The fastest way to get rid of jock itch is by consistently applying an over-the-counter (OTC) antifungal cream, particularly one from the allylamine class, while maintaining strict hygiene.
With proper care, most mild to moderate cases of this frustrating condition can be resolved within one to three weeks, bringing an end to the persistent itching and discomfort.
If you’re dealing with this issue, you are far from alone. Fungal skin infections are a global health concern, with some estimates suggesting they affect up to 25% of the world’s population.
As noted in research published by the National Center for Biotechnology Information (NCBI), conditions like jock itch are incredibly common, especially in warm, humid climates and among athletes.
This guide is designed to be the definitive resource for understanding and eliminating jock itch.
We will move beyond surface-level advice to provide a deep, evidence-based analysis of the condition.
You will learn how to accurately identify its symptoms, navigate the pharmacy aisle to choose the most effective OTC treatment, understand when professional medical help is non-negotiable, and implement a robust prevention strategy to keep it from returning.
Read on for our expert-vetted, step-by-step plan to find fast relief and reclaim your comfort.
In This Article
What Exactly Is Jock Itch (Tinea Cruris)?
Jock itch, known in the medical community as tinea cruris, is a common superficial fungal infection of the skin.
It is crucial to understand that it is caused by a fungus, not bacteria or poor hygiene alone, although hygiene plays a significant role in its management and prevention.
The term “tinea” refers to a group of fungal infections often called “ringworm”, while “cruris” is Latin for groin, indicating its typical location.
The culprits behind jock itch are a group of fungi called dermatophytes.
These microscopic organisms have a unique and troublesome characteristic: they feed on keratin, the tough, fibrous protein that makes up the outer layer of our skin, as well as our hair and nails.
This is why the infection remains superficial, confined to the stratum corneum (the outermost layer of the epidermis), and doesn’t typically invade deeper tissues in individuals with healthy immune systems.
The pathophysiology is straightforward: dermatophyte spores land on the skin, and if the environment is right—warm, moist, and dark—they germinate, grow, and begin to digest keratin, leading to the characteristic inflammatory rash.
The infection typically manifests in the skin folds of the groin, the inner thighs and the buttocks.
A common misconception is that it affects the genitals (the penis and scrotum in men or the vulva in women), but this is rare for tinea cruris.
A rash directly on the genitals is more likely to be a different condition, such as a yeast infection (candidiasis), and warrants a doctor’s visit.
The rash itself often presents as a half-moon or ring-shaped patch that is reddish-brown in color, with a distinctly raised, scaly, and advancing border.
Furthermore, there is a strong and clinically significant connection between jock itch and athlete’s foot (tinea pedis).
According to the Mayo Clinic, the same dermatophyte species often cause both conditions. This creates a common pathway for autoinoculation, or self-infection.
An individual can unknowingly transfer the fungus from their feet to their groin via their hands or a contaminated towel, leading to a new or recurring case of jock itch.
What Are the Telltale Symptoms of Jock Itch?
Recognizing the symptoms of jock itch is the first step toward effective treatment.
While the name implies an athletic origin, anyone can experience this condition.
The signs can range from mildly annoying to intensely uncomfortable.
Here is a clear checklist of the most common symptoms, which can help you differentiate jock itch from other skin irritations.
Primary Symptoms Checklist:
- Persistent Itching and Burning: This is often the first and most prominent symptom. The itch is typically located in the groin creases, on the inner thighs, or around the buttocks and can be intense, especially after sweating or physical activity.
- A Distinctive Rash: The rash is the key visual identifier. It usually starts as a small, red, tan or brown patch that spreads outward in a half-moon or ring-like shape.
- Raised and Scaly Border: A hallmark of tinea cruris is its well-defined, advancing border. This edge is often more inflamed and scaly than the center of the rash and may contain small blisters or pustules.
- Central Clearing: As the rash expands, the center may begin to heal and clear up, leaving skin that appears relatively normal. This gives the rash its classic “ringworm” appearance.
- Flaking, Peeling, or Cracking Skin: The affected skin can become dry, flaky, and may even crack, especially in the skin folds, which can be painful.
- Worsening with Activity: Symptoms, particularly itching and burning, often intensify with moisture and friction from exercise or tight clothing.
It’s important to note how the rash’s appearance can differ based on skin tone.
On lighter skin, the rash is typically bright red or pink.
On darker skin tones, the rash may appear as a more subtle gray, purple, or brown discoloration, as highlighted by the Cleveland Clinic.
This variation can sometimes make diagnosis more challenging without a close examination of the rash’s texture and border.
The progression of symptoms is also a key indicator. What begins as a minor itch can quickly evolve.
If left untreated, the rash can spread over a large area of the thighs and buttocks, and the constant scratching can lead to breaks in the skin.
These breaks create an entry point for bacteria, potentially causing a secondary bacterial infection, which presents with increased pain, swelling and pus.
What Causes Jock Itch and Who Is at Risk?
Understanding the root causes and risk factors for jock itch is essential for both treatment and prevention.
It’s not simply a matter of being “unclean”, rather, it’s about a specific fungus encountering the perfect environment to thrive.
This section breaks down the fungal culprits and the conditions that put individuals at a higher risk.
The Fungal Culprits
As previously mentioned, jock itch is caused by dermatophyte fungi.
The most common species responsible for tinea cruris worldwide is Trichophyton rubrum.
Other frequently implicated fungi include Epidermophyton floccosum and Trichophyton mentagrophytes.
These fungi are ubiquitous in our environment and can be passed between people, from animals to people or even from contaminated objects.
The “Perfect Storm” Environment
Dermatophytes don’t cause an infection every time they land on the skin.
They require a specific set of conditions to grow and multiply—a “perfect storm” that is commonly found in the groin area:
- Warmth: The groin is naturally one of the warmest parts of the body.
- Moisture: Sweat accumulates easily in this area, especially during exercise or in hot weather.
- Darkness: The area is typically covered by clothing, blocking out light.
- Occlusion: Tight clothing traps heat and moisture, creating a humid microclimate that is ideal for fungal growth.
Primary Risk Factors
Certain individuals are more susceptible to developing jock itch due to their physiology, lifestyle, or health status. Identifying these risk factors is key to prevention.
- Heavy Sweating (Hyperhidrosis): Individuals who sweat profusely provide a constant source of moisture for the fungus to flourish. This is why athletes are commonly affected.
- Wearing Tight, Non-Breathable Clothing: Synthetic fabrics like nylon and polyester trap moisture against the skin. Tight jeans, underwear, or athletic gear prevent air circulation, exacerbating the problem.
- Being Male: Men are about three times more likely to develop jock itch than women. This is partly due to anatomy, as the male groin can trap more heat and moisture.
- Obesity: Excess body weight can lead to deeper skin folds (intertrigo), which are prime locations for moisture and heat to become trapped, creating an ideal breeding ground for fungi.
- Weakened Immune System: Individuals with compromised immune systems due to conditions like HIV/AIDS, chemotherapy, or immunosuppressant drugs are more vulnerable to all types of infections, including fungal ones.
- Diabetes: People with poorly controlled diabetes often have higher blood sugar levels, which can promote fungal growth. They may also have compromised circulation and nerve function, making them more susceptible to skin infections.
- Having a Concurrent Fungal Infection: As noted, having athlete’s foot significantly increases the risk. The fungus can easily be transferred from the feet to the groin.
- Sharing Contaminated Items: The fungus can survive for a period on damp surfaces. Sharing towels, clothing or athletic supporters with an infected person is a direct route of transmission.
How to Get Rid of Jock Itch Fast with OTC Treatments
For most cases of jock itch, the path to relief starts in the aisle of your local pharmacy.
Over-the-counter (OTC) antifungal treatments are highly effective, accessible and the cornerstone of therapy.
However, the variety of options can be confusing.
This section provides an in-depth guide to choosing the right product and using it correctly for the fastest possible results.
Choosing the Right Antifungal: Allylamines vs. Azoles
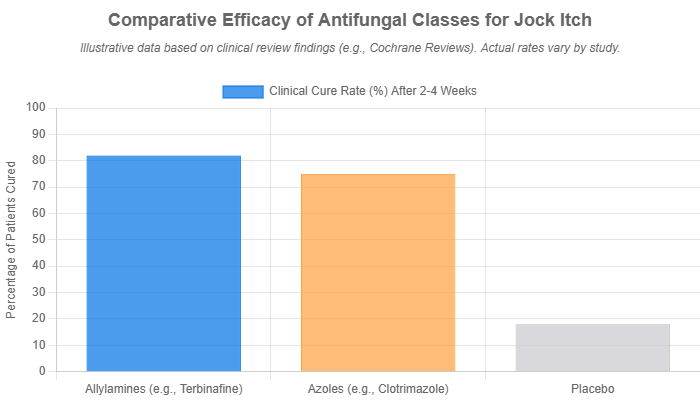
OTC antifungal medications primarily fall into two major classes: allylamines and azoles.
Understanding the difference between them can help you make a more informed choice.
Allylamines (Fungicidal)
Allylamine antifungals, such as terbinafine (found in Lamisil AT) and butenafine (found in Lotrimin Ultra), are generally considered the more powerful option.
They are fungicidal, which means they actively kill the fungal cells by inhibiting an enzyme called squalene epoxidase, a critical component in the fungus’s cell membrane synthesis pathway.
The key advantage of allylamines is their potential for faster results and shorter treatment durations.
Clinical studies have often shown them to have slightly higher cure rates and lower relapse rates compared to azoles.
For instance, a comprehensive Cochrane Review on topical treatments for tinea infections noted that terbinafine was significantly more effective than a placebo and that allylamines may offer a therapeutic edge.
This makes them an excellent first choice for someone seeking rapid relief from jock itch.
Azoles (Fungistatic)
Azole antifungals, including clotrimazole (Lotrimin AF Cream) and miconazole (Micatin, Lotrimin AF Spray) are the other major group.
They are fungistatic, meaning they don’t kill the fungus outright but instead inhibit its growth and reproduction.
They work by disrupting the production of ergosterol, another vital component of the fungal cell membrane.
While they may require a longer treatment course (typically 2-4 weeks), azoles are still highly effective at resolving jock itch.
They have been the standard of care for decades, are widely available, and are often more affordable than their allylamine counterparts.
For mild cases or for those on a budget, an azole-based cream is a very reliable option.
Comparative Table of Common OTC Jock Itch Treatment Creams
To simplify your choice, here is a table comparing some of the most common and effective OTC products for treating jock itch.
This table is designed to help you quickly identify the right product based on its active ingredient and mechanism.
| Active Ingredient | Common Brand Name(s) | Class | Typical Treatment Duration | Key Feature |
|---|---|---|---|---|
| Terbinafine 1% | Lamisil AT | Allylamine (Fungicidal) | 1-2 weeks | Fast-acting; actively kills the fungus. Often recommended for quicker results. |
| Butenafine 1% | Lotrimin Ultra | Allylamine (Fungicidal) | 2 weeks (once daily) | Potent and fast; clinical studies show high efficacy in a short time frame. |
| Clotrimazole 1% | Lotrimin AF Cream, Canesten | Azole (Fungistatic) | 2-4 weeks | Reliable and affordable; stops fungal growth. A long-standing, trusted option. |
| Miconazole 2% | Micatin, Lotrimin AF Powder Spray | Azole (Fungistatic) | 2-4 weeks | Versatile; available in creams, sprays, and powders to help keep the area dry. |
| Tolnaftate 1% | Tinactin, Lamisil AF Defense | Thiocarbamate | 2-4 weeks | Good for prevention; effective for treatment and can also be used to prevent recurrence. |
Step-by-Step Guide to Applying Jock Itch Treatment Cream
Choosing the right cream is only half the battle.
Correct and consistent application is absolutely critical for eradicating the infection and preventing its return. Follow these steps precisely:
- Wash and Dry the Area Thoroughly: Before each application, gently wash the affected groin and thigh area with a mild, unscented soap and warm water. Afterward, pat the area completely dry with a clean towel. Crucially, use a separate towel for the infected area than for the rest of your body to prevent spreading the fungus.
- Apply a Thin, Even Layer: Squeeze a small amount of the antifungal cream (about the size of a pea) onto your fingertip. Gently rub it into the affected skin, creating a thin, even layer. Using too much cream will not speed up healing and can trap moisture.
- Extend Beyond the Rash Border: This is a vital step that many people miss. The fungus is most active at the leading edge of the rash and may be present in the surrounding, seemingly healthy skin. Apply the cream to cover the entire rash and extend it about one to two inches beyond the visible border.
- Wash Your Hands Immediately: After applying the cream, wash your hands thoroughly with soap and water. This prevents you from accidentally spreading the fungal spores to other parts of your body (like your face or hands) or to other people.
- Be Consistent and Complete the Full Course: This is the most important rule. Fungal infections are notoriously stubborn. Even if your symptoms of itching and redness improve within a few days, the fungus is likely still present. You must continue to apply the medication for the full duration recommended on the product label (usually 1-4 weeks). Stopping treatment early is the number one reason for recurrence.
When Should I See a Doctor for Jock Itch?
While most cases of jock itch respond well to OTC treatments, there are situations where self-care is not enough and a professional medical evaluation is necessary.
Ignoring these signs can lead to a chronic infection, complications, or a misdiagnosis of a more serious condition.
Trust and safety are paramount, so it’s important to know when to seek help.
Red Flag Symptoms Requiring Medical Attention:
- No Improvement After Consistent Treatment: If you have been diligently using an OTC antifungal cream as directed for one to two weeks and see no improvement in your symptoms, it’s time to see a doctor.
- The Rash Worsens or Spreads Rapidly: If the rash becomes more painful, the redness intensifies, or it spreads quickly despite treatment, a medical professional should evaluate it.
- Signs of a Secondary Bacterial Infection: Constant scratching can create breaks in the skin, allowing bacteria to enter. If you notice increased swelling, warmth, pain, or the development of pus or oozing from the rash, you may have a secondary infection that requires antibiotics.
- You Develop a Fever: A fever is a sign of a systemic response to an infection and is not a typical symptom of a simple case of jock itch. It warrants an immediate medical consultation.
- The Infection Keeps Coming Back (Chronic Tinea Cruris): If your jock itch clears up with treatment only to return shortly after, you may be dealing with a resistant fungal strain or an unaddressed source of reinfection (like chronic athlete’s foot).
- You Have a Compromised Immune System or Diabetes: Individuals with these conditions are at higher risk for complications and may require more aggressive treatment. It’s always best to manage skin infections under a doctor’s supervision.
- You Are Unsure of the Diagnosis: If the rash looks unusual, involves the genitals, or doesn’t fit the classic description of jock itch, a proper diagnosis is essential.
What to Expect from a Doctor’s Visit
A doctor or dermatologist can provide a definitive diagnosis and a more powerful treatment plan. This may involve:
- Diagnosis Confirmation: To confirm the presence of a fungus, your doctor may perform a simple, painless test called a KOH prep. This involves gently scraping a small sample of skin from the rash’s border, placing it on a slide with a potassium hydroxide (KOH) solution, and examining it under a microscope for fungal hyphae.
- Prescription-Strength Treatments: If OTC products have failed, your doctor can prescribe stronger topical antifungals (e.g., econazole, oxiconazole) or, for severe or widespread infections, oral antifungal pills. Oral medications like terbinafine or itraconazole work systemically to attack the fungus from within and are highly effective for stubborn cases.
- Addressing Inflammation (with caution): In cases of extreme inflammation and itching, a doctor might prescribe a combination cream containing both an antifungal and a mild corticosteroid for a very short period. However, as detailed in resources like the NCBI StatPearls on Tinea Cruris, this must be done with extreme caution. Using a steroid alone on a fungal infection can suppress the immune response, allowing the fungus to flourish and leading to a condition called tinea incognito, where the rash’s appearance is altered, masking the true problem and making it harder to treat.
- Investigating Differential Diagnoses: Several other skin conditions can mimic jock itch. A doctor can differentiate it from:
- Inverse Psoriasis: An autoimmune condition causing smooth, red lesions in skin folds, but without the scaly border.
- Erythrasma: A bacterial infection causing reddish-brown patches in skin folds, which will glow coral-red under a Wood’s lamp.
- Candidiasis (Yeast Infection): Often brighter red, may involve the scrotum or vulva, and typically features small “satellite” pustules around the main rash.
- Contact Dermatitis: An allergic or irritant reaction to a substance, which usually appears more uniform and is directly related to exposure.
Are There Home Remedies That Actually Work for Jock Itch?
In the quest for relief from jock itch, many people turn to home remedies.
While the internet is filled with suggestions, it’s vital to approach them with an evidence-based mindset.
The most effective “home remedies” are actually lifestyle and hygiene practices that create an environment hostile to fungal growth.
Others may offer symptomatic relief but will not cure the underlying infection.
It is critical to understand that home remedies should be viewed as supportive measures to be used alongside proven OTC or prescription antifungal treatments, not as standalone cures for jock itch.
Evidence-Based Supportive Care (The Most Effective “Remedies”)
- Hygiene is #1: Keep the Area Clean and DRY: This is the single most important non-pharmacological intervention. The fungus needs moisture to survive. After bathing or exercising, take extra time to ensure the groin area is completely dry before getting dressed. Use a clean towel every time.
- Wear Loose-Fitting, Breathable Clothing: Ditch the tight synthetic underwear and pants. Switch to loose-fitting cotton boxer shorts and breathable fabrics that allow air to circulate and moisture to evaporate.
- Use a Drying Powder: After drying, applying a non-medicated, talc-free powder can help absorb residual moisture throughout the day. Look for powders containing cornstarch or other absorbents. Avoid powders with fragrances that could irritate the skin.
Natural Antifungals (To Be Used with Caution)
Some natural substances have demonstrated antifungal properties in laboratory settings, but their effectiveness in treating an active jock itch infection on human skin is less certain.
They may help, but should not replace a proper antifungal cream.
- Tea Tree Oil (Melaleuca alternifolia): Several studies suggest that tea tree oil has broad-spectrum antifungal properties. However, it is potent and can cause significant skin irritation if used undiluted.
- How to use (cautiously): Dilute a few drops of tea tree oil in a tablespoon of a carrier oil like coconut or jojoba oil. Perform a patch test on a small area of your arm first to check for an allergic reaction. If no irritation occurs after 24 hours, you can apply the diluted mixture to the affected area once or twice a day.
- Aloe Vera: While not a potent antifungal, aloe vera is well-known for its soothing and anti-inflammatory properties. As noted by the Cleveland Clinic, it can provide temporary relief from the itching and burning associated with jock itch, but it will not eradicate the fungus.
Remedies to AVOID
Some “remedies” found online are not only ineffective but also dangerous.
They can damage your skin’s protective barrier, worsen inflammation, and increase the risk of secondary infection.
- Undiluted Bleach: This is a caustic chemical that can cause severe chemical burns to the skin. Never apply bleach to your skin.
- Rubbing Alcohol or Hydrogen Peroxide: While these are disinfectants, they are extremely harsh and drying on inflamed skin. Applying them to the delicate groin area will cause intense stinging and pain, damage skin tissue and delay healing.
- Undiluted Apple Cider Vinegar: While some claim it has antifungal properties, applying undiluted vinegar can cause chemical burns and severe irritation.
How Can I Prevent Jock Itch from Coming Back?
Curing an active case of jock itch is a great achievement, but the ultimate goal is to prevent it from ever returning.
Because the fungi that cause it are common, prevention relies on consistently maintaining an environment that is inhospitable to their growth.
This proactive, long-term plan can help you break the cycle of reinfection.
Your Proactive Prevention Checklist:
- Dry Off Smart: This is a simple but powerful habit. After showering or swimming, always dry your feet last. Or, even better, use two separate towels: one for your body and one for your feet. This prevents you from transferring athlete’s foot fungus (tinea pedis) from your feet to your groin.
- Implement Daily Clothing Changes: Change your underwear at least once a day, or more often if you sweat heavily. Never re-wear workout clothes without washing them first. Damp, sweaty clothes are a perfect breeding ground for fungi.
- Wash Clothes and Towels in Hot Water: To effectively kill fungal spores, wash your towels, underwear, socks, and athletic wear in hot water (at least 140°F or 60°C) with a good quality detergent.
- Choose Your Fabrics Wisely: Opt for underwear and clothing made from natural, breathable fabrics like cotton or moisture-wicking synthetic blends designed for athletic wear. Avoid tight-fitting clothes that trap heat and moisture. Many people find that switching from briefs to boxer shorts helps improve air circulation.
- Don’t Share Personal Items: Fungi can be transmitted via contaminated objects. Never share towels, clothing or athletic supporters with others.
- Treat Athlete’s Foot Promptly and Aggressively: Since athlete’s foot is a major reservoir for the fungus that causes jock itch, you must treat it as soon as you notice symptoms (itching, scaling, or blisters between the toes). A persistent case of athlete’s foot almost guarantees a recurrence of jock itch.
- Protect Your Feet in Public Areas: Always wear waterproof sandals or shower shoes in public locker rooms, gyms, showers, and around swimming pools to avoid picking up the fungus in the first place.
- Consider a Prophylactic Powder: If you are prone to sweating or live in a humid climate, using an OTC antifungal powder (like one containing miconazole or tolnaftate) in your groin area and on your feet after showering can help absorb moisture and prevent fungal growth.
What Should I Know About Antifungal-Resistant Jock Itch?
One of the most significant and emerging challenges in dermatology is the rise of antifungal-resistant dermatophytes.
This is a topic most general articles on jock itch fail to cover, but it is crucial for understanding why some infections are so difficult to treat.
Just as bacteria can become resistant to antibiotics, fungi are evolving to withstand standard antifungal medications.
Recently, dermatologists and public health officials have raised alarms about new, highly contagious, and hard-to-treat strains of ringworm fungi.
A notable example is Trichophyton indotineae, a strain that has spread from South Asia to Europe and North America.
This strain often shows resistance to terbinafine, one of the most common and effective oral antifungals.
The Centers for Disease Control and Prevention (CDC) has issued alerts to healthcare providers to be aware of these emerging threats.
What Causes Antifungal Resistance?
Several factors contribute to the development of resistance, and patient behavior plays a significant role:
- Incomplete Treatment Courses: When a patient stops using an antifungal cream or pill as soon as their symptoms improve, they may not have fully eradicated the fungus. The surviving, more resilient fungi can then multiply, leading to a recurrent infection that is harder to treat.
- Misuse of Combination Steroid-Antifungal Creams: The widespread, improper use of creams that mix a potent steroid with an antifungal is a major driver of resistance. The steroid suppresses inflammation, making the patient feel better quickly, but it also dampens the local immune response, allowing the fungus to thrive and potentially develop resistance mutations.
- Over-the-Counter Access and Misdiagnosis: Patients self-treating what they think is jock itch with the wrong product or for the wrong duration can inadvertently contribute to the problem.
What This Means for You
If you have a case of jock itch that simply won’t go away despite following all the rules of OTC treatment, you could be dealing with a resistant strain.
It is absolutely essential to see a dermatologist in this situation.
A dermatologist can perform a fungal culture, where a skin sample is sent to a lab to grow the fungus and identify the specific species.
The lab can also perform susceptibility testing to see which antifungal medications will be effective against that particular strain.
Treatment for resistant infections often requires longer courses of different, sometimes more powerful, oral antifungal medications like itraconazole or voriconazole, managed carefully by a specialist.
This emerging threat underscores the importance of using all medications, including simple OTC creams, exactly as directed.
By completing the full course of treatment, you not only ensure your own infection is cured but also help prevent the development and spread of drug-resistant fungi in the community.
Frequently Asked Questions (FAQ) about Jock Itch
1. How long does jock itch last?
With proper and consistent OTC treatment, a typical case of jock itch resolves in 1 to 3 weeks. If left untreated, the fungal infection can persist for months, potentially spreading to other areas and becoming more difficult to cure.
2. Can women get jock itch?
Yes, women can get jock itch, although it is much less common than in men. The symptoms, causes (fungus thriving in moisture), and treatments are generally the same, affecting the skin of the groin, inner thighs, and buttocks.
3. Is jock itch an STD?
No, jock itch is a fungal skin infection, not a sexually transmitted disease (STD). However, because it is contagious, it can be spread from person to person through close skin-to-skin contact, including sexual activity, or by sharing contaminated items.
4. Should I use a steroid cream like hydrocortisone on jock itch?
No. Using a steroid cream alone on a fungal infection is a bad idea. It can suppress the local immune response, allowing the fungus to spread unchecked. This can also alter the rash’s appearance (a condition called tinea incognito), making it harder to diagnose and treat.
5. What’s the difference between jock itch and chafing?
Chafing is skin irritation caused by friction, appearing as red, sore, and sometimes raw skin, but it usually lacks a defined, scaly border. Jock itch is a fungal infection with a distinct, often ring-shaped, itchy rash with a raised edge.
6. Can I get jock itch on my penis or scrotum?
It is very rare for true jock itch (tinea cruris) to affect the penis or scrotum. A rash on the genitals is more likely to be another condition, such as a yeast infection (candidiasis) or contact dermatitis, and requires a doctor’s evaluation for an accurate diagnosis.
7. Does rubbing alcohol kill jock itch?
While alcohol can kill fungus on surfaces, applying it directly to inflamed skin is not recommended. It will cause severe stinging, pain, and excessive dryness, which can damage the skin’s protective barrier and ultimately worsen the problem and delay healing.
8. Why does my jock itch keep coming back?
Recurrence is often due to one of three main reasons: not completing the full antifungal treatment course, constant reinfection from an untreated case of athlete’s foot, or failing to address underlying risk factors like excessive moisture and wearing tight, non-breathable clothing.
Conclusion
Dealing with the relentless itch and discomfort of jock itch can be a frustrating experience, but it is a highly treatable and preventable condition.
Armed with the right knowledge and a consistent plan, you can achieve fast relief and keep the infection from returning.
The path to success is built on three fundamental pillars:
- Treat Effectively: Choose a proven OTC antifungal medication. For faster results, consider an allylamine-based cream like terbinafine or butenafine. Apply it correctly, extending beyond the rash border.
- Treat Completely: The single most important factor in preventing recurrence is to complete the full treatment course as directed on the label, even after your symptoms have disappeared.
- Prevent Proactively: The ultimate cure is prevention. Prioritize keeping the groin area clean and, most importantly, dry. Wear breathable clothing, treat athlete’s foot immediately, and never share towels.
While self-treatment is effective for most, it is equally important to recognize its limits.
If your condition does not improve, worsens, or if you are ever in doubt about the diagnosis, do not hesitate to consult a healthcare professional.
They can provide a definitive diagnosis, access to prescription-strength treatments, and a personalized care plan to address stubborn or recurrent infections.
Take control of your comfort today.
By understanding the science behind jock itch and implementing these evidence-based strategies, you can confidently and effectively manage this common condition.
Have a question or a tip that worked for you? Share it in the comments below to help others in the community!
Reference
[1] Jock Itch: Causes, Treatment, Prevention – WebMD
https://www.webmd.com/men/causes-and-prevent-jock-itch
[2] Jock itch – Symptoms and causes
https://www.mayoclinic.org/diseases-conditions/jock-itch/symptoms-causes/syc-20353807
[3] Tinea Cruris – StatPearls
https://www.ncbi.nlm.nih.gov/books/NBK554602
[4] Tinea Cruris (Jock Itch) – Dermatologic Disorders
[5] an overview on pharmacotherapy of jock itch (tinea cruris)
[6] Jock Itch: What It Is, Symptoms & Treatment – Cleveland Clinic
https://my.clevelandclinic.org/health/diseases/22141-jock-itch-tinea-cruris
[7] Jock itch Information | Mount Sinai – New York
https://www.mountsinai.org/health-library/diseases-conditions/jock-itch
[8] Jock Itch: Treatments and Symptoms (With Pictures) – GoodRx
[9] What is the best way to treat tinea cruris? – PubMed

