Getting rid of acne fast involves a multi-pronged approach that combines effective over-the-counter products, smart lifestyle choices, and, when necessary, powerful prescription treatments from a dermatologist.
While “fast” is relative in dermatology—often meaning weeks, not hours—significant improvement can be achieved by targeting the root causes of acne: excess oil, clogged pores, bacteria and inflammation.
In fact, acne is the most common skin condition in the United States, affecting up to 50 million Americans annually.
This guide will break down the science behind acne and provide a clear, evidence-based roadmap to clearer skin.
You will learn to identify your specific acne type, choose the right treatments and understand when it’s crucial to seek professional help to prevent long-term scarring and emotional distress.
Read on to take control of your skin health.
In This Article
1. What Exactly Is Acne and Why Do I Get It?
At its core, acne is an inflammatory disorder of the skin’s pilosebaceous units, which consist of a hair follicle and its associated sebaceous (oil) gland.
According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the condition occurs when these follicles become clogged with a mixture of oil (sebum) and dead skin cells.
This blockage creates the perfect environment for bacteria to thrive, leading to inflammation and the lesions we commonly call pimples or zits.
Here’s a step-by-step breakdown of how a pimple forms:
- Excess Sebum Production: Sebaceous glands produce an oily substance called sebum to lubricate the skin and hair. Hormonal fluctuations can cause these glands to produce too much oil.
- Follicular Hyperkeratinization: Dead skin cells (keratinocytes) don’t shed properly and instead clump together, mixing with the excess sebum.
- Pore Blockage: This sticky mixture forms a plug, blocking the hair follicle. This initial blockage is called a microcomedone, which is invisible to the naked eye.
- Bacterial Growth: A bacterium that normally lives on the skin, Cutibacterium acnes (formerly Propionibacterium acnes), begins to multiply rapidly within the clogged follicle.
- Inflammation: The body’s immune system responds to the bacterial overgrowth, sending white blood cells to fight the infection. This immune response causes the redness, swelling and pain characteristic of inflammatory acne.
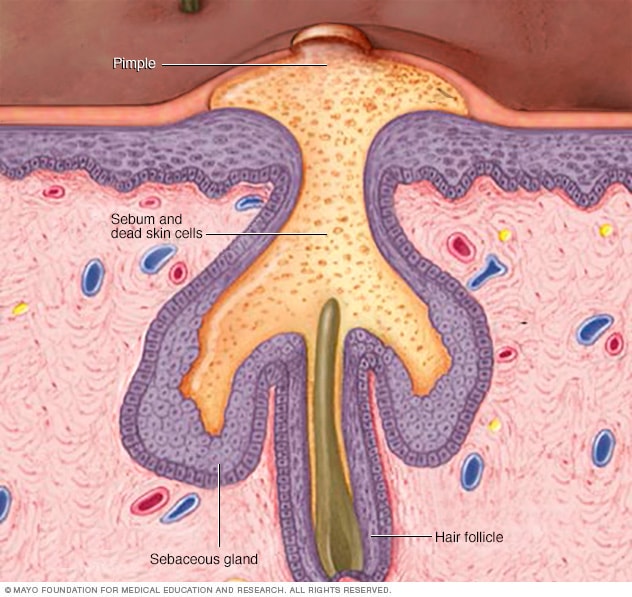
This illustration shows how a hair follicle becomes clogged, leading to the formation of acne.
Acne most commonly appears on the face, forehead, chest, upper back and shoulders because these areas have the highest concentration of sebaceous glands.
While it’s most prevalent among teenagers—affecting about 85% of adolescents—it can persist into or even begin in adulthood.
A 2024 study highlighted the increasing global burden of acne, noting that its prevalence has been rising since 1990, particularly among young people.
The study found that in 2021, acne was about 25% more common in young women than in young men.
2. What Are the Different Types of Acne?
Understanding the specific type of acne you have is the first step toward effective treatment.
Not all blemishes are the same, and they are broadly categorized into two groups: non-inflammatory and inflammatory.
Many people experience a combination of types.
Non-Inflammatory Acne
This type of acne is characterized by clogged pores without significant redness or swelling. It includes:
- Whiteheads (Closed Comedones): These are hair follicles that are completely blocked, trapping sebum and dead skin cells beneath the skin’s surface. They appear as small, flesh-colored or whitish bumps.
- Blackheads (Open Comedones): These are similar to whiteheads, but the pore is open at the surface. The black color is not dirt, it’s the result of the trapped sebum and skin cells oxidizing (reacting with oxygen) when exposed to air.
Inflammatory Acne
This occurs when the follicle wall ruptures, allowing bacteria and sebum to spill into the surrounding skin, triggering an immune response.
This is often more painful and has a higher risk of scarring.
- Papules: Small, red, tender bumps. They are inflamed comedones where the follicle wall has a minor break.
- Pustules: Often called pimples, these are papules with a white or yellow center filled with pus (a collection of dead white blood cells, bacteria and debris).
- Nodules: Large, solid, painful lumps that are lodged deep within the skin. They form from a deep rupture in the follicle wall and can persist for weeks or months.
- Cysts: The most severe form of acne. These are large, soft, painful, pus-filled lumps deep under the skin. Cystic acne carries the highest risk of causing permanent scars.
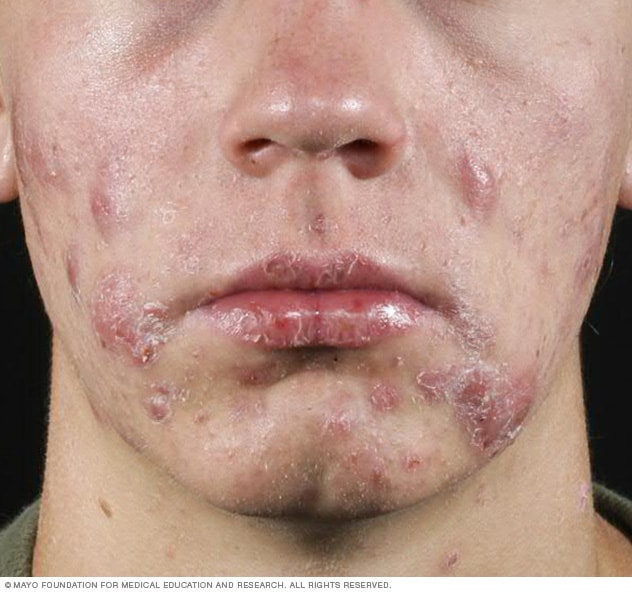
Cystic acne, the most severe form, involves deep, painful, pus-filled lesions that can lead to scarring.
Clinical Insight: It’s crucial to differentiate between acne and other conditions that can look similar, such as rosacea, perioral dermatitis, or hidradenitis suppurativa.
A dermatologist can provide an accurate diagnosis, which is essential for effective treatment.
Acne Severity Classification
Dermatologists often classify acne severity to guide treatment decisions:
- Mild Acne: Mostly whiteheads and blackheads, with a few papules and pustules.
- Moderate Acne: More widespread whiteheads and blackheads, with numerous papules and pustules.
- Severe Acne: Extensive papules and pustules, along with painful nodules and/or cysts. Scarring is common.
| Category | Type | Appearance | Primary Cause | Risk of Scarring |
|---|---|---|---|---|
| Non-Inflammatory | Whitehead (Closed Comedone) | Small, skin-colored bump | Completely blocked pore | Very Low |
| Blackhead (Open Comedone) | Small, dark bump with open center | Partially blocked pore, oxidized sebum | Very Low | |
| Inflammatory | Papule | Small, red, tender bump | Inflammation from follicle wall break | Low |
| Pustule (Pimple) | Red bump with a pus-filled tip | Inflammation and pus formation | Low to Moderate | |
| Nodule | Large, hard, painful lump under the skin | Deep follicle rupture and inflammation | High | |
| Cyst | Large, soft, painful, pus-filled lump | Severe inflammation and infection | Very High |
3. What Are the Main Causes and Triggers of Acne?
While the direct mechanism of acne is clogged pores, several underlying factors can cause or worsen the condition.
The Mayo Clinic identifies four main factors: excess oil production, clogged hair follicles, bacteria and inflammation.
These are influenced by a variety of internal and external triggers.
Primary Influencing Factors
- Hormonal Changes: Androgens, which are hormones that increase during puberty in both boys and girls, cause sebaceous glands to enlarge and produce more sebum. For women, hormonal fluctuations related to the menstrual cycle, pregnancy and conditions like Polycystic Ovary Syndrome (PCOS) are major triggers for breakouts, often referred to as hormonal acne.
- Family History (Genetics): If your parents had acne, you are more likely to develop it too. Genetics plays a significant role in your skin’s predisposition to acne, influencing factors like sebum production and inflammatory response.
- Medications: Certain drugs can induce or worsen acne. Examples include corticosteroids, testosterone, lithium and some anticonvulsants.
- Age: While most common in teenagers, adult acne is increasingly prevalent, particularly in women over 25.
Potential Triggers and Aggravating Factors
- Stress: While stress doesn’t directly cause acne, it can make existing acne worse. When you’re stressed, your body produces more cortisol and androgens, which can stimulate oil glands and increase inflammation.
- Diet: The link between diet and acne is complex and still being studied. However, emerging evidence suggests that certain foods may worsen acne in some individuals. High-glycemic-index foods (like white bread, sugary snacks and processed carbohydrates) and dairy products (especially skim milk) have been associated with increased breakouts.
- Friction or Pressure on Skin: Anything that rubs against your skin and traps sweat and oil can lead to breakouts. This is known as acne mechanica and can be caused by cellphones, helmets, tight collars, backpacks and face masks (“maskne”).
- Greasy or Oily Substances: Using oily cosmetics, lotions, or hair products can clog pores. Look for products labeled non-comedogenic, meaning they are formulated not to cause pore blockages.
Common Acne Myths Debunked
It’s just as important to know what doesn’t cause acne to avoid ineffective or harmful practices.
Myth 1: Acne is caused by dirty skin.
Fact: Acne is an inflammatory condition that starts deep inside the pore, not on the surface. In fact, scrubbing your skin too hard or cleansing with harsh soaps can irritate the skin and worsen acne.
Myth 2: Eating chocolate and greasy foods causes pimples.
Fact: Decades of research have found little to no direct link between eating chocolate or greasy foods and developing acne. The stronger dietary link is with high-glycemic foods and dairy.
Myth 3: You should let acne run its course.
Fact: Without treatment, acne can lead to permanent scarring, skin discoloration (post-inflammatory hyperpigmentation), and significant psychological distress. Early and effective treatment is key.
4. How Can I Treat Mild Acne at Home (OTC Options)?
For mild to moderate acne, over-the-counter (OTC) products can be highly effective.
The key is to choose the right active ingredients and use them consistently.
Results are not immediate, it typically takes 4-8 weeks to see a noticeable improvement.
Key Over-the-Counter Active Ingredients
According to the American Academy of Dermatology (AAD), the following ingredients are mainstays of OTC acne treatment.
1. Benzoyl Peroxide
- How it works: It kills C. acnes bacteria, helps remove excess oil and exfoliates dead skin cells.
- Available in: Cleansers, lotions, creams, and gels in strengths from 2.5% to 10%.
- How to use: Start with a lower concentration (2.5% or 5%) to minimize irritation. It can be used as a spot treatment or applied as a thin layer over acne-prone areas. Be aware that it can bleach hair and fabrics.
2. Salicylic Acid
- How it works: It’s a beta-hydroxy acid (BHA) that exfoliates the skin and penetrates into pores to dissolve oil and dead skin cell plugs. It’s particularly effective for blackheads and whiteheads.
- Available in: Cleansers, toners, pads, and leave-on treatments, typically in 0.5% to 2% concentrations.
- How to use: Can be used once or twice daily. It’s generally less irritating than benzoyl peroxide but can still cause dryness.
3. Adapalene (A Retinoid)
- How it works: Adapalene (brand name Differin 0.1% gel) is a topical retinoid that was previously available only by prescription. It works by regulating skin cell turnover to prevent pores from becoming clogged. It also has anti-inflammatory properties.
- Available in: A 0.1% gel.
- How to use: Apply a pea-sized amount to the entire face (not just as a spot treatment) once daily, usually at night. It can cause initial dryness, redness and peeling, so start by using it every other night. Sun sensitivity is increased, so daily sunscreen is essential.
4. Azelaic Acid
- How it works: This naturally occurring acid has antibacterial properties, reduces inflammation and helps clear pores. It’s also effective at reducing post-inflammatory hyperpigmentation (dark spots).
- Available in: OTC products often contain lower strengths (around 10%), while prescription versions are stronger (15-20%).
- How to use: Can be applied once or twice daily. It’s generally well-tolerated and is considered a safe option during pregnancy.
Building a Basic Anti-Acne Skincare Routine
- Cleanse Gently: Wash your face twice a day (morning and night) and after sweating. Use a gentle, non-abrasive cleanser and your fingertips, not a washcloth or scrub brush.
- Apply Treatment: After cleansing, apply your chosen OTC active ingredient. A common and effective strategy is to use a benzoyl peroxide cleanser in the morning and a leave-on adapalene gel at night.
- Moisturize: Acne treatments can be drying. Use a lightweight, oil-free, non-comedogenic moisturizer to maintain your skin’s barrier.
- Protect from the Sun: Many acne treatments (especially retinoids) increase sun sensitivity. Apply a broad-spectrum, non-comedogenic sunscreen with an SPF of 30 or higher every single morning. This also helps prevent dark spots from worsening.
Pro Tip: Don’t layer too many active ingredients at once, as this can lead to severe irritation. Start with one or two products and introduce them slowly. Consistency is more important than intensity.
5. When Should I See a Dermatologist for My Acne?
While OTC treatments are great for mild cases, professional medical help is often necessary for more persistent or severe acne.
Seeing a dermatologist early can prevent years of frustration, reduce the risk of permanent scarring, and address the psychological impact of the condition.
You should schedule an appointment with a dermatologist if:
- Your acne is not improving after 8-12 weeks of consistent OTC treatment. If you’ve given a good routine a fair shot with no results, it’s time for something stronger.
- You have moderate to severe acne. This includes having many inflamed papules and pustules, or any painful nodules or cysts. These types of acne rarely respond to OTC products alone.
- Your acne is causing scarring. Any sign of pitted or raised scars is a clear signal to seek immediate professional care to prevent further damage.
- Your acne is causing significant emotional distress. If acne is affecting your self-esteem, social life, or causing anxiety or depression, a dermatologist can help you get it under control. Studies show a strong link between acne and mental health issues.
- You suspect your acne is linked to an underlying medical condition. For women, sudden severe acne can be a sign of a hormonal imbalance like PCOS. A sudden onset of severe acne in an older adult can also signal an underlying disease.
FDA Warning: The Food and Drug Administration (FDA) warns that some popular nonprescription acne products can cause a rare but serious allergic reaction. Seek emergency medical help if you experience faintness, difficulty breathing, or swelling of the eyes, face, lips, or tongue after using a new skin product.
6. What Prescription Treatments Can a Dermatologist Offer?
A dermatologist has access to a wide range of powerful medications and therapies to create a personalized treatment plan.
According to the 2024 AAD Guidelines for the Management of Acne Vulgaris, treatment often involves a combination of topical and/or oral medications.
Topical Prescription Medications
These are applied directly to the skin and are the foundation of most acne treatment plans.
- Topical Retinoids: Stronger than OTC adapalene, these include tretinoin, tazarotene, and trifarotene. They are highly effective at preventing clogged pores and reducing inflammation.
- Topical Antibiotics: Clindamycin and erythromycin are used to kill C. acnes bacteria and reduce inflammation. To prevent antibiotic resistance, they are almost always prescribed in combination with benzoyl peroxide.
- Combination Products: Many prescription topicals combine ingredients for convenience and enhanced efficacy, such as clindamycin/benzoyl peroxide, or adapalene/benzoyl peroxide.
- Clascoterone: A newer topical medication that works by blocking androgen hormones at the skin level, reducing sebum production.
Oral Medications (Systemic Treatments)
For moderate to severe acne, or acne that doesn’t respond to topicals, oral medications are used.
- Oral Antibiotics: Tetracyclines (doxycycline, minocycline) and sarecycline are commonly used to reduce bacteria and inflammation. They are typically prescribed for the shortest duration possible (usually 3-6 months) and used alongside topical treatments.
- Combined Oral Contraceptives (Birth Control Pills): For women, certain FDA-approved birth control pills can be very effective for hormonal acne by regulating hormones that contribute to sebum production.
- Anti-Androgen Agents (Spironolactone): This medication is used off-label for women to treat hormonal acne. It works by blocking the effect of androgen hormones on oil glands. It is highly effective for deep, tender acne along the jawline and lower face.
- Isotretinoin (formerly Accutane): This oral retinoid is the most powerful and effective treatment available for severe, nodular, or treatment-resistant acne. It addresses all four causes of acne. However, it has significant potential side effects, including severe birth defects if taken during pregnancy, and requires strict monitoring by a dermatologist through the FDA’s iPLEDGE program.
| Treatment Type | Examples | How It Works | Best For |
|---|---|---|---|
| OTC Topicals | Benzoyl Peroxide, Salicylic Acid, Adapalene 0.1% | Kills bacteria, unclogs pores, normalizes skin cell turnover | Mild to moderate acne, blackheads, whiteheads |
| Prescription Topicals | Tretinoin, Tazarotene, Clindamycin/BPO, Clascoterone | Stronger pore-unclogging, anti-inflammatory, antibacterial effects | Mild to severe acne |
| Oral Antibiotics | Doxycycline, Minocycline, Sarecycline | Reduces bacteria and systemic inflammation | Moderate to severe inflammatory acne |
| Hormonal Therapies | Oral Contraceptives, Spironolactone | Regulates hormones to decrease oil production | Hormonal acne in women |
| Oral Retinoid | Isotretinoin | Dramatically reduces oil production, bacteria, inflammation and clogged pores | Severe, scarring, or treatment-resistant acne |
7. Are There Advanced Therapies for Stubborn Acne and Scars?
In addition to medication, dermatologists can perform in-office procedures to help clear acne faster and treat the scars it leaves behind.
In-Office Procedures for Active Acne
- Corticosteroid Injections: For large, painful nodules or cysts, a dermatologist can inject a diluted steroid directly into the lesion. This rapidly reduces inflammation, pain, and size within 24-48 hours, and can help prevent scarring.
- Drainage and Extraction: A dermatologist can use sterile tools to safely extract blackheads and whiteheads or drain large cysts that haven’t responded to other treatments. This should never be attempted at home due to high risk of scarring and infection.
- Chemical Peels: Using solutions like salicylic, glycolic, or retinoic acid, a chemical peel exfoliates the top layers of skin, helping to unclog pores and improve skin texture. A series of peels is usually required.
- Light and Laser Therapies: Various light-based treatments, including blue light, red light, and pulsed dye lasers (PDL), can help reduce C. acnes bacteria and inflammation. While they can be effective, multiple sessions are needed and they are often used in combination with other treatments.
Treatments for Acne Scars
Once active acne is under control, the focus can shift to treating any remaining scars.
The best treatment depends on the scar type (atrophic/pitted vs. hypertrophic/raised).
- Laser Resurfacing: Ablative (e.g., CO2, Erbium) and non-ablative lasers are used to stimulate collagen production and smooth the skin’s surface.
- Microneedling: This procedure uses fine needles to create controlled micro-injuries in the skin, which stimulates the body’s natural wound healing process and boosts collagen production.
- Radiofrequency (RF) Microneedling: Combines microneedling with radiofrequency energy delivered deep into the dermis, providing more robust collagen remodeling and scar improvement.
- Dermal Fillers: Injectable fillers can be used to temporarily lift and fill in certain types of atrophic scars, making them less noticeable.
- Scar Surgery (Subcision): A minor surgical procedure where a needle is inserted under the skin to break up the fibrous bands that pull the scar down, allowing the skin to rise and level out.
8. Can Lifestyle and Diet Changes Really Help My Acne?
While medication is the most direct way to treat moderate to severe acne, certain lifestyle and dietary habits can support your treatment plan and help prevent future breakouts.
Evidence-Based Dietary Considerations
- Low-Glycemic Diet: A diet rich in low-glycemic-index foods (whole grains, legumes, vegetables) may help improve acne. High-glycemic foods cause rapid spikes in blood sugar and insulin, which can increase inflammation and sebum production.
- Dairy Intake: Some studies have shown a correlation between milk consumption (particularly skim milk) and acne. If you suspect dairy is a trigger, you could try eliminating it for a few weeks to see if your skin improves.
- Omega-3 Fatty Acids: Foods rich in omega-3s, like fatty fish (salmon, mackerel) and walnuts, have anti-inflammatory properties that may help reduce inflammatory acne.
Helpful Lifestyle Habits
- Manage Stress: Practice stress-reduction techniques like meditation, yoga, deep breathing, or regular exercise. Getting enough sleep is also crucial for hormone regulation and stress management.
- Hands Off: Avoid touching, picking, or squeezing your blemishes. This can push bacteria deeper into the skin, worsen inflammation, and lead to permanent scarring.
- Cleanse Post-Workout: Shower or wash your face as soon as possible after exercising to remove sweat, oil, and bacteria that can clog pores.
- Choose Products Wisely: Use only non-comedogenic and oil-free makeup, sunscreen and hair products. Always remove makeup before going to bed.
- Wash Items That Touch Your Face: Regularly wash pillowcases, hats, headbands and makeup brushes to remove oil, dirt and bacteria.
9. How Does Acne Affect Mental Health and How to Cope?
The impact of acne is more than skin deep.
The condition can have profound psychological and social effects, which are not always related to its clinical severity.
Research has consistently shown a link between acne and an increased risk of developing anxiety, depression, low self-esteem and social isolation.
A 2023 study published in Nature confirmed that acne and its associated psychological distress have a significant negative impact on a patient’s self-esteem and quality of life.
This highlights the need for a holistic approach to care that addresses both the physical and emotional aspects of the condition.
Coping Strategies:
- Seek Effective Treatment: The single best thing you can do for your mental health is to get your acne under control. Seeing a dermatologist and starting an effective treatment plan can lead to significant improvements in mood and self-confidence.
- Talk About It: Don’t suffer in silence. Talk to trusted friends, family, or a mental health professional about how you’re feeling. Support groups, either online or in-person, can also connect you with others who understand what you’re going through.
- Focus on What You Can Control: While you can’t make acne disappear overnight, you can control how you manage it. Focus on consistently following your skincare routine and celebrating small improvements.
- Practice Self-Compassion: Your worth is not defined by your skin. Be kind to yourself and shift your focus from your skin to your positive attributes, hobbies and passions.
- Limit Mirror Time: Constantly examining your skin in the mirror can increase stress and the urge to pick. Try to limit how often you scrutinize your reflection.
Frequently Asked Questions (FAQ)
1. How long does it take for acne treatments to work?
Most acne treatments, both OTC and prescription, take 4 to 8 weeks to show noticeable results. Full clearing can take many months. Consistency is crucial, as treatments work by preventing new acne, not just treating existing spots.
2. Can I get rid of a pimple overnight?
You cannot fully eliminate a pimple overnight, but you can reduce its inflammation and appearance. Applying a spot treatment with benzoyl peroxide or salicylic acid, or a hydrocolloid patch, can help. For a large, painful cyst, a dermatologist can administer a cortisone shot for rapid improvement.
3. Is it okay to pop my pimples?
No. Popping pimples can force bacteria and pus deeper into the skin, leading to more inflammation, infection, and a higher risk of permanent scarring and dark spots. It’s best to let blemishes heal on their own or be extracted by a professional.
4. Does toothpaste work on pimples?
This is a myth. While some ingredients in toothpaste like triclosan might have antibacterial effects, toothpaste also contains harsh ingredients that can severely irritate, burn and dry out the skin, ultimately making the breakout look worse.
5. What is the difference between acne and rosacea?
Acne is characterized by comedones (blackheads and whiteheads), papules and pustules. Rosacea typically involves persistent facial redness, flushing, and inflammatory bumps, but it does not have comedones. A dermatologist can distinguish between the two, as treatments differ.
6. Will my acne go away on its own after my teen years?
For many people, acne improves after puberty. However, adult acne is very common, especially in women. It’s not advisable to simply wait for it to go away, as untreated acne can lead to permanent scarring and emotional distress.
7. Can makeup make my acne worse?
Yes, if you use heavy, oily, or pore-clogging (comedogenic) makeup. To avoid this, choose products labeled “non-comedogenic” or “oil-free”. Always remove your makeup completely before sleeping to allow your skin to breathe and regenerate.
8. Is sun exposure good for acne?
While a tan might temporarily mask the redness of acne, sun exposure can damage the skin, worsen post-inflammatory hyperpigmentation (dark spots) and increase the risk of skin cancer. Furthermore, many acne medications make your skin more sensitive to the sun.
Conclusion
Getting rid of acne is a marathon, not a sprint.
While the desire for a “fast” fix is understandable, the most effective and sustainable approach involves understanding your skin, using evidence-based treatments consistently and adopting healthy lifestyle habits.
From powerful OTC ingredients like benzoyl peroxide and adapalene to transformative prescription medications like isotretinoin, there are more effective options available today than ever before.
Remember the key takeaways:
- Identify your acne type to choose the right treatment.
- Be consistent with your skincare routine, results take time.
- Protect your skin with a non-comedogenic moisturizer and daily sunscreen.
- Don’t pick or pop your pimples to prevent scarring.
- Know when to seek help. If your acne is severe, scarring, or impacting your mental health, a board-certified dermatologist is your greatest ally.
Your journey to clear skin is unique. By arming yourself with knowledge and seeking professional guidance, you can take control of your acne and achieve the healthy, clear skin you deserve.
Ready to take the next step? If you’ve struggled with acne and OTC products aren’t working, schedule a consultation with a board-certified dermatologist to discuss a personalized treatment plan.
We’d love to hear from you! Share your own experiences or questions about dealing with acne in the comments below.
Disclaimer
The information provided in this article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read here.

