To get rid of heartburn, you can use fast-acting solutions like over-the-counter antacids and simple posture changes.
For long-term relief, the focus shifts to identifying and avoiding dietary triggers, making key lifestyle adjustments, and understanding when it’s crucial to seek professional medical advice for persistent symptoms.
This burning sensation is far more than just an occasional nuisance.
It’s a widespread issue affecting over 60 million Americans at least once a month.
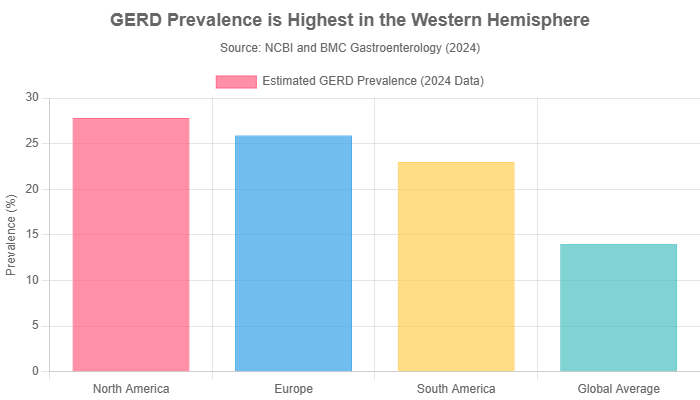
More significantly, recent 2024 data reveals that its chronic and more severe form, Gastroesophageal Reflux Disease (GERD), impacts up to 27.8% of the North American population, underscoring a major public health concern that disrupts daily life and carries long-term risks if left unmanaged.
This comprehensive guide will walk you through everything you need to know to conquer heartburn.
We will explore immediate relief strategies, evaluate science-backed natural remedies, and detail sustainable long-term lifestyle changes to prevent its recurrence.
Critically, we will also clarify the vital differences between heartburn and a heart attack, equipping you with the knowledge to act safely and decisively.
Continue reading to take control of your digestive health and find lasting relief from that familiar, unwelcome burn.
In This Article
Part 1: Understanding the Burn: What Is Heartburn and Why Does It Happen?
Before we can effectively treat and prevent heartburn, it’s essential to understand what it is and the mechanical failures behind the sensation.
This section demystifies the condition, moving beyond a simple definition to explain the physiological processes in an accessible way.
This foundational knowledge is the first step toward mastering your digestive health and achieving long-term heartburn relief.
What Does Heartburn Feel Like?
At its core, heartburn is a symptom, not a disease.
It’s characterized by a distinct burning pain or discomfort in the chest, typically located just behind the breastbone.
This sensation can range from mild and fleeting to severe and persistent. Many people also experience:
- A sour, acidic, or bitter taste in the back of the throat, known as regurgitation.
- Pain that intensifies after eating, in the evening, or when lying down or bending over.
- A feeling of pressure or fullness in the chest.
- Occasional coughing or hoarseness, especially in the morning.
To understand why this happens, it helps to use an analogy.
Think of your esophagus—the tube connecting your throat to your stomach—as a one-way street for food.
At the bottom of this street is a critical gatekeeper: a ring of muscle called the lower esophageal sphincter (LES).
In a healthy system, the LES opens to let food pass into the stomach and then snaps shut tightly to keep the stomach’s highly acidic contents where they belong.
Heartburn occurs when this gatekeeper fails.
When the LES is weak or relaxes at the wrong time, it allows corrosive stomach acid to flow backward (reflux) into the esophagus, which isn’t designed to handle such acidity.
This chemical irritation of the esophageal lining is what you perceive as the burning pain of heartburn.
The Primary Causes of Heartburn
The failure of the LES isn’t random, it’s often triggered by a combination of physiological conditions, dietary choices, and lifestyle habits.
Understanding what causes heartburn for you is the key to effective prevention.
Physiological Factors
These are underlying physical conditions that can compromise the integrity of the barrier between the stomach and esophagus.
- Weak Lower Esophageal Sphincter (LES): This is the most direct cause. For some individuals, the LES muscle is inherently weak or experiences transient relaxations not related to swallowing, allowing for frequent reflux.
- Hiatal Hernia: This condition occurs when the upper part of the stomach bulges up through the diaphragm (the large muscle separating your abdomen and chest) into the chest cavity. A hiatal hernia can weaken the LES and disrupt the normal pressure gradient that helps prevent reflux.
- Pregnancy: Heartburn is extremely common during pregnancy due to a dual-front attack. Hormones like progesterone cause the LES muscle to relax, while the growing uterus increases physical pressure on the stomach, pushing its contents upward.
Common Dietary Triggers
Certain foods and drinks are notorious for either relaxing the LES, increasing stomach acid production, or slowing down digestion, all of which contribute to heartburn.
- Spicy Foods: Compounds like capsaicin can irritate the esophagus and may slow stomach emptying.
- Fried or High-Fat Foods: These foods take longer to digest, meaning they sit in the stomach longer, increasing the window of opportunity for reflux. They can also cause the LES to relax.
- Chocolate: Contains methylxanthine, a compound that has been shown to relax the smooth muscle of the LES.
- Citrus Fruits and Juices: Oranges, grapefruits, and lemons are highly acidic and can worsen the burning sensation if reflux occurs.
- Tomatoes and Tomato-Based Products: Like citrus, tomatoes (and products like ketchup, marinara sauce, and chili) are acidic and common triggers.
- Onions and Garlic: Especially in their raw form, these can trigger heartburn in many individuals, though the exact mechanism is not fully understood.
- Peppermint: While often thought of as a digestive aid, peppermint can relax the LES, making it a common culprit for reflux.
- Carbonated Beverages, Coffee, and Alcohol: Carbonation can increase stomach pressure. Caffeine and alcohol can both relax the LES and stimulate acid production.
Lifestyle and Behavioral Factors
Your daily habits play a massive role in managing or exacerbating heartburn.
- Obesity: Excess body weight, particularly around the abdomen, increases intra-abdominal pressure. This pressure physically squeezes the stomach, promoting the backflow of acid.
- Smoking: Smoking has a multi-pronged negative effect. It can directly relax the LES, impair the muscle’s function, and reduce the production of saliva, which is the body’s natural acid buffer. Research shows that quitting smoking can significantly reduce reflux symptoms.
- Eating Habits: Consuming large meals fills the stomach and increases pressure on the LES. Similarly, eating within 2-3 hours of lying down means gravity is no longer on your side to help keep acid down.
- Wearing Tight-Fitting Clothing: Belts, waistbands, or shapewear that constrict the abdomen can increase pressure on the stomach, much like excess weight does, forcing acid upward.
Part 2: Fast Heartburn Relief: How to Stop the Pain Now
When the fire of heartburn strikes, your immediate priority is to extinguish it.
This section is designed to be highly actionable, providing a clear guide to the most effective strategies for rapid relief.
We’ll compare different over-the-counter options and explore evidence-based home remedies to help you find comfort quickly.
Over-the-Counter (OTC) Medications: Your First Line of Defense
The pharmacy aisle offers several effective options for immediate and short-term heartburn relief.
They work in different ways and are suited for different situations. Understanding the distinction is key to choosing the right tool for the job.
| Medication Type | How It Works | Speed of Relief | Best For | Common Examples |
|---|---|---|---|---|
| Antacids | Neutralizes existing stomach acid on contact, acting like a chemical buffer. | Very Fast (within minutes) | Occasional, mild heartburn that occurs after a specific meal. Provides immediate but short-lived relief. | Tums (Calcium Carbonate), Rolaids (Calcium Carbonate, Magnesium Hydroxide), Mylanta (Aluminum Hydroxide, Magnesium Hydroxide) |
| H2 Blockers | Reduces acid production by blocking histamine-2, a chemical signal that tells the stomach to make acid. | Slower (30-90 mins), but lasts longer (up to 12 hours) | Preventing heartburn when taken 30-60 minutes before a known trigger meal. Also treats existing mild-to-moderate heartburn. | Pepcid (Famotidine), Tagamet (Cimetidine) |
| Proton Pump Inhibitors (PPIs) | Blocks acid production more potently and for a longer duration by shutting down the “pumps” in stomach cells that secrete acid. | Slowest (1-4 days for full effect) | Frequent, moderate-to-severe heartburn (occurring 2+ days a week). Not for immediate relief, but for ongoing management. | Prilosec (Omeprazole), Nexium (Esomeprazole), Prevacid (Lansoprazole) |
Science-Backed Home Remedies for Quick Comfort
While medications are effective, several simple, non-pharmacological strategies can provide surprisingly fast heartburn relief. It’s important to separate evidence-based remedies from old wives’ tales.
- Stand Up and Loosen Your Belt: This is the simplest and often most effective immediate action. Standing upright enlists gravity to help pull acid back down into the stomach. Simultaneously, loosening any tight clothing around your waist immediately reduces the external pressure on your stomach, giving acid less reason to move upward.
- Baking Soda (Sodium Bicarbonate): A half-teaspoon of baking soda mixed in a small glass of water can act as a powerful, fast-acting antacid. It’s a base (alkaline) that chemically neutralizes stomach acid. Crucial Warning: This is a short-term fix only. Baking soda is very high in sodium, which can be dangerous for those on a low-sodium diet or with high blood pressure. Overuse can also lead to “acid rebound”, where the stomach overcompensates by producing even more acid later. Use it sparingly, if at all.
- Chew Sugar-Free Gum: The act of chewing stimulates saliva production. According to research on the topic, this increased saliva flow does two things: it helps neutralize the acid in the esophagus, and the repeated swallowing helps wash the acid back down into the stomach more quickly. Choose a non-mint flavor, as mint can relax the LES.
- Sip a Small Amount of Water: Slowly sipping a few ounces of room-temperature water can help dilute the acid in your esophagus and gently wash it back into the stomach. Avoid chugging a large amount, as this can increase stomach volume and pressure, potentially worsening the problem.
- Herbal Solutions with Emerging Evidence:
- Deglycyrrhizinated Licorice (DGL): Unlike standard licorice, DGL has had the compound glycyrrhizin (which can raise blood pressure) removed. Some studies suggest DGL may work by increasing the production of mucus in the stomach and esophagus, which forms a protective barrier against acid. It’s available as chewable tablets.
- Ginger Tea: Ginger is well-known for its anti-inflammatory and anti-nausea properties. A small cup of warm ginger tea can help soothe an irritated stomach and esophagus. However, moderation is key, large quantities of ginger can be a heartburn trigger for some individuals.
Part 3: Long-Term Solutions: Preventing Heartburn from Coming Back
While fast fixes are essential for acute discomfort, the ultimate goal is to prevent heartburn from occurring in the first place.
This requires a shift from a reactive to a proactive mindset.
This section focuses on sustainable, evidence-based strategies for long-term management, empowering you to make lasting changes for a reflux-free life.
The Anti-Heartburn Diet: Strategic Eating for Lasting Relief
Managing heartburn long-term is less about restrictive dieting and more about smart, strategic choices.
It involves not only avoiding triggers but actively incorporating foods that promote digestive health.
Foods to Embrace
These foods are generally low-acid, easy to digest, and can help absorb excess stomach acid.
- High-Fiber Foods: Fiber promotes healthy digestion and can make you feel full, reducing the likelihood of overeating. Excellent choices include oatmeal, brown rice, whole-grain bread, sweet potatoes, carrots, and beets.
- Alkaline Foods: These foods have a higher pH, which can help offset strong stomach acid. Think bananas, melons (cantaloupe, honeydew), cauliflower, fennel, and nuts.
- Watery Foods: Foods with high water content can dilute and weaken stomach acid. Include celery, cucumber, lettuce, and watermelon in your diet.
- Lean Proteins: Choose baked, grilled, or broiled options over fried ones. Lean chicken, turkey, fish, and tofu are excellent choices that are less likely to trigger reflux than fatty meats.
Eating Habits That Matter
How you eat is just as important as what you eat.
- Eat Smaller, More Frequent Meals: Instead of three large meals, try five or six smaller ones throughout the day. This prevents the stomach from becoming overly full, which reduces pressure on the LES.
- Avoid Eating Within 3 Hours of Bedtime: This is one of the most critical rules. Giving your stomach ample time to empty before you lie down significantly reduces the risk of nighttime heartburn.
- Sit Upright: Eat your meals while sitting up straight and remain upright (sitting or standing) for at least 30-60 minutes afterward. This allows gravity to assist in digestion and keep stomach contents down.
Key Lifestyle Adjustments for a Reflux-Free Life
Beyond diet, several lifestyle modifications have been proven to dramatically reduce the frequency and severity of heartburn.
- Maintain a Healthy Weight: The link between excess weight and GERD is well-established. As noted by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), even a modest amount of weight loss can significantly decrease pressure on the abdomen and reduce reflux episodes.
- Elevate the Head of Your Bed: This is a simple yet powerful mechanical fix for nighttime reflux. Use 6- to 8-inch blocks or risers under the posts at the head of your bed. A wedge pillow that elevates your entire torso is also effective. Simply stacking pillows is not recommended, as it can bend your body at the waist, increasing abdominal pressure and making heartburn worse.
- Quit Smoking: If you smoke, quitting is one of the most impactful things you can do for your reflux. As mentioned earlier, smoking weakens the LES, reduces protective saliva, and can increase acid production. The benefits of quitting extend far beyond just heartburn relief.
- Manage Stress: The gut-brain axis is a powerful connection. Stress doesn’t directly cause reflux, but it can increase the production of stomach acid and make the esophagus more sensitive to irritation. Incorporating evidence-based stress-reduction techniques can be highly beneficial. Consider:
- Mindfulness Meditation: Focusing on the present moment can help calm the nervous system.
- Deep Breathing Exercises: Slow, diaphragmatic breathing can lower stress hormones and have a calming physical effect.
- Yoga or Tai Chi: These practices combine gentle movement, breathing, and meditation to reduce stress and improve overall well-being.
Part 4: Is It Just Heartburn? Recognizing Red Flags
This section addresses one of the most critical and anxiety-provoking questions for anyone experiencing chest pain: is it simple heartburn or something far more serious, like a heart attack?
Understanding the key differences is vital for your safety.
We will also outline clear, unambiguous red flags that indicate it’s time to stop self-treating and seek professional medical help.
This information is essential for making safe and responsible health decisions.
Heartburn vs. Heart Attack: How to Tell the Difference
While the symptoms can sometimes overlap, there are classic distinguishing features.
However, the most important rule is to err on the side of caution.
The consequences of ignoring a heart attack are infinitely greater than those of having a false alarm.
| Symptom Feature | Typical Heartburn | Possible Heart Attack |
|---|---|---|
| Type of Pain | A sharp, burning sensation that feels like it’s rising from the stomach into the chest and throat. | Feels like intense pressure, tightness, squeezing, or aching in the center of the chest. Often described as “an elephant sitting on my chest”. |
| Pain Location | Primarily located behind the breastbone. The pain may move up toward the throat. | Pain can radiate from the chest to the shoulders, neck, jaw, back, or one or both arms (more commonly the left). |
| Related Symptoms | Often accompanied by a sour or acidic taste in the mouth (regurgitation) and sometimes burping. | Frequently occurs with shortness of breath, a cold sweat, nausea, vomiting, dizziness, or extreme fatigue. |
| Triggers & Relief | Often occurs after eating a large or trigger meal, bending over, or lying down. Usually improves with antacids or by standing up. | Can occur at any time, often triggered by physical exertion or emotional stress, but can also happen at rest. Pain is persistent and does not improve with antacids. |
CRITICAL MEDICAL WARNING
If you have any doubt about the cause of your chest pain, especially if it’s accompanied by shortness of breath, sweating, or pain radiating to your arm or jaw, call 911 or seek emergency medical help immediately. This is particularly important if you have risk factors for heart disease, such as high blood pressure, high cholesterol, diabetes, a history of smoking, or a family history of heart disease. Do not try to self-diagnose a potential heart attack.
When to See a Doctor for Your Heartburn
Even when it’s clearly not a heart attack, persistent heartburn warrants a visit to a healthcare professional.
Self-treating a chronic problem can mask a more serious underlying condition.
Here is a clear checklist of non-emergency situations where you should make an appointment:
- You experience heartburn more than twice a week, and it’s disrupting your life.
- Your symptoms persist or worsen despite consistent use of over-the-counter medications.
- You have difficulty swallowing (a condition known as dysphagia) or feel a sensation of food being stuck in your throat or chest.
- You have persistent, unexplained nausea or vomiting.
- You have lost weight without trying.
- You notice your stools are black, tarry, or contain visible blood, which can be a sign of bleeding in the digestive tract.
- You have chronic hoarseness, a persistent sore throat, or a cough that won’t go away.
Part 5: The Deeper Dive: Chronic Heartburn (GERD) and Associated Risks
This section elevates the discussion from occasional discomfort to the clinical realities of chronic reflux.
We’ll explore what it means when heartburn becomes a daily battle, the potential long-term health consequences of untreated acid exposure, and the important considerations regarding the medications used for long-term management.
This is crucial for a complete understanding of the condition.
From Heartburn to GERD: When It Becomes a Chronic Condition
While nearly everyone experiences occasional heartburn, Gastroesophageal Reflux Disease (GERD) is diagnosed when this reflux is frequent and severe enough to be considered a chronic condition.
The general clinical guideline is experiencing mild acid reflux at least twice a week, or moderate to severe reflux at least once a week. GERD is not just more frequent heartburn, it’s a disease that can lead to significant complications if not properly managed.
If your doctor suspects GERD, they may recommend diagnostic tests to assess the extent of the problem and rule out other issues. These can include:
- Upper Endoscopy: A thin, flexible tube with a camera is passed down your throat to visually inspect the esophagus, stomach, and upper small intestine for inflammation or damage.
- Ambulatory Acid (pH) Probe Test: A small monitor is placed in your esophagus to measure when, and for how long, stomach acid refluxes there over a 24-hour period. This is the gold standard for diagnosing reflux.
The Hidden Dangers: Complications of Untreated GERD
Constant exposure to stomach acid can cause serious damage to the delicate lining of the esophagus over time.
These complications are why managing GERD is so important.
- Esophagitis: This is inflammation, irritation, or swelling of the esophagus. It can cause painful swallowing, chest pain, and can lead to ulcers or scarring.
- Esophageal Strictures: Over time, the damage from acid can cause scar tissue to form, which narrows the esophagus. This can make it difficult for food to pass through, leading to swallowing problems.
- Barrett’s Esophagus: This is a serious complication where the tissue lining the esophagus changes, becoming more like the tissue that lines the intestine. According to data from the NCBI, Barrett’s esophagus can be found in 5% to 12% of patients with chronic GERD symptoms. This condition is a significant concern because it is a known precursor to esophageal adenocarcinoma, a type of cancer.
A Word of Caution: The Risks of Long-Term Medication Use
Proton Pump Inhibitors (PPIs) are incredibly effective at controlling GERD, but their widespread, long-term use has become a topic of medical discussion.
While the benefits often outweigh the risks for those with severe GERD or Barrett’s esophagus, it’s important to be aware of potential associations.
This balanced perspective is crucial for informed decision-making with your doctor.
According to institutions like Yale Medicine, potential concerns associated with long-term PPI use include:
- Nutrient Deficiencies: PPIs can interfere with the absorption of essential micronutrients, including Vitamin B12, magnesium, and calcium.
- Increased Fracture Risk: The link to poor calcium absorption may contribute to a higher risk of bone fractures, particularly of the hip, wrist, and spine, in older adults.
- Infections: By reducing stomach acid, a natural defense against ingested pathogens, there may be a slightly increased risk of certain infections, including pneumonia and the intestinal bacterium Clostridioides difficile (C. diff).
It is essential to emphasize that you should never stop taking a prescribed medication without consulting your doctor. The risks of untreated GERD, such as Barrett’s esophagus, are often far greater than the potential risks of the medication. The goal is to use the lowest effective dose for the shortest necessary time, a strategy you should develop in partnership with your healthcare provider.
Frequently Asked Questions (FAQ)
1. How long does heartburn last?
Heartburn typically lasts from a few minutes to several hours. The duration depends on the trigger and any actions taken for relief. It usually subsides once the trigger food is digested or after taking an antacid.
2. Can drinking water help heartburn?
Yes, sipping small amounts of water can help. It works by diluting stomach acid and helping to wash it out of the esophagus. However, avoid drinking a large amount quickly, as this can increase stomach pressure and worsen symptoms.
3. Why is my heartburn worse at night?
When you lie down, you lose the assistance of gravity that helps keep stomach acid in the stomach. This horizontal position makes it much easier for acid to flow backward into the esophagus, leading to more frequent and severe nighttime symptoms.
4. Is it safe to take Tums or other antacids every day?
Occasional use of antacids like Tums is generally safe. However, daily, long-term use can mask a more serious underlying condition like GERD and may lead to side effects like electrolyte imbalances. If you need antacids daily, consult a doctor.
5. What is the fastest way to neutralize stomach acid?
The fastest way is to take a calcium carbonate-based antacid (e.g., Tums, Rolaids), which begins neutralizing acid on contact. A small amount of baking soda (sodium bicarbonate) in water also works very quickly but carries risks and should be used with caution.
6. Can stress cause heartburn?
Yes, stress is a well-known factor. While it may not be the direct cause of reflux, stress can increase stomach acid production, slow digestion, and heighten your perception of pain, making the esophagus more sensitive to even small amounts of acid.
7. Does apple cider vinegar really help heartburn?
The evidence for apple cider vinegar is purely anecdotal. While some individuals report relief, there is no scientific consensus to support its use. As an acid itself, it has the potential to worsen heartburn symptoms for many people.
8. What position should I sleep in to avoid heartburn?
Sleeping on your left side with your head and torso elevated is the best position. This posture uses gravity and the natural anatomy of the stomach to make it physically more difficult for acid to flow into the esophagus.
Conclusion
Navigating the world of heartburn can feel overwhelming, but relief and prevention are well within your reach.
We’ve learned that heartburn is fundamentally a mechanical issue—the backflow of stomach acid into an unprotected esophagus. The path to comfort involves a two-pronged approach.
- For immediate relief, you have powerful tools at your disposal, from fast-acting OTC medications like antacids to simple, effective remedies like standing up and letting gravity do its work.
- For long-term prevention, the focus shifts to proactive, sustainable habits. This includes making smart dietary choices, maintaining a healthy weight, elevating the head of your bed for sleep, and managing stress.
Crucially, it is vital to be vigilant—to understand the critical differences between heartburn vs. a heart attack and to recognize the red flags that signal the need for professional medical evaluation.
You have the power to manage and even prevent the discomfort of heartburn.
By understanding your personal triggers and consistently implementing these evidence-based strategies, you can achieve lasting comfort and safeguard your long-term digestive health.
If your symptoms are frequent, severe, or concerning, do not hesitate to partner with a healthcare professional.
They can help you create a personalized treatment plan, ensure an accurate diagnosis, and rule out more serious conditions. Your health is a collaborative effort.
What’s your go-to tip for fast heartburn relief? Share your experience in the comments below to help others in the community!
Reference
[1] Natural Home Remedies for Heartburn
https://www.webmd.com/heartburn-gerd/home-heartburn-remedies-natural-remedies-heartburn
[2] Improving treatment of people with gastro-esophageal reflux …
https://www.nature.com/articles/s43856-024-00632-6
[3] Heartburn vs. Heart Attack: How to Tell the Difference
[4] GERD: Can certain medications make it worse? – Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/gerd/expert-answers/heartburn-gerd/faq-20058535
[5] Is the Long-Term Use of Antacids Safe? – University Hospitals
https://www.uhhospitals.org/blog/articles/2024/03/is-the-long-term-use-of-antacids-safe
[6] Heartburn or Heart Attack? Signs of Both & How to Tell the Difference
[7] Natural Products in the Management of Gastroesophageal …

