The search for “high blood pressure symptoms” is one of the most common health queries online, yet it is based on a dangerous misconception.
The stark reality is that high blood pressure (hypertension) typically has no symptoms.
This is precisely why it has earned the ominous title of the “silent killer”—it can inflict significant, irreversible damage long before a person ever feels unwell. This silent epidemic is staggering in its scale.
According to the latest data from the Centers for Disease Control and Prevention (CDC), nearly half of all adults in the United States (48.1%, or about 120 million people) have high blood pressure.
For hundreds of thousands each year, it becomes a primary or contributing cause of life-threatening events like heart attacks and strokes.
This creates a confusing paradox: if hypertension is symptomless, why do so many people associate it with headaches, dizziness, or nosebleeds? And when do symptoms actually become a critical warning sign?
This article will demystify the nature of high blood pressure, clarifying the crucial difference between the silent, chronic condition and the loud alarm bells of a hypertensive crisis.
In the sections that follow, you will gain a comprehensive understanding of what your blood pressure numbers mean, the hidden risks that accumulate over time, and why symptoms are so conspicuously absent.
Most importantly, you will learn to recognize the rare but life-threatening emergency signs and discover actionable, evidence-based strategies to manage and lower your blood pressure.
Continue reading to arm yourself with the knowledge to protect your long-term health.
In This Article
What Is High Blood Pressure (Hypertension)? Decoding the Numbers
Before we can understand its effects, we must first define what high blood pressure truly is.
At its core, blood pressure is a simple measurement of force. It is the force exerted by circulating blood against the walls of your body’s main arteries.
While some pressure is necessary to move blood, when that pressure is consistently too high, it forces your heart to work overtime and can damage your arteries, leading to a cascade of health problems.
What Do Blood Pressure Numbers Actually Mean?
A blood pressure reading is always given as two numbers, one over the other, measured in millimeters of mercury (mm Hg).
- Systolic Pressure (the top number): This measures the pressure in your arteries when your heart beats or contracts, pushing blood out. Think of it as the maximum force of water pushing through a hose when the tap is fully open. This number reflects the workload on your heart and the strain on your arteries during a heartbeat.
- Diastolic Pressure (the bottom number): This measures the pressure in your arteries when your heart is at rest between beats. Using the hose analogy, this is the residual pressure remaining in the hose when the tap is turned off. It indicates the baseline resistance of your blood vessels.
For decades, diastolic pressure was considered the more critical indicator.
However, extensive research, particularly from large-scale studies like the Framingham Heart Study, has shown that for individuals over 50, systolic pressure is a much more powerful predictor of cardiovascular disease.
Nonetheless, both numbers are crucial for a complete assessment of your cardiovascular risk.
What Is Considered High Blood Pressure?
The definitions for blood pressure categories have evolved. In 2017, the American Heart Association (AHA) and the American College of Cardiology (ACC) updated their guidelines, lowering the threshold for a hypertension diagnosis.
This change was made not to label more people as sick, but to encourage earlier intervention with lifestyle changes to prevent the progression to more severe disease.
The following table, based on the current AHA/ACC guidelines, is the gold standard for classifying blood pressure in adults.
| Blood Pressure Category | Systolic (mm Hg) | Diastolic (mm Hg) | What It Means & Recommended Action | |
|---|---|---|---|---|
| Normal | Less than 120 | and | Less than 80 | Your blood pressure is in the ideal range. Maintain a healthy lifestyle and have it rechecked as your doctor advises. |
| Elevated | 120 – 129 | and | Less than 80 | You are at an increased risk of developing high blood pressure. Lifestyle changes are strongly recommended to prevent progression. |
| Hypertension: Stage 1 | 130 – 139 | or | 80 – 89 | A doctor will likely recommend lifestyle changes and may consider medication based on your overall risk of atherosclerotic cardiovascular disease (ASCVD), such as a heart attack or stroke. |
| Hypertension: Stage 2 | 140 or higher | or | 90 or higher | A doctor will likely prescribe a combination of blood pressure medications and aggressive lifestyle changes. |
| Hypertensive Crisis | Higher than 180 | and/or | Higher than 120 | This is a medical emergency. Seek immediate medical attention. If you experience symptoms like chest pain, shortness of breath, or vision changes, call 911. |
The key takeaway from these guidelines is the emphasis on early detection and action.
The “Elevated” category serves as a crucial warning sign, offering a window of opportunity to make meaningful changes before the condition progresses to full-blown hypertension, where the risk of long-term damage significantly increases.
The Symptoms Deception: Why You Usually Feel Nothing (Until It’s an Emergency)
This section directly confronts the central paradox of high blood pressure: its silence.
Understanding why symptoms are absent is fundamental to appreciating the danger and the absolute necessity of regular monitoring.
Why Is Chronic High Blood Pressure Asymptomatic?
The human body is a master of adaptation. When blood pressure rises, it typically does so very gradually over many years, even decades.
This slow, insidious increase allows the body’s systems, including the blood vessels and heart, to acclimate to the higher pressure.
There is no sudden change to trigger alarm bells like pain or discomfort. The body simply adjusts to a new, more dangerous “normal”.
This leads to the debunking of several persistent myths. Many people believe they can “feel” their blood pressure rising.
However, major health organizations are clear on this point:
“High blood pressure has no warning signs or symptoms, and many people do not know they have it… Myths about high blood pressure are also common. The truth is: High blood pressure is a ‘silent killer’. Most people with high blood pressure have no signs or symptoms”. – Centers for Disease Control and Prevention (CDC)
Commonly cited “symptoms” are generally not reliable indicators of chronic hypertension:
- Headaches: While a sudden, severe headache can be a sign of a hypertensive crisis (more on this below), routine headaches are not caused by chronic high blood pressure. In fact, some studies suggest people with hypertension may have fewer headaches.
- Nosebleeds: These are most often caused by dry air, irritation, or allergies. They are not a sign of high blood pressure unless the pressure is dangerously high, in the range of a hypertensive crisis.
- Dizziness or Lightheadedness: These feelings can have many causes, including dehydration, inner ear issues, or even some blood pressure medications themselves. They are not a direct symptom of the underlying high blood pressure.
The most critical lesson here is that the absence of symptoms does not mean the absence of damage.
While you feel perfectly fine, the relentless, elevated pressure is silently wearing away at the delicate lining of your arteries, overworking your heart muscle, and straining the filtering units in your kidneys.
This damage is cumulative and sets the stage for a future catastrophic event.
When Does High Blood Pressure Cause Symptoms? Understanding Hypertensive Crisis
The one exception to the “no symptoms” rule is a hypertensive crisis.
This is a medical emergency defined by a blood pressure reading that skyrockets to 180/120 mm Hg or higher.
At this extreme level, the pressure is so great that it can rapidly cause organ damage, and the body can no longer compensate silently.
This is when clear, acute, and frightening symptoms can appear. It’s vital to distinguish between two types of hypertensive crisis:
- Hypertensive Urgency: Your blood pressure is 180/120 mm Hg or higher, but you have no associated symptoms of organ damage.
- Hypertensive Emergency: Your blood pressure is 180/120 mm Hg or higher, AND you are experiencing symptoms that suggest organ damage is occurring.
Emergency Action Plan
If you measure your blood pressure and it is 180/120 mm Hg or higher, follow these steps from the American Heart Association:
- If you are NOT experiencing symptoms: Wait five minutes and test it again. If the reading is still at or above this level, contact your doctor immediately. A change in medication may be needed. Do not try to handle it on your own.
- If you ARE experiencing any of the symptoms below: Do not wait. Call 9-1-1 immediately. This is a life-threatening emergency.
The following are potential symptoms of a hypertensive emergency, indicating that the extreme pressure is damaging vital organs like the brain, heart, or kidneys:
- Severe headache, often described as a “thunderclap” headache, different from any you’ve had before.
- Shortness of breath or difficulty breathing.
- Severe chest pain, which could signal a heart attack.
- Nosebleeds (in the context of these extremely high numbers).
- Sudden vision changes, such as blurred vision, double vision, or loss of vision.
- Numbness, weakness, or tingling, especially on one side of the body (a sign of stroke).
- Confusion, severe anxiety, or difficulty speaking.
- Seizures.
These symptoms are not subtle. They are the body’s final, desperate alarm system. Relying on them to appear is a gamble no one should take. The only winning strategy is regular monitoring.
Are You at Risk? Unpacking the Causes of Hypertension
Understanding the factors that contribute to high blood pressure is the first step toward prevention and control.
Hypertension is broadly divided into two types, based on its cause.
What Causes High Blood Pressure?
- Primary (Essential) Hypertension: This is the most common form, accounting for 90-95% of all cases. For people with primary hypertension, there is no single, identifiable cause. Instead, it is understood to develop gradually over many years as a result of a complex interplay between genetics, environment, and lifestyle factors.
- Secondary Hypertension: This accounts for the remaining 5-10% of cases. In secondary hypertension, the high blood pressure is a direct result of an underlying, identifiable medical condition. When the root cause is treated, the blood pressure often improves or returns to normal. Common causes include:
- Obstructive sleep apnea
- Kidney disease
- Adrenal gland tumors
- Thyroid problems
- Certain congenital defects in blood vessels
- Certain medications, including some decongestants, birth control pills, and over-the-counter pain relievers.
For the vast majority of people, the focus must be on managing the web of risk factors associated with primary hypertension.
These can be separated into two categories: those you can change, and those you cannot.
Which Risk Factors Can You Control?
These lifestyle factors are the cornerstone of hypertension prevention and management.
They represent your greatest power to influence your cardiovascular health.
Unhealthy Diet
The modern diet is perhaps the single greatest contributor to rising rates of hypertension.
The key culprits are high sodium intake, which causes the body to retain fluid and increases blood volume, and low potassium intake, which disrupts the body’s ability to excrete sodium.
A diet high in processed foods, saturated fats, and sugar also contributes to inflammation and obesity, both of which drive up blood pressure.
Physical Inactivity
A sedentary lifestyle forces the heart to work harder with every beat.
Regular physical activity strengthens the heart muscle, allowing it to pump blood more efficiently.
A stronger heart can pump the same amount of blood with less effort, which decreases the force on your arteries and lowers your blood pressure.
Obesity
Carrying excess weight significantly increases the risk of hypertension.
More body mass requires more blood to supply oxygen and nutrients to the tissues.
This increased blood volume circulates through your arteries, raising the pressure on their walls.
Obesity is also linked to other risk factors like sleep apnea and insulin resistance.
Excessive Alcohol Consumption
Drinking too much alcohol can raise blood pressure to unhealthy levels.
Having more than three drinks in one sitting temporarily increases your blood pressure, but repeated binge drinking can lead to long-term increases.
Alcohol can also contribute to weight gain and can interfere with the effectiveness of blood pressure medications.
Smoking and Tobacco Use
The impact of tobacco is twofold and immediate.
The nicotine in tobacco products temporarily raises your blood pressure and heart rate each time you use it.
More importantly, the chemicals in tobacco smoke can damage the lining of your artery walls, causing them to narrow and harden (atherosclerosis), which permanently increases blood pressure.
Chronic Stress
While acute stress causes temporary spikes in blood pressure, the role of chronic stress is more complex.
Persistent stress can lead to poor coping behaviors—such as overeating, smoking, or drinking alcohol—that are known risk factors for hypertension.
Furthermore, chronic activation of the body’s stress hormones may have a direct, long-term effect on the cardiovascular system.
Which Risk Factors Are Beyond Your Control?
While you cannot change these factors, knowing about them is crucial for understanding your personal risk profile and underscores the importance of managing the factors you can control.
Family History (Genetics)
High blood pressure has a strong genetic component and tends to run in families.
If your parents or other close blood relatives have hypertension, you are more likely to develop it.
This genetic predisposition makes a healthy lifestyle even more critical for you.
Age
The risk of high blood pressure increases as you get older.
This is a natural consequence of the aging process, as arteries gradually lose some of their elasticity and become stiffer.
This stiffness means they are less able to expand to accommodate blood flow, leading to higher pressure.
Race and Ethnicity
Certain racial and ethnic groups experience a higher burden of hypertension.
In the United States, it is particularly prevalent and often more severe in non-Hispanic Black adults. It also tends to develop earlier in life in this population.
The reasons are complex and thought to involve a combination of genetic and environmental factors.
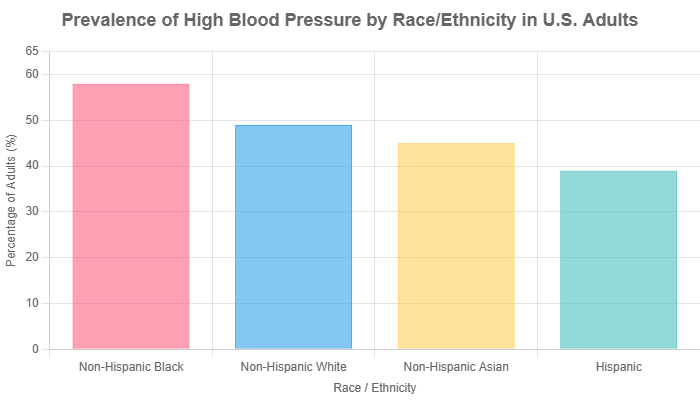
As the data from the CDC clearly illustrates, significant disparities exist. This highlights the need for targeted public health initiatives and increased awareness within higher-risk communities.
Chronic Conditions
Other chronic diseases can increase your risk of developing high blood pressure or make it harder to control.
Conditions like diabetes and kidney disease are closely linked with hypertension, often creating a vicious cycle where each condition worsens the other.
The Long-Term Damage: What Happens if High Blood Pressure Goes Unchecked?
The “silent” nature of hypertension belies the violent storm it wages inside the body.
Over years, the relentless force of high-pressure blood flow acts like a slow-motion wrecking ball, causing systemic damage to your most vital organs.
Understanding these consequences is the ultimate motivation for taking control of your blood pressure.
How Does High Blood Pressure Damage Your Body?
Damage to Arteries: The Foundation of Disease
Your arteries are designed to be strong yet flexible, expanding and contracting with each heartbeat.
High blood pressure disrupts this delicate balance in two main ways:
- Atherosclerosis: The constant high pressure injures the delicate inner lining (endothelium) of your arteries. This damage creates sites where LDL (“bad”) cholesterol and other cellular debris can accumulate, forming plaques. This process, known as atherosclerosis, narrows and hardens the arteries, restricting blood flow and further increasing pressure.
- Aneurysm: In some areas, the constant pressure can cause a section of an artery wall to weaken and bulge outwards, forming an aneurysm. If an aneurysm ruptures, it can cause life-threatening internal bleeding. Aneurysms can occur anywhere, but are most dangerous in the brain or the body’s main artery, the aorta.
Damage to the Heart: An Overworked Pump
Your heart bears the direct brunt of high blood pressure.
To push blood against the higher resistance in your arteries, the heart muscle must work harder.
Just like any muscle that is overworked, it adapts by getting bigger.
- Left Ventricular Hypertrophy (LVH): The heart’s main pumping chamber, the left ventricle, thickens and enlarges. While a bigger muscle might sound stronger, an enlarged heart is actually less efficient and stiffer, impairing its ability to fill with and pump blood effectively.
- Heart Failure: Over time, the strain of pumping against high pressure can cause the heart muscle to weaken and fail. The heart can no longer pump enough blood to meet the body’s needs, leading to symptoms like shortness of breath, fatigue, and swelling in the legs and abdomen.
- Coronary Artery Disease: The same atherosclerotic process that damages other arteries also affects the coronary arteries, which supply blood to the heart muscle itself. When these become narrowed or blocked, it can lead to angina (chest pain) or a full-blown heart attack (myocardial infarction).
Damage to the Brain: A Stroke and Dementia Risk
The brain is exquisitely sensitive to disruptions in blood flow. High blood pressure is the single most important risk factor for stroke.
- Ischemic Stroke: This is the most common type of stroke. It occurs when atherosclerosis or a blood clot completely blocks an artery leading to the brain, depriving brain cells of oxygen and causing them to die.
- Hemorrhagic Stroke: This occurs when an artery in the brain bursts, often due to a long-standing aneurysm caused by high blood pressure. The resulting bleeding puts pressure on brain tissue and damages it.
- Vascular Dementia: Chronic high blood pressure can cause widespread, small-scale damage to the blood vessels deep within the brain. Over time, this “silent” damage impairs blood flow and can lead to problems with thinking, memory, and reasoning, a condition known as vascular dementia.
Damage to the Kidneys: A Failing Filter
Your kidneys are dense networks of tiny blood vessels that filter waste from your blood.
This filtration system is highly dependent on healthy, stable blood pressure.
- Nephrosclerosis: High blood pressure damages the arteries leading to the kidneys and the tiny filtering units (glomeruli) within them. This leads to scarring of the kidney tissue, a condition called nephrosclerosis.
- Kidney Failure: As more and more filtering units are destroyed, the kidneys lose their ability to remove waste and excess fluid from the body. This can eventually progress to end-stage renal disease, requiring dialysis or a kidney transplant to survive.
Damage to the Eyes: A Window to the Vessels
The tiny, delicate blood vessels in the retina at the back of your eye are a visible indicator of the health of blood vessels throughout your body.
An eye doctor can often see the damage from high blood pressure during a routine exam.
- Hypertensive Retinopathy: High blood pressure can damage these vessels, causing them to leak fluid or bleed. This can lead to blurred vision, and in severe cases, complete vision loss.
- Optic Neuropathy: Blocked blood flow can also damage the optic nerve, which transmits visual information to the brain, resulting in permanent vision loss.
Taking Control: How Is High Blood Pressure Diagnosed and Managed?
Given its silent nature, the diagnosis of hypertension cannot rely on symptoms.
It depends entirely on accurate measurement.
The process is straightforward but requires care to avoid misdiagnosis.
How Do Doctors Diagnose High Blood Pressure?
A diagnosis of hypertension is almost never made from a single high reading.
Blood pressure fluctuates naturally throughout the day and can be influenced by stress, activity, and even the time of day.
A proper diagnosis involves a systematic approach:
- Initial Screening: A high reading during a routine check-up is a red flag that warrants further investigation.
- Multiple Readings: Your doctor will want to confirm the high reading with several measurements taken on at least two or three separate occasions. Proper technique is crucial: you should be seated quietly for at least five minutes with your back supported, feet flat on the floor, and your arm supported at heart level.
- Addressing “White-Coat Hypertension”: Many people experience anxiety in a medical setting, which can cause their blood pressure to be temporarily higher than it is in their daily life. This is known as “white-coat hypertension”. To rule this out and get a more accurate picture of your true blood pressure, your doctor may recommend:
- Home Blood Pressure Monitoring: Using a validated, automated device at home allows you to take readings in a relaxed environment. Your doctor will ask you to keep a log of readings taken at specific times over several days.
- Ambulatory Blood Pressure Monitoring (ABPM): This is considered the gold standard. You wear a small, portable device with a cuff that automatically measures and records your blood pressure at regular intervals over a 24-hour period, including while you sleep. This provides a comprehensive view of your blood pressure patterns.
Once a diagnosis of hypertension is confirmed, your doctor will also conduct other tests—such as blood work, a urine test, and an electrocardiogram (ECG)—to check for underlying causes (secondary hypertension) and to see if any organ damage has already occurred.
What Is the First Step in Managing High Blood Pressure?
The answer is universal and unequivocal: lifestyle modification is the foundation of treatment for every single person with elevated blood pressure or hypertension.
For individuals in the “Elevated” or “Stage 1 Hypertension” categories with a low overall cardiovascular risk, intensive lifestyle changes may be the only treatment needed to bring their blood pressure back into a healthy range.
For those with more severe hypertension or higher risk, lifestyle changes are still essential.
They enhance the effectiveness of medications, often allowing for lower doses, and provide broad health benefits that go far beyond blood pressure control.
The next section provides a detailed action plan for implementing these critical lifestyle strategies.
Your Action Plan: Proven Strategies to Lower Blood Pressure
Managing high blood pressure is a lifelong commitment, but the tools to do so are powerful and accessible.
The approach combines natural, lifestyle-based strategies with medical therapies when necessary.
This section provides a comprehensive, evidence-based guide to taking control.
How Can I Lower My Blood Pressure Naturally?
These lifestyle interventions are the most powerful tools at your disposal.
They are not just suggestions, they are prescriptions for a healthier cardiovascular system.
Adopt the DASH Eating Plan
The DASH (Dietary Approaches to Stop Hypertension) diet is not a fad, it’s a scientifically proven eating plan developed by the National Heart, Lung, and Blood Institute (NHLBI) specifically to lower blood pressure.
It can lower blood pressure as much as some medications, often within just a few weeks.
The core principles of the DASH diet are:
- Focus on: Fruits, vegetables, and whole grains.
- Include: Fat-free or low-fat dairy products, fish, poultry, beans, nuts, and vegetable oils.
- Limit: Foods high in saturated fat (like fatty meats and full-fat dairy), sugar-sweetened beverages, and sweets.
- Key Nutrients: It is naturally rich in potassium, magnesium, calcium, and fiber, and low in sodium—a combination that is ideal for blood pressure control.
Reduce Sodium Intake Drastically
While DASH is a broad framework, sodium reduction deserves special attention.
The average American consumes over 3.400 mg of sodium per day, far more than the body needs.
The AHA recommends an ideal limit of no more than 1.500 mg per day for most adults, especially those with high blood pressure.
Practical tips for cutting sodium:
- Read Labels: Sodium hides in countless processed foods. Look for “low sodium” or “no salt added” versions.
- Avoid the “Salty Six”: The AHA identifies bread and rolls, pizza, sandwiches, cold cuts and cured meats, soup, and burritos/tacos as major sources of sodium in the American diet.
- Cook at Home: This gives you complete control over how much salt goes into your food. Use herbs, spices, citrus, and vinegar to add flavor instead of salt.
Get Regular Physical Activity
Exercise is medicine for your heart. The standard recommendation is for at least 150 minutes of moderate-intensity aerobic exercise per week.
This can be broken down into 30 minutes, five days a week.
- Moderate-intensity activities include: Brisk walking, cycling (on flat ground), swimming, dancing, or gardening.
- Consistency is key: The blood pressure-lowering effects of exercise last only as long as you continue to be active. Make it a non-negotiable part of your routine.
Maintain a Healthy Weight
Blood pressure often rises as weight increases. The good news is that even a small amount of weight loss can have a major impact.
Losing as little as 5 to 10 pounds can help lower your blood pressure and improve the effectiveness of blood pressure medications.
Limit Alcohol and Quit Tobacco
If you drink alcohol, do so in moderation. That means up to one drink per day for women and up to two drinks per day for men.
If you don’t drink, don’t start. If you use tobacco, quitting is the single most important step you can take to protect your cardiovascular health.
Your doctor can provide resources to help you quit successfully.
What Medications Are Used to Treat High Blood Pressure?
When lifestyle changes alone are not enough to reach your blood pressure goal, or if you have Stage 2 hypertension or other significant risk factors, your doctor will prescribe medication.
There are many different classes of blood pressure drugs, and they work in different ways.
Often, a combination of two or more drugs is more effective than a single one.
Medical Advice Disclaimer: The following is for informational purposes only. Never start, stop, or change a medication without consulting your doctor. They will choose the best medication(s) for you based on your health profile, other medical conditions, and potential side effects.
The main classes of medication include:
- Diuretics (“water pills”): These drugs, such as hydrochlorothiazide or chlorthalidone, help your kidneys eliminate excess sodium and water from your body, reducing blood volume and pressure. They are often one of the first-line choices.
- ACE (Angiotensin-Converting Enzyme) Inhibitors: Drugs like lisinopril and enalapril help relax your blood vessels by blocking the formation of a natural chemical (angiotensin II) that narrows them.
- ARBs (Angiotensin II Receptor Blockers): These drugs, such as losartan and valsartan, also help relax blood vessels by blocking the action (rather than the formation) of angiotensin II. They are often used if ACE inhibitors cause side effects like a dry cough.
- Calcium Channel Blockers: Medications like amlodipine and diltiazem help relax the muscle cells of your blood vessels. Some can also slow your heart rate.
- Beta-Blockers: Drugs like metoprolol and atenolol work by making your heart beat slower and with less force, which lowers blood pressure. They are no longer a first-line choice for hypertension alone but are used if you also have other conditions like coronary artery disease or certain arrhythmias.
Finding the right medication or combination of medications can sometimes take trial and error.
Open communication with your doctor is essential to find a regimen that is both effective and has minimal side effects for you.
Frequently Asked Questions (FAQ)
Q1: Can high blood pressure be cured?
A: High blood pressure can be effectively managed with lifestyle changes and medication, but it is a lifelong condition that typically cannot be “cured”. Consistent management is key to preventing complications and maintaining a healthy life.
Q2: Can I feel when my blood pressure is high?
A: No, most people cannot feel chronic high blood pressure. Relying on feelings like headaches or dizziness is dangerous and unreliable. The only way to know your numbers is to have your blood pressure measured regularly.
Q3: Does stress cause long-term high blood pressure?
A: While acute stress temporarily raises blood pressure, the link to chronic hypertension is complex. Chronic stress often leads to unhealthy habits (poor diet, alcohol use, lack of sleep) that are proven contributors to long-term high blood pressure.
Q4: How quickly can I lower my blood pressure?
A: Consistent lifestyle changes, like the DASH diet, can start to lower blood pressure within a few weeks. However, achieving significant, stable improvement takes months of dedication. Medications can work more quickly, often showing effects within days or weeks.
Q5: Is the top or bottom blood pressure number more important?
A: Both are important for assessing risk. Historically, more emphasis was placed on the diastolic (bottom) number, but extensive research now shows that for people over 50, the systolic (top) number is often a better predictor of stroke and heart disease risk.
Q6: Can I stop taking my blood pressure medication if I feel better?
A: Absolutely not. This is a critical and dangerous mistake. You feel better *because* the medication is working to control your pressure. Stopping it abruptly can cause your blood pressure to rebound to dangerously high levels, increasing your risk of a stroke or heart attack.
Q7: Is red wine good for high blood pressure?
A: This is largely a myth. While some observational studies suggest moderate red wine consumption may be associated with some heart benefits, excessive alcohol of any kind raises blood pressure. The American Heart Association does not recommend that anyone start drinking alcohol for potential health benefits.
Q8: What is a good home blood pressure monitor?
A: Choose an automatic, cuff-style monitor that goes on your upper arm (not the wrist or finger, which are less accurate). Look for a device that has been clinically validated for accuracy. You can consult validatebp.org or ask your doctor or pharmacist for a recommendation.
Conclusion
We have journeyed through the silent, complex world of high blood pressure.
The most critical takeaways are simple yet profound: high blood pressure is a common, serious, and fundamentally silent condition.
Its danger lies not in the symptoms it causes, but in the devastating damage it inflicts while causing no symptoms at all.
The headaches, dizziness, and nosebleeds of popular myth are unreliable distractions, the true signs of a problem only appear during a life-threatening emergency.
Therefore, knowing your numbers is not just a good idea—it is the first and most essential act of self-defense against this silent killer.
Regular monitoring is the only way to unmask the threat before it’s too late. But this knowledge should not inspire fear, it should inspire action.
The management of hypertension is a powerful example of how proactive self-care can profoundly alter your health trajectory.
The evidence is clear: lifestyle changes are remarkably effective, and modern medical treatments can safely and successfully control blood pressure in nearly everyone.
Framing this not as a burden, but as an empowering act of taking control, is the key to long-term success.
Don’t wait for a silent killer to make itself known through a catastrophic event. Your future self will thank you for the actions you take today.
Schedule an appointment with your doctor to get your blood pressure checked. Discuss your personal risk factors, understand your numbers, and partner with your healthcare provider to create a plan that will protect your heart, brain, and body for years to come.
Do you have experience managing high blood pressure? Share your tips or questions in the comments below to help our community learn and grow together.

