Improving gut health for women involves a holistic approach that goes beyond simple digestion.
It requires a conscious focus on diet, stress management, and targeted supplementation to balance the trillions of microorganisms in your gut.
This intricate ecosystem, known as the microbiome, profoundly influences everything from your mood to the clarity of your skin.
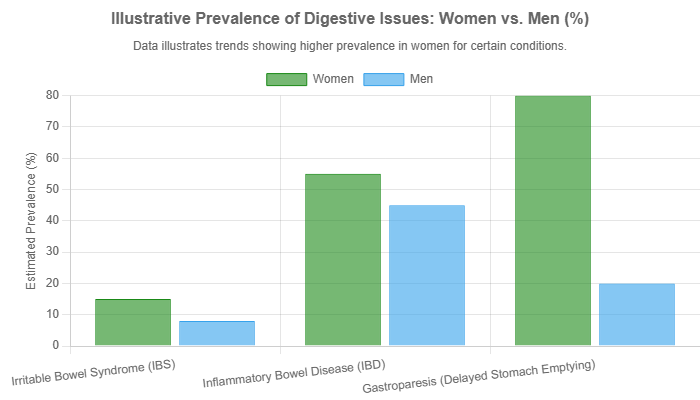
Did you know that women are significantly more likely to suffer from digestive issues? Conditions like Irritable Bowel Syndrome (IBS) are estimated to affect up to 20% of the population, with women being disproportionately represented.
This isn’t a coincidence; it’s a reflection of the unique biological factors, including hormonal fluctuations, that shape a woman’s gut environment.
This guide will delve into the science behind the gut-brain-skin connection, explore how hormones play a pivotal role, and provide a clear, actionable plan to help you cultivate a healthier gut for a more vibrant life.
In This Article
Why is Gut Health for Women a Unique Concern?
While gut health is universal, the female experience is distinct.
Hormonal cycles, life stages like pregnancy and menopause, and a higher prevalence of certain autoimmune conditions create a unique landscape for the female gut microbiome.
Understanding these differences is the first step toward effective and personalized care.
The Influence of Hormones
One of the most fascinating aspects of gut health for women is the estrobolome.
This term refers to a specific collection of gut bacteria capable of metabolizing and modulating the body’s estrogen levels.
These microbes produce an enzyme called β-glucuronidase, which converts inactive estrogen back into its active form, allowing it to re-enter circulation.
When the estrobolome is balanced, it helps maintain hormonal equilibrium. However, dysbiosis (an imbalanced gut) can disrupt this process.
A 2017 study in Maturitas highlighted that an altered estrobolome can lead to either a deficiency or an excess of free estrogen, contributing to conditions like:
- Polycystic Ovary Syndrome (PCOS)
- Endometriosis
- Infertility
- Mood swings and weight fluctuations
- Increased risk for certain estrogen-related cancers
This intricate dance between your gut microbes and hormones underscores why a gut-centric approach is crucial for overall female wellness.
Gut Health Through a Woman’s Life Stages
A woman’s microbiome is not static; it evolves significantly through different life phases, largely driven by hormonal shifts.
Research published in the World Journal of Clinical Cases details these dynamic changes:
- Puberty: The rise in estrogen helps shape a health-promoting gut and vaginal microbiota, establishing a foundation for reproductive health.
- Pregnancy: The microbiome shifts dramatically to support maternal metabolic changes and fetal growth. This includes a “low-grade” inflammatory state that is normal and necessary for a healthy pregnancy.
- Menopause: As estrogen levels decline, gut microbial diversity often decreases, sometimes becoming more similar to that of age-matched men. This shift can be linked to menopausal symptoms like weight gain, mood changes, and an increased risk of metabolic issues.
What is the Gut-Brain Connection and How Does It Affect Your Mood?
The feeling of “butterflies in your stomach” is more than just a metaphor.
It’s a real-time demonstration of the gut-brain connection, a complex, bidirectional communication network linking the central nervous system with the enteric nervous system (the “second brain” in your gut).
How Your Gut “Talks” to Your Brain
This conversation happens through several pathways:
- Neurotransmitters: Your gut microbes produce a vast array of neurotransmitters, including an estimated 95% of the body’s serotonin (the “feel-good” chemical) and Gamma-Aminobutyric Acid (GABA), which has calming effects.
- The Vagus Nerve: This major nerve acts as a superhighway, transmitting signals directly between the gut and the brain.
- Immune System: Gut dysbiosis can trigger inflammation, sending inflammatory signals (cytokines) to the brain, which can impact mood and cognitive function. Johns Hopkins Medicine explains that irritation in the gut can send signals to the brain that trigger mood changes.
Signs Your Mood Might Be Linked to Your Gut
While not a diagnostic tool, persistent issues like the following could suggest a link between your gut health and mental well-being:
- Chronic anxiety or feelings of depression that don’t respond to other interventions.
- “Brain fog” or difficulty concentrating.
- Increased irritability, especially when accompanied by digestive upset.
- Heightened stress response.
A 2024 study found that a prebiotic fiber intervention could positively alter mood in daily life, demonstrating a direct link between what we feed our gut and how we feel.
How Does the Gut-Skin Axis Impact Your Complexion?
The idea that internal health reflects on our skin is ancient wisdom, now validated by modern science through the concept of the gut-skin axis.
This axis describes how the health of your gut microbiome can directly influence the health and appearance of your skin.
Understanding “Leaky Gut” and Its Link to Skin Problems
A central mechanism in the gut-skin axis is intestinal permeability, often called “leaky gut“. In a healthy gut, the intestinal lining forms a tight barrier.
When this barrier is compromised, undigested food particles, toxins, and bacteria can “leak” into the bloodstream.
This triggers a systemic inflammatory response as the immune system attacks these foreign invaders.
This chronic, low-grade inflammation can manifest anywhere in the body, and the skin is a common target.
It can exacerbate inflammatory skin conditions and contribute to a dull, reactive complexion.
The Microbiome’s Role in Acne, Eczema, and Rosacea
Research increasingly connects gut dysbiosis to specific skin disorders:
- Acne: A 2022 review found that acne patients often have altered gut microbiota, with lower levels of beneficial bacteria. This imbalance can influence inflammation and sebum production.
- Atopic Dermatitis (Eczema): Studies show that modulating the gut microbiome with probiotics can improve skin barrier function and reduce the severity of eczema symptoms.
- Rosacea: This condition is strongly linked to gut inflammation, with a higher prevalence of Small Intestinal Bacterial Overgrowth (SIBO) found in rosacea patients.
Probiotics for Skin: What Does the Science Say?
The evidence for using probiotics to improve skin health is growing.
A comprehensive 2023 review highlighted several ways oral probiotics can benefit the skin:
- Improving Moisturization: Certain strains like Lactobacillus plantarum can increase skin ceramide levels, enhancing the skin’s moisture barrier.
- Anti-Aging Effects: Probiotics can help combat photoaging by reducing the expression of enzymes that break down collagen (MMPs) and by providing antioxidant effects.
- Strengthening the Skin Barrier: By improving gut barrier integrity, probiotics reduce systemic inflammation that can damage the skin.
What Are the Best Foods to Cultivate a Healthy Gut?
Building a resilient microbiome starts on your plate.
The goal is diversity—feeding your gut a wide variety of plant-based foods provides the different fibers and nutrients that diverse beneficial microbes need to thrive.
The Power of Prebiotics: Fueling Your Good Bacteria
Prebiotics are types of fiber that your body can’t digest, but your gut bacteria love to eat.
They are the essential fuel for a healthy microbiome. OHSU’s Center for Women’s Health emphasizes that prebiotics are key to making sure your good bacteria are healthy and thriving. Excellent sources include:
- Garlic, Onions, and Leeks
- Asparagus
- Bananas (especially slightly unripe)
- Oats and Barley
- Chicory Root
- Flaxseeds
Probiotic Powerhouses: Fermented Foods and Their Benefits
Probiotic foods contain live beneficial bacteria that can help populate your gut.
Incorporating these into your diet is a natural way to support your microbiome:
- Yogurt and Kefir: Look for “live and active cultures” and minimal added sugar.
- Sauerkraut and Kimchi: Fermented cabbage dishes packed with probiotics.
- Miso: A fermented soybean paste used in Japanese cuisine.
- Kombucha: A fermented tea, but be mindful of sugar content.
- Tempeh: A fermented soybean cake that’s also a great source of protein.
Polyphenol-Rich Foods: The Unsung Heroes
Polyphenols are antioxidant compounds found in plants.
They not only fight oxidative stress but also act as prebiotics, feeding beneficial bacteria like Akkermansia muciniphila, which is crucial for a healthy gut lining. Find them in:
- Berries (blueberries, raspberries)
- Dark Chocolate (70% cocoa or higher)
- Green Tea
- Olive Oil
- Nuts and Seeds
| Nutrient Type | Function | Top Food Sources for Women’s Gut Health |
|---|---|---|
| Prebiotics | Fuel for beneficial gut bacteria. | Garlic, onions, oats, flaxseed, asparagus, chicory root. |
| Probiotics | Introduce live beneficial bacteria. | Yogurt, kefir, sauerkraut, kimchi, miso, tempeh. |
| Polyphenols | Antioxidants that also feed good microbes. | Berries, dark chocolate, green tea, olive oil, red wine. |
Which Probiotic Supplements Are Best for Women?
While a food-first approach is ideal, probiotic supplements can provide a more targeted and potent dose of beneficial bacteria, especially for addressing specific concerns related to gut health for women.
Key Strains to Look For
Not all probiotics are created equal. Different strains have different benefits. For women’s health, look for products containing:
- Lactobacillus species (e.g., L. rhamnosus, L. reuteri, L. acidophilus): These are well-researched for supporting vaginal health, preventing UTIs, and improving digestive and skin health.
- Bifidobacterium species (e.g., B. lactis, B. longum): Known for supporting overall gut barrier function, reducing inflammation, and alleviating symptoms of IBS.
Reading the Label: CFUs, Strains, and Quality
- CFU (Colony Forming Units): This indicates the number of live microbes. A dose between 10 to 50 billion CFUs is generally effective for daily support.
- Strain Specificity: A good product will list the specific strains (e.g., Lactobacillus rhamnosus GG), not just the genus.
- Delivery Technology: Look for delayed-release capsules designed to protect the bacteria from stomach acid so they can reach your intestines alive.
What Lifestyle Changes Support a Thriving Microbiome?
Diet is only one piece of the puzzle. Your daily habits have a profound impact on your gut ecosystem.
The Critical Role of Stress Management
Chronic stress is a primary enemy of gut health.
The stress hormone cortisol can decrease beneficial bacteria, increase gut permeability, and alter gut motility. Integrating stress-reduction practices is non-negotiable:
- Mindfulness and Meditation: Even 10 minutes a day can lower cortisol.
- Deep Breathing Exercises: Activates the vagus nerve, promoting a “rest and digest” state.
- Spending Time in Nature: Proven to reduce stress and improve mood.
Exercise: More Than Just Burning Calories
Regular, moderate exercise is fantastic for your gut. It increases microbial diversity and promotes the growth of butyrate-producing bacteria.
Butyrate is a short-chain fatty acid that is the primary fuel for your colon cells and has powerful anti-inflammatory effects.
Aim for a mix of cardiovascular activity and strength training.
The Importance of Sleep for Gut Repair
Your gut, like your brain, follows a circadian rhythm.
Poor sleep disrupts this rhythm, negatively impacting microbial diversity and function.
Prioritizing 7-9 hours of quality sleep per night allows your gut lining to repair and regenerate.
What Should You Avoid for Better Gut Health?
Just as important as what you add to your diet is what you limit.
Certain foods and substances can wreak havoc on your microbiome:
- Ultra-Processed Foods: These are typically high in sugar, unhealthy fats, and artificial additives, which feed pathogenic bacteria and promote inflammation.
- Excessive Sugar: Sugar fuels the growth of yeast and harmful bacteria, contributing to dysbiosis.
- Artificial Sweeteners: Some studies suggest that sweeteners like aspartame and sucralose can negatively alter the composition of the gut microbiome.
- Unnecessary Antibiotics: While lifesaving when needed, antibiotics are indiscriminate, wiping out both good and bad bacteria. Always use them as prescribed and focus on rebuilding your gut health afterward.
How Can I Tell if My Gut Health is Improving?
Healing your gut is a journey, not an overnight fix. Look for gradual, positive changes:
- Improved Digestion: Less bloating, gas, and more regular, well-formed bowel movements.
- Increased Energy Levels: Better nutrient absorption leads to more stable energy.
- Clearer Skin: A reduction in inflammatory skin issues.
- More Stable Mood: Fewer dramatic swings and a greater sense of well-being.
- Stronger Immunity: Fewer colds and infections.
Keeping a simple journal to track your food, symptoms, and lifestyle habits can be an invaluable tool for noticing these patterns of improvement.
Conclusion: Your Gut is Your Foundation
Nurturing your gut health is one of the most powerful investments you can make in your overall well-being. The connections between your microbiome and your mood, skin, hormones, and immunity are undeniable. By adopting a holistic approach that combines a diverse, plant-rich diet, mindful lifestyle habits, and targeted supplementation, you can cultivate a thriving internal ecosystem. Start with one small change today—perhaps adding a fermented food to your lunch or taking a 10-minute walk after dinner. Your body will thank you for it.
Frequently Asked Questions (FAQ) about Gut Health for Women
- How long does it take to heal your gut?
It varies greatly, but you may notice initial improvements in digestion within a few weeks. Significant, lasting changes to the microbiome and symptom resolution can take anywhere from 3 to 12 months of consistent effort. - Can gut health affect my period?
Absolutely. The estrobolome in your gut helps regulate estrogen. An imbalanced gut can contribute to hormonal imbalances, potentially leading to more severe PMS, irregular cycles, or heavier periods. - Is kombucha really good for you?
Kombucha can be a good source of probiotics, but it’s crucial to choose brands with low sugar content (under 5g per serving). For some people with gut sensitivity, the carbonation and wild yeasts can cause bloating. - Do I need both prebiotics and probiotics?
Yes, they work as a team. Probiotics add beneficial bacteria to your system, while prebiotics provide the food those bacteria need to survive and flourish. A diet rich in both is the ideal strategy. - Can a poor gut cause weight gain in women?
Yes. Gut dysbiosis can lead to increased inflammation, insulin resistance, and altered hormone signals related to hunger and satiety (like ghrelin and leptin), all of which can contribute to weight gain or difficulty losing weight. - What’s the difference between IBS and IBD?
IBS (Irritable Bowel Syndrome) is a functional disorder, meaning the gut looks normal but doesn’t function correctly. IBD (Inflammatory Bowel Disease), which includes Crohn’s and Ulcerative Colitis, is an autoimmune disease characterized by chronic inflammation and physical damage to the gut lining. - Are food sensitivity tests for leaky gut reliable?
Most commercial IgG food sensitivity tests are not considered reliable by the mainstream medical community for diagnosing leaky gut or food allergies. An elimination diet, guided by a healthcare professional, is the gold standard for identifying trigger foods. - Can gut issues cause fatigue?
Yes, through several mechanisms. Poor nutrient absorption can lead to deficiencies (like iron or B12), while chronic inflammation from gut dysbiosis places a constant, energy-draining demand on your immune system.

