Hemorrhoids are swollen veins in your anus and lower rectum that can cause discomfort, itching, and rectal bleeding.
This condition, also known as piles, is incredibly common, affecting about 1 in 20 Americans and roughly half of all adults by the age of 50, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Despite their prevalence, many people feel embarrassed to discuss them, leading to delayed diagnosis and unnecessary suffering.
This comprehensive guide is designed to break the silence, providing you with authoritative, in-depth information on everything from the subtle signs of internal hemorrhoids to the most advanced treatments for severe cases.
By understanding the causes, symptoms, and full spectrum of management options, you can take control of your health and find lasting relief.
In This Article
What Exactly Are Hemorrhoids? (And What They’re Not)
While many people think of hemorrhoids as a disease, they are actually a normal part of the human anatomy.
In their normal state, they are pillow-like clusters of veins, smooth muscle, and connective tissue that lie just beneath the mucous membranes lining the lower rectum and anus.
These “anal cushions” play a role in stool control and protect the anal sphincter.
The condition most of us call hemorrhoids, or piles, develops when these veins become swollen, inflamed, and distended—similar to varicose veins in the legs. This swelling occurs due to increased pressure in the lower rectum, which interferes with blood flow and causes blood to pool in the vessels.
The Anatomy of the Anal Canal: Normal vs. Symptomatic Hemorrhoids
To understand hemorrhoidal disease, it’s crucial to distinguish between the normal anatomical structures and the symptomatic condition.
The anal canal is the final section of the large intestine, and it’s rich with blood vessels.
The dentate line (or pectinate line) is an important landmark within the anal canal that separates the upper two-thirds from the lower third.
This line is significant because it determines the type of hemorrhoid and the symptoms you might experience, as the nerves above and below it are different.
- Above the Dentate Line: This area is lined with the same type of cells as the rest of the intestines and is supplied by visceral nerves. These nerves don’t sense pain, which is why internal hemorrhoids are typically painless.
- Below the Dentate Line: This area is covered by skin-like cells and is rich in somatic nerves, which are highly sensitive to pain, touch, and temperature. This is why external hemorrhoids can be very painful.
When these vascular cushions become enlarged and symptomatic, they are classified as hemorrhoidal disease.
Internal vs. External Hemorrhoids: Key Differences
The location relative to the dentate line determines whether a hemorrhoid is internal or external. Many people have both types simultaneously.

Illustration showing the location of internal (inside the rectum) and external hemorrhoids (under the skin around the anus).
Internal Hemorrhoids
Internal hemorrhoids form in the lining of the anus and lower rectum, above the dentate line. You usually can’t see or feel them, and they rarely cause discomfort because of the lack of pain-sensing nerves in that area.
The primary sign is painless, bright red bleeding during or after a bowel movement. They can also prolapse, meaning they stretch and bulge outside the anal opening.
External Hemorrhoids
External hemorrhoids develop under the skin around the anus, below the dentate line. Because this area is rich in pain-sensing nerves, external hemorrhoids are often associated with more noticeable symptoms. These can include pain, itching, irritation, and swelling around the anus.
If a blood clot forms within an external hemorrhoid, it becomes a thrombosed hemorrhoid, which can be suddenly and severely painful.
Debunking Common Myths About Hemorrhoids
Misinformation about hemorrhoids is widespread, often leading to fear and delayed treatment. Let’s separate fact from fiction.
| Myth | Fact |
|---|---|
| Only older people get hemorrhoids. | While the risk increases with age as supporting tissues weaken, hemorrhoids can affect people of any age. Factors like pregnancy, chronic constipation, and lifestyle can cause them in younger adults and even teenagers. |
| Spicy foods cause hemorrhoids. | Spicy foods are not the cause. However, for some individuals, they can irritate the digestive tract and may worsen the symptoms of existing hemorrhoids, but they are not a root cause. |
| Hemorrhoids are a sign of cancer. | Hemorrhoids are not cancerous and do not cause cancer. However, their main symptom—rectal bleeding—is also a key symptom of colorectal cancer. For this reason, it is crucial to have any rectal bleeding evaluated by a doctor to rule out more serious conditions. |
| You can get hemorrhoids from sitting on cold surfaces. | There is no scientific evidence to support this claim. The primary causes are related to increased pressure on the rectal veins, not temperature. |
| Poor hygiene causes hemorrhoids. | Hygiene is not the cause. They are a vascular issue caused by internal pressure. In fact, overly aggressive wiping or cleaning can irritate existing external hemorrhoids and worsen symptoms. |
| All hemorrhoids require surgery. | This is false. The vast majority of hemorrhoids can be managed effectively with lifestyle changes, dietary adjustments, and at-home remedies. Surgery is reserved for severe, persistent cases that do not respond to less invasive treatments. |
What Are the Symptoms of Hemorrhoids?
The symptoms depend largely on the type—whether they are internal or external. It’s possible to have both types at the same time, leading to a mix of symptoms.
Symptoms of Internal Hemorrhoids
Because they are located inside the rectum where there are no pain receptors, internal hemorrhoids may go unnoticed unless they cause bleeding or prolapse.
- Painless Rectal Bleeding: This is the most common sign. You might notice small amounts of bright red blood on your toilet paper after wiping, in the toilet bowl, or as streaks on the surface of your stool. Because the blood is fresh, it is typically bright red, not dark.
- Prolapse: Straining during a bowel movement can push an internal hemorrhoid through the anal opening. This is known as a prolapsed or protruding hemorrhoid. It may feel like a soft, grape-like lump. A prolapsed hemorrhoid can be painful and irritating, especially when wiping. It may retract back inside on its own or may need to be gently pushed back in.
- Mucus Discharge and Itching: A prolapsed hemorrhoid can bring mucus with it, which can irritate the sensitive skin around the anus, causing itching (pruritus ani) and a feeling of dampness.
The Grading System for Internal Hemorrhoids
Clinicians often use a grading system, known as the Goligher classification, to describe the severity of internal hemorrhoids based on the degree of prolapse. This helps guide treatment decisions.
| Grade | Description | Common Symptoms |
|---|---|---|
| Grade I | Hemorrhoids are present but do not prolapse (bulge out of the anus). They remain inside the rectum. | Painless bleeding is the most common symptom. They are only visible via anoscopy. |
| Grade II | Hemorrhoids prolapse during a bowel movement or straining but retract spontaneously (go back in on their own). | Bleeding and a feeling of fullness or a lump that disappears after defecation. |
| Grade III | Hemorrhoids prolapse and must be manually pushed back into the anus. | Bleeding, discomfort, itching, and a noticeable lump that requires manual reduction. |
| Grade IV | Hemorrhoids are permanently prolapsed and cannot be manually pushed back in. They remain outside the anus. | Constant discomfort, pain, soiling, itching, and risk of strangulation (see complications). |
Symptoms of External Hemorrhoids
Located under the sensitive skin around the anus, external hemorrhoids are more likely to cause noticeable discomfort.
- Pain or Discomfort: This can range from mild soreness to significant pain, especially when sitting or during bowel movements.
- Itching or Irritation: The anal area may become itchy and irritated. This can be made worse by moisture or difficulty cleaning the area properly.
- Swelling or Lumps: You may feel one or more soft or firm lumps around the anal opening.
- Bleeding: While less common than with internal hemorrhoids, external ones can also bleed, especially if irritated by wiping.
What is a Thrombosed Hemorrhoid?
A thrombosed hemorrhoid is a complication that occurs when a blood clot (thrombus) forms inside an external hemorrhoid.
This is not dangerous, but it can be extremely painful. The pressure from the clot causes a rapid onset of symptoms:
- Severe, Acute Pain: The pain is often sudden and intense, making it difficult to sit, walk, or have a bowel movement.
- A Hard, Painful Lump: A firm, tender lump can be felt at the anal edge. It may appear bluish or purple due to the underlying clot.
- Swelling and Inflammation: The area around the clot becomes very swollen and inflamed.
The body will usually reabsorb the clot over several weeks, and the pain will subside. However, the pain is often most severe in the first 48-72 hours. A doctor can perform a minor procedure to remove the clot and provide immediate relief if you are seen within this window.
When Should You See a Doctor for Hemorrhoids?
While many cases of hemorrhoids can be managed at home, certain symptoms warrant a professional medical evaluation.
It’s important not to self-diagnose, as other more serious conditions can have similar symptoms.
Recognizing Red Flag Symptoms
According to the Mayo Clinic, you should talk with a healthcare professional if your hemorrhoids don’t improve after a week of home care or if you experience any of the following:
- Rectal bleeding for the first time, or an increase in the amount of bleeding.
- Changes in your bowel habits, such as a change in stool color (e.g., black, tarry stools) or consistency that lasts for more than a few days.
- Severe pain that is not relieved by home treatments.
- A lump that is hard and very painful, which could indicate a thrombosed hemorrhoid.
- Unexplained weight loss, fever, or abdominal pain accompanying your rectal symptoms.
Seek emergency care immediately if you experience large amounts of rectal bleeding, lightheadedness, dizziness, or faintness. This could be a sign of significant blood loss.
Why You Shouldn’t Self-Diagnose Rectal Bleeding
The most critical reason to see a doctor for rectal bleeding is to rule out other, more serious conditions.
While hemorrhoids are the most common cause of bright red blood after a bowel movement, they are not the only cause. Other potential causes include:
- Anal Fissures: Small tears in the lining of the anus.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis.
- Diverticular Disease: Small pouches in the colon wall that can bleed.
- Colorectal Polyps or Cancer: Rectal bleeding is a key warning sign of colorectal cancer.
Don’t assume your bleeding is “just hemorrhoids“, especially if you are over 40 or have other risk factors for colorectal cancer.
A proper diagnosis is the only way to ensure you receive the right treatment.
Preparing for Your Doctor’s Appointment
To make the most of your appointment, it helps to be prepared. Consider the following:
- Write down your symptoms: Note when they started, how often they occur, and what makes them better or worse. Be specific about bleeding (color, amount, when it occurs).
- List your medications: Include all prescription drugs, over-the-counter medicines, and supplements you take.
- Note your personal and family medical history: Mention any history of digestive diseases, IBD, or colorectal cancer.
- Prepare questions to ask: Examples include “What is the likely cause of my symptoms?”, “What tests do I need?”, “What treatment approach do you recommend?”, and “What lifestyle changes can I make to prevent this from happening again?”.
What Causes Hemorrhoids and Who Is at Risk?
Hemorrhoids develop when there is excessive pressure on the veins in the pelvic and rectal area. This pressure causes the veins to swell and bulge.
While the exact pathophysiology is complex, several key factors are known to contribute to their development.
Primary Causes: The Science of Increased Pressure
Any activity or condition that increases intra-abdominal pressure can lead to the formation of symptomatic hemorrhoids. The main culprits include:
- Straining During Bowel Movements: This is the most common cause. Pushing hard to pass stool increases pressure in the anal canal, forcing blood into the anal cushions and preventing it from flowing out.
- Chronic Constipation or Diarrhea: Constipation leads to hard stools and straining. Chronic diarrhea can also be irritating and increase pressure in the area.
- Prolonged Sitting, Especially on the Toilet: Sitting for long periods, particularly on the toilet, allows blood to pool in the hemorrhoidal veins, increasing pressure and encouraging them to swell. This position causes the anal muscles to relax, removing support from the veins.
- Pregnancy: The enlarging uterus puts direct pressure on the rectal veins. Hormonal changes can also cause veins to relax and swell. The strain of childbirth is another major contributor.
- Obesity: Excess body weight, especially around the abdomen, increases pressure on the pelvic veins.
- Heavy Lifting: Regularly lifting heavy objects, often while holding your breath, can dramatically increase intra-abdominal pressure.
Major Risk Factors
While anyone can develop hemorrhoids, certain factors increase your likelihood. Many of these are linked to the causes listed above.
- Age: The risk of hemorrhoids increases as you get older. By age 50, about half of the population has experienced symptoms. This is because the connective tissues that support the veins in the rectum and anus can weaken and stretch over time.
- Diet: A low-fiber diet is a primary contributor to constipation, which in turn leads to straining and hemorrhoids.
- Lifestyle: A sedentary lifestyle can contribute to both obesity and poor bowel function, increasing your risk.
- Anal Intercourse: This activity can directly cause or exacerbate existing hemorrhoids.
Are Hemorrhoids Hereditary?
While there isn’t a specific “hemorrhoid gene”, there does appear to be a hereditary component. Some people may inherit weaker vein walls or connective tissues, making them more susceptible to developing hemorrhoids and varicose veins in general.
If your parents had hemorrhoids, you may be more likely to develop them as well.
However, lifestyle factors play a much more significant role, and even with a genetic predisposition, you can take steps to prevent them.
How Are Hemorrhoids Diagnosed?
A doctor can typically diagnose hemorrhoids based on a medical history and a physical examination.
The process is usually straightforward and helps rule out other, more serious conditions.
Medical History and Physical Examination
Your doctor will start by asking about your symptoms, such as bleeding, pain, itching, and any lumps you may have felt.
They will also ask about your bowel habits, diet, and family history.
The physical exam usually includes:
- Visual Inspection: The doctor will examine the area around your anus to look for external hemorrhoids, skin tags, fissures, or other abnormalities. Prolapsed internal hemorrhoids may also be visible.
- Digital Rectal Exam (DRE): The doctor will insert a gloved, lubricated finger into your rectum. This allows them to feel for any lumps or abnormalities and check the tone of the sphincter muscle. Internal hemorrhoids are often too soft to be felt unless they are large or thrombosed. A DRE also helps check for blood in the stool.
Diagnostic Procedures for a Closer Look
If the diagnosis is unclear or if your doctor needs to evaluate internal hemorrhoids more closely, they may use a scope.
These procedures are usually performed in the office and cause minimal discomfort.
- Anoscopy: This is the primary procedure for diagnosing internal hemorrhoids. A short, rigid, hollow tube with a light on the end, called an anoscope, is inserted a few inches into the anus. This provides a clear view of the lower rectum and anal canal, allowing the doctor to see the size and location of internal hemorrhoids.
- Flexible Sigmoidoscopy or Colonoscopy: If you have rectal bleeding, your doctor may recommend a more extensive examination to rule out other causes like polyps or cancer, especially if you are over 40 or have other risk factors. A flexible sigmoidoscopy examines the lower third of the colon, while a colonoscopy examines the entire colon. These procedures are essential for a comprehensive evaluation of the gastrointestinal tract.
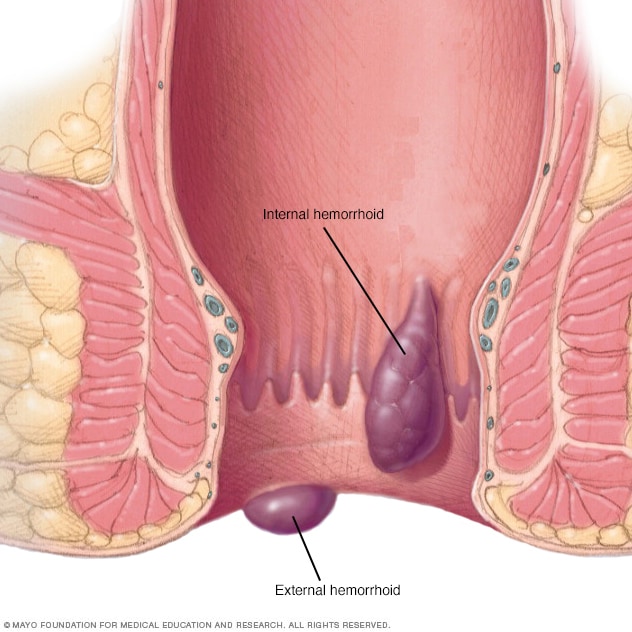
This illustration clearly shows an internal hemorrhoid located within the rectum and an external hemorrhoid under the skin of the anus.
How Can You Get Rid of Hemorrhoids at Home?
Fortunately, most cases of symptomatic hemorrhoids can be effectively managed with simple home treatments and lifestyle adjustments.
The goal of these remedies is to relieve symptoms and prevent flare-ups by promoting soft, easy-to-pass stools.
1. Embrace a High-Fiber Diet
This is the single most important step for treating and preventing hemorrhoids. Fiber softens stool and increases its bulk, which helps you avoid straining.
The NIDDK recommends aiming for 25-30 grams of fiber per day.
- High-Fiber Foods: Incorporate more fruits (berries, pears, apples), vegetables (broccoli, Brussels sprouts, leafy greens), beans, lentils, and whole grains (oatmeal, brown rice, quinoa) into your meals.
- Fiber Supplements: If you struggle to get enough fiber from food, over-the-counter supplements like psyllium (Metamucil), methylcellulose (Citrucel), or wheat dextrin (Benefiber) are highly effective. Start slowly to avoid gas and bloating.
2. Drink Plenty of Fluids
Water is essential for fiber to work properly. It helps draw water into your stool, keeping it soft.
Aim to drink 6 to 8 glasses of water and other clear liquids (like broth or fruit juice) each day. Insufficient fluid intake while on a high-fiber diet can actually worsen constipation.
3. Take Warm (Sitz) Baths
A sitz bath is a warm, shallow bath that cleanses and soothes the perineum. It can provide significant relief from the itching, irritation, and muscle spasms associated with hemorrhoids.
- How to do it: You can sit in a regular bathtub with a few inches of warm (not hot) water, or use a small plastic tub that fits over your toilet seat.
- Frequency: Experts at Harvard Health recommend a 15-20 minute sitz bath two to three times a day, especially after each bowel movement.
- Afterward: Gently pat the area dry with a soft towel. Do not rub. You can also use a hairdryer on a cool setting.
4. Use Over-the-Counter Topical Treatments
Several non-prescription products can help manage the acute symptoms of a hemorrhoid flare-up.
- Soothing Wipes: Medicated pads containing witch hazel (like Tucks) can be soothing and help reduce itching and inflammation without harmful side effects.
- Creams and Ointments: Creams containing hydrocortisone can reduce inflammation and itching, while those with lidocaine can provide temporary pain relief. Use them only for a short period (no more than a week) unless directed by your doctor, as prolonged use of steroids can thin the skin.
- Cold Compresses: Applying an ice pack wrapped in a cloth to the anal area for a few minutes at a time can help reduce swelling and numb the pain, especially for thrombosed hemorrhoids.
5. Practice Good Toilet Habits
How you behave on the toilet can have a huge impact on hemorrhoids.
- Don’t Strain: Avoid straining or holding your breath when trying to pass a stool. This creates immense pressure on the rectal veins. Let things happen naturally.
- Go When You Feel the Urge: Don’t delay a bowel movement. Waiting can cause the stool to become harder and drier, leading to more straining.
- Limit Time on the Toilet: Avoid sitting on the toilet for extended periods (e.g., reading or using your phone). This position encourages blood to pool in the hemorrhoidal veins.
What Medical Treatments Are Available for Hemorrhoids?
When home remedies aren’t enough, or for persistent and severe hemorrhoids (typically Grades II-IV), a number of effective medical procedures are available.
These range from minimally invasive office-based procedures to more extensive surgery.
Minimally Invasive Office-Based Procedures
These procedures are for symptomatic internal hemorrhoids and are typically performed in a doctor’s office without the need for anesthesia.
They are generally quick, with minimal discomfort and a fast recovery.
Rubber Band Ligation (RBL)
This is the most common and effective office treatment for internal hemorrhoids. A small elastic band is placed around the base of the hemorrhoid, cutting off its blood supply.
The hemorrhoid then withers and falls off within a week or two, usually during a bowel movement. The wound heals and creates a scar, which helps hold nearby veins in place.
- Best for: Grades I, II, and III internal hemorrhoids.
- Effectiveness: Success rates are high, often reported between 70-80%. Multiple sessions may be needed to treat all hemorrhoidal columns.
- Side Effects: A feeling of fullness or mild pain is common but usually subsides quickly. Bleeding can occur when the hemorrhoid falls off. Serious complications are rare.
Sclerotherapy
In this procedure, a chemical solution (a sclerosant) is injected directly into the internal hemorrhoid tissue.
This causes a local inflammatory reaction that leads to scarring, which makes the hemorrhoid shrink and retract.
Recent advancements, particularly the use of polidocanol foam, have renewed interest in this technique.
- Best for: Grades I and II internal hemorrhoids, especially for patients on blood thinners where banding may be risky.
- Effectiveness: Effective for controlling bleeding, though recurrence may be slightly higher than with RBL. Studies on polidocanol foam show promising results with high patient satisfaction and low pain. A 2022 study in Tech Coloproctol found polidocanol foam sclerotherapy to be effective and safe even in patients with bleeding disorders.
- Side Effects: Generally very safe with minimal pain. Rare complications can include allergic reactions or, if injected improperly, more serious issues.
Infrared Coagulation (IRC)
This technique uses a device that creates an intense beam of infrared light to generate heat.
The heat is applied to the base of the hemorrhoid, causing scar tissue to form and cutting off the blood supply. The hemorrhoid then shrinks and recedes.
- Best for: Grades I and II internal hemorrhoids.
- Effectiveness: Effective, but may require more sessions than RBL and has a higher recurrence rate.
- Side Effects: Generally painless. Bleeding and mild discomfort can occur.
Surgical Procedures for Severe Hemorrhoids
Surgery is typically reserved for large, symptomatic Grade III and IV internal hemorrhoids, external hemorrhoids that cause significant problems, or when office procedures have failed.
Hemorrhoidectomy
This is the traditional surgical removal of hemorrhoids and is the most effective and complete treatment.
The surgeon makes incisions around the hemorrhoidal tissue and removes the offending swollen veins. The procedure is performed under anesthesia in an outpatient center or hospital.
- Best for: Large external hemorrhoids, combined internal and external hemorrhoids, and Grade III-IV prolapsed hemorrhoids.
- Effectiveness: Cures about 95% of cases with a very low recurrence rate. It is considered the gold standard for severe disease.
- Recovery: This procedure has a well-deserved reputation for being painful. Recovery can take 2 to 4 weeks, with significant pain during the first week, especially with bowel movements. Pain management is a key part of post-operative care.
Stapled Hemorrhoidopexy (PPH)
Also known as Procedure for Prolapse and Hemorrhoids (PPH), this is a less painful alternative to traditional hemorrhoidectomy.
It is used for prolapsed internal hemorrhoids. A circular stapling device is used to remove a ring of excess hemorrhoidal tissue from higher up in the anal canal.
This pulls the remaining hemorrhoidal cushions back up into their normal anatomical position and cuts off their blood supply, causing them to shrink.
- Best for: Grade III and some Grade IV internal hemorrhoids. It does not treat external hemorrhoids.
- Effectiveness: Effective for controlling prolapse and bleeding.
- Recovery: Significantly less painful than a hemorrhoidectomy, with a faster return to normal activities. However, it has a higher rate of recurrence and a risk of unique complications like rectal urgency or, rarely, severe issues like staple line stricture.
Hemorrhoidal Artery Ligation and Recto-Anal Repair (HAL-RAR)
This is a minimally invasive surgical technique that uses a small Doppler ultrasound probe to locate the arteries supplying blood to the hemorrhoids.
The surgeon then places a stitch around each artery to tie it off, cutting off the blood supply and causing the hemorrhoid to shrink.
If prolapse is present, an additional stitching technique (recto-anal repair) is used to lift and fix the prolapsed tissue back in place.
- Best for: Grades II and III internal hemorrhoids.
- Effectiveness: Good results for bleeding and prolapse, with less post-operative pain than hemorrhoidectomy.
- Recovery: Faster recovery and less pain compared to traditional surgery. Recurrence rates may be slightly higher than with hemorrhoidectomy.
What Are the Potential Complications of Untreated Hemorrhoids?
While rarely dangerous, ignoring persistent symptoms can lead to a few complications that can be uncomfortable and, in rare cases, serious.
- Anemia: While uncommon, chronic blood loss from bleeding hemorrhoids can lead to iron deficiency anemia. Symptoms include fatigue, weakness, pale skin, and shortness of breath. This is more likely with long-standing, frequent bleeding.
- Strangulated Hemorrhoid: If a prolapsed internal hemorrhoid becomes trapped by the anal sphincter muscles, its blood supply can be cut off. This is a “strangulated” hemorrhoid, which can cause extreme pain and may lead to tissue death (gangrene). This is a medical emergency requiring immediate attention.
- Thrombosis: As discussed earlier, a blood clot can form within an external hemorrhoid, causing a very painful, hard lump. While not dangerous, the pain can be severe.
- Skin Tags: After a clot in a thrombosed hemorrhoid dissolves or an external hemorrhoid resolves, it can leave behind a stretch of excess skin. These skin tags are generally harmless but can interfere with hygiene and become irritated.
- Infection: Though rare, open sores on external hemorrhoids can become infected.
How Can You Prevent Hemorrhoids?
The best way to prevent hemorrhoids is to keep your stools soft so they pass easily, avoiding straining and excess pressure.
The same lifestyle changes used to treat them are also the best methods of prevention.
- Eat High-Fiber Foods: Consistently consume 25-30 grams of fiber daily from fruits, vegetables, and whole grains. This is the cornerstone of prevention.
- Stay Hydrated: Drink 6-8 glasses of water per day to help fiber do its job.
- Don’t Strain: Listen to your body and go to the bathroom when you feel the urge. Avoid pushing hard or holding your breath.
- Stay Active: Regular exercise, such as 30 minutes of brisk walking daily, promotes healthy bowel function and helps maintain a healthy weight.
- Avoid Prolonged Sitting: Get up and move around regularly, especially if you have a desk job. Limit your time on the toilet to only what is necessary.
- Maintain a Healthy Weight: Losing excess weight can reduce the pressure on your pelvic and rectal veins.
The Overlooked Impact: Quality of Life and Mental Health
The physical symptoms are only part of the story. The condition can have a significant, though often unspoken, impact on a person’s quality of life and mental well-being.
The stigma and embarrassment associated with anal health issues prevent many from seeking help or even talking about their suffering.
A 2022 study published in BMC Public Health on the quality of life in patients with hemorrhoidal disease found that as symptom burden increases, quality of life decreases to levels below the general population average. Patients report that symptoms like pain, bleeding, and itching lead to:
- Emotional Burden: Feelings of fear (especially from bleeding), embarrassment, and anxiety are common. The fear of a sudden flare-up or an embarrassing accident can lead to chronic stress.
- Social Isolation: Patients may avoid social activities, exercise, or travel due to pain or fear of symptoms. The need for frequent bathroom trips or special accommodations can be disruptive.
- Daily Life Adjustments: Many people develop coping mechanisms that impact their daily routine, such as needing to get up earlier, using sanitary pads for bleeding or discharge, or avoiding certain types of clothing.
“I’ve lived with haemorrhoids, I understand what it is to have the burden of them – it’s not nice, it can be embarrassing to talk about… they play on your mind, impairing your comfort of life in so many ways.” – Patient story from OneWelbeck.
Recognizing this psychological toll is crucial. Seeking treatment is not just about managing physical symptoms, it’s about restoring your confidence and quality of life.
If hemorrhoids are affecting your mental health, know that you are not alone and effective treatments are available.
Frequently Asked Questions (FAQ)
1. How long do hemorrhoids last?
The duration varies. Small flare-ups may resolve within a few days with home care. Larger or more severe hemorrhoids can last for several weeks. Chronic hemorrhoids may have symptoms that come and go over months or years without proper lifestyle changes or treatment.
2. Can hemorrhoids go away on their own?
Yes, many small, symptomatic hemorrhoids can go away on their own, especially if the underlying cause (like temporary constipation or pregnancy) is resolved. Lifestyle changes, such as increasing fiber and water intake, can help them resolve faster and prevent recurrence.
3. What is the fastest way to get rid of hemorrhoids?
For immediate symptom relief at home, a sitz bath can reduce pain and swelling quickly. For a thrombosed hemorrhoid, seeing a doctor within 72 hours for a clot removal (thrombectomy) is the fastest way to resolve severe pain. Long-term, dietary changes are key.
4. What should you not do if you have hemorrhoids?
Avoid straining during bowel movements, sitting on the toilet for long periods, and using dry, rough toilet paper. Also, avoid a low-fiber, low-fluid diet, as this leads to constipation. Aggressive wiping and cleaning of the anal area should also be avoided.
5. Does walking help hemorrhoids?
Yes, moderate exercise like brisk walking is excellent for hemorrhoids. It helps stimulate bowel function to prevent constipation and improves blood flow and circulation in the rectal area, which can help reduce pressure on the veins and promote healing.
6. What do bleeding hemorrhoids look like?
Bleeding from hemorrhoids typically involves small amounts of bright red blood. You may see it on the toilet paper after wiping, as drops in the toilet bowl, or as streaks on the stool’s surface. Dark, tarry, or clotted blood is not typical and requires immediate medical evaluation.
7. Can stress cause hemorrhoids?
Stress itself doesn’t directly cause hemorrhoids, but it can contribute to digestive issues like constipation or diarrhea, which are major risk factors. High stress levels can alter gut function and lead to behaviors (like poor diet) that increase the likelihood of a flare-up.
8. Is it okay to pop a hemorrhoid?
No, you should never attempt to pop a hemorrhoid. This can lead to severe pain, significant bleeding, and a high risk of infection. A thrombosed hemorrhoid contains a blood clot, not pus, and must be treated by a medical professional in a sterile environment.
Conclusion
Hemorrhoids are a common and highly treatable condition. While they can cause significant discomfort and affect your quality of life, the vast majority of cases can be managed and prevented with simple, consistent lifestyle changes.
Increasing your fiber and water intake, staying active, and practicing healthy toilet habits are the most powerful tools at your disposal.
For symptoms that persist, a range of effective and minimally invasive medical treatments can provide lasting relief. The most important step is to overcome any embarrassment and seek a proper diagnosis from a healthcare professional.
This ensures your symptoms are not caused by a more serious condition and opens the door to a personalized treatment plan.
Don’t let hemorrhoids control your life. Take action today by implementing the strategies in this guide and consulting with your doctor. Your path to comfort and peace of mind is within reach.
Have you found a particular home remedy or lifestyle change that worked for you? Share your experience in the comments below to help others in the community!

