changes.
Landmark research has shown that you can significantly improve your body’s sensitivity to insulin, reverse prediabetes, and prevent or delay the onset of type 2 diabetes through dedicated lifestyle modifications.
The Power of Lifestyle Changes: Diet and Physical Activity
The cornerstone of reversing insulin resistance is a healthy lifestyle.
This isn’t about extreme diets or impossible workout regimens, it’s about making sustainable changes. A healthy lifestyle includes:
- Consuming healthy foods and drinks: Focus on whole, unprocessed foods like fruits, vegetables, lean proteins, and whole grains. Limit sugary drinks, refined carbohydrates, and processed foods.
- Being physically active: Aim for at least 150 minutes of moderate-intensity activity, like brisk walking, per week.
- Managing your weight: Even modest weight loss can have a profound impact.
- Getting enough sleep: Poor sleep can worsen insulin resistance.
- Quitting smoking: Smoking is a significant risk factor.
The 5-7% Rule: How Modest Weight Loss Makes a Huge Difference
One of the most influential studies in this area is the Diabetes Prevention Program (DPP), funded by the NIH.
This major study found that people at high risk for diabetes who lost just 5% to 7% of their body weight (that’s 10 to 14 pounds for a 200-pound person) and exercised 150 minutes per week reduced their risk of developing type 2 diabetes by an incredible 58%.
The DPP study provided definitive proof that lifestyle intervention is often more effective than medication in preventing type 2 diabetes. Its findings have changed the way diabetes prevention is approached worldwide.
Medications That Can Help: The Role of Metformin
In addition to lifestyle changes, your doctor may prescribe medication.
The most common drug for prediabetes is metformin. The DPP study also showed that metformin reduced the risk of developing diabetes, though to a lesser degree than the intensive lifestyle intervention (a 31% reduction).
Metformin works primarily by reducing the amount of glucose produced by the liver and improving the body’s sensitivity to insulin.
It is most effective in younger adults, people with higher body mass index (BMI), and women with a history of gestational diabetes.
How is Insulin Administered?
Because insulin is a protein, it cannot be taken as a pill. If swallowed, it would be broken down by digestive enzymes in the stomach, just like the protein in food, rendering it useless.
Therefore, it must be delivered directly into the body, bypassing the digestive system.
The most common method is injection into the layer of fat just under the skin (subcutaneous tissue).
Injections: Syringes and Pens
For decades, the standard method of insulin delivery has been a syringe and vial.
Users draw up a precise dose of insulin from a vial into a syringe and inject it. In recent years, insulin pens have become increasingly popular.
These devices contain a cartridge of insulin and allow users to simply dial the desired dose and inject it with a disposable pen needle. Pens offer greater convenience, portability, and dose accuracy, especially for those with vision or dexterity issues.
What is an Insulin Pump and How Does it Work?
An insulin pump is a small, computerized device, about the size of a pager, that delivers a continuous supply of rapid-acting insulin 24 hours a day.
The pump holds an insulin reservoir and is connected to the body via a thin plastic tube called an infusion set, which has a small cannula inserted under the skin. The pump is programmed to deliver:
- A basal rate: A slow, steady trickle of insulin to cover background needs between meals and overnight.
- A bolus dose: A larger dose of insulin that the user programs the pump to deliver at mealtimes to cover the carbohydrates in food.
Modern pumps often integrate with Continuous Glucose Monitors (CGMs) to create “hybrid closed-loop” systems that can automatically adjust insulin delivery based on real-time glucose readings, further mimicking a healthy pancreas.
Understanding Insulin Strength: U-100 vs. U-500
The concentration, or strength, of insulin is measured in units per milliliter (mL). It’s critical to use the correct syringe for your insulin strength to ensure accurate dosing.
- U-100: This is the standard and most common strength in the United States. It means there are 100 units of insulin in every 1 mL of fluid. It is used with U-100 syringes.
- U-500: This is a highly concentrated insulin, five times stronger than U-100. It is reserved for patients who are extremely insulin resistant and require very large daily doses of insulin. Using U-500 insulin requires extreme care and a special U-500 syringe to prevent dangerous overdoses.
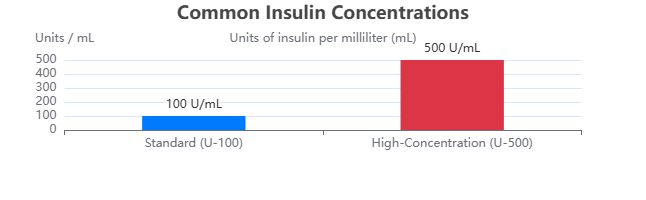
A comparison of standard (U-100) and high-concentration (U-500) insulin, used for severe insulin resistance.
Frequently Asked Questions (FAQ)
1. Can insulin be taken as a pill?
No. Insulin is a protein that would be destroyed by stomach acid and digestive enzymes if taken orally. It must be injected or inhaled to enter the bloodstream effectively and perform its function of regulating blood glucose.
2. What are the symptoms of insulin resistance or prediabetes?
Usually, there are no symptoms. This is why it’s often called a “silent” condition. Some people may develop darkened skin patches (acanthosis nigricans) on the neck or armpits, but diagnosis relies on blood tests.
3. Does everyone with prediabetes develop type 2 diabetes?
No. While prediabetes significantly increases your risk, it is not a guarantee. With proactive lifestyle changes like weight loss, healthy eating, and exercise, many people can return their blood sugar levels to normal and prevent or delay diabetes.
4. What is the difference between insulin and glucagon?
They are opposing hormones. Insulin lowers blood sugar by helping cells absorb glucose. Glucagon raises blood sugar by signaling the liver to release stored glucose. Together, they maintain a stable balance in your bloodstream.
5. Can you be “addicted” to insulin?
No. For people with type 1 diabetes, insulin is a necessary hormone for survival, not an addictive drug. For those with type 2, it’s a tool to manage blood sugar when the body can’t. It replaces a hormone the body is lacking.
6. Does taking insulin mean I have failed at managing my diabetes?
Absolutely not. Type 2 diabetes is a progressive disease. Over time, the pancreas may naturally produce less insulin. Starting insulin therapy is a proactive step to maintain good blood sugar control and prevent long-term complications.
7. Will insulin make me gain weight?
Insulin can contribute to weight gain because it is an energy-storage hormone. When your blood sugar is better controlled, your body is able to use and store glucose more efficiently, which can lead to weight gain if calorie intake isn’t adjusted.
8. What is an insulin pump?
An insulin pump is a small, wearable device that delivers a continuous, customized dose of rapid-acting insulin throughout the day. It provides a background (basal) rate and allows the user to deliver larger (bolus) doses for meals.
9. How is C-peptide related to insulin?
C-peptide is a fragment that is split off from proinsulin to create active insulin. It is released in equal amounts to insulin, so measuring C-peptide levels in the blood is an accurate way to determine how much insulin a person’s own pancreas is producing.
Conclusion
Insulin is far more than just a medication for diabetes, it is a fundamental hormone that sustains life by managing our body’s energy supply.
From its creation in the pancreas to its role as the “key” that unlocks our cells, its function is elegant and vital.
When this system is disrupted by insulin resistance, the consequences can be serious, placing millions at risk for type 2 diabetes and cardiovascular disease.
However, knowledge is power. By understanding how insulin works, the risk factors for resistance, and the diagnostic criteria for prediabetes, you are equipped to take control.
The evidence is clear: lifestyle changes—centered on a healthy diet, regular physical activity, and modest weight loss—are incredibly effective at improving insulin sensitivity and preventing disease.
For those who do require insulin therapy, modern medicine offers a sophisticated toolkit of different types of insulin and delivery systems like the insulin pump to help manage blood sugar with precision.
If you are concerned about your risk or have been diagnosed with prediabetes, the most important step you can take is to speak with your healthcare provider.
Together, you can create a personalized plan to protect your metabolic health for years to come. Don’t wait for symptoms to appear, be proactive today.
Found this article helpful? Share it with friends and family to spread awareness about the critical role of insulin in our health.

