Gingivitis is the mild, reversible inflammation of the gums, whereas periodontitis is a severe, destructive disease that leads to irreversible bone and tissue loss around the teeth.
Understanding this distinction is the first step toward protecting your oral and overall health.
Shockingly, severe periodontal diseases affect over a billion people globally, making it one of the most common chronic inflammatory conditions worldwide.
While gingivitis is often painless and easily overlooked, its progression to periodontitis can have devastating consequences, including tooth loss and links to systemic health issues like diabetes and heart disease.
This comprehensive guide will demystify these conditions, exploring their causes, symptoms, stages, and treatments, empowering you to take control of your gum health.
In This Article
1. What is Gum Disease? A Tale of Two Conditions
Gum disease, broadly known as periodontal disease, is an inflammatory condition affecting the tissues surrounding the teeth.
It’s not a single entity but rather a spectrum that ranges from a mild, reversible stage to a severe, destructive one.
The two main stages on this spectrum are gingivitis and periodontitis.
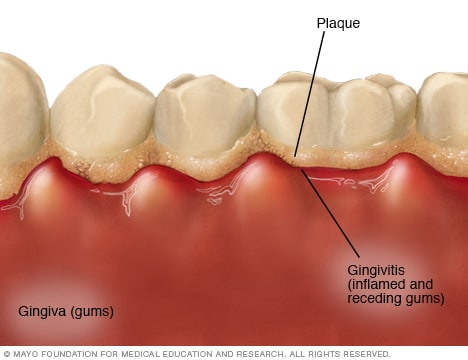
Think of gingivitis as the initial warning shot. It’s an inflammation confined to the gingiva—the part of your gum around the base of your teeth.
At this stage, the infection has not yet reached the bone and connective tissues that hold your teeth in place.
This is a critical point because, with prompt and proper care, gingivitis is entirely reversible.
However, if left untreated gingivitis can advance to periodontitis. Periodontitis is a far more serious condition.
The prefix “perio-” means around, and “-dontitis” means inflammation of the tooth.
In this advanced stage, the inflammation and infection spread below the gum line and begin to destroy the underlying bone and ligaments that support the teeth.
This damage is irreversible and, without intervention, can lead to loosening of teeth and eventual tooth loss.
According to the World Health Organization (WHO), periodontitis is a major cause of tooth loss in adults.
2. Gingivitis vs. Periodontitis: A Side-by-Side Comparison
To clarify the crucial distinctions, here is a detailed comparison between gingivitis and periodontitis.
Recognizing these differences can help you understand the severity of your symptoms and the urgency of seeking dental care.
| Feature | Gingivitis | Periodontitis |
|---|---|---|
| Definition | Mild, early-stage gum inflammation. Affects only the gingiva (gums). | Advanced, destructive gum disease. Affects gums, ligaments, and the underlying bone. |
| Main Symptoms | Red, swollen, tender gums; bleeding gums when brushing or flossing. | All symptoms of gingivitis, plus receding gums, persistent bad breath, pus between teeth, loose teeth and changes in bite. |
| Bone Loss | No bone loss occurs. The supporting structures of the teeth are still intact. | Causes progressive and irreversible loss of the alveolar bone that supports the teeth. |
| Gum Pockets | May cause “pseudo-pockets” due to swelling, but no true detachment. Probing depths are generally 1-3 mm. | Forms deep periodontal pockets (4mm or more) as gums detach from teeth, trapping more bacteria. |
| Reversibility | Completely reversible with professional cleaning and improved oral hygiene. | Irreversible damage. Treatment can halt progression and manage the disease, but lost bone and tissue do not grow back without advanced surgical procedures. |
| Treatment | Professional dental cleaning (prophylaxis) and consistent at-home care (brushing, flossing). | Deep cleaning (scaling and root planing), antibiotics and potentially surgical interventions like flap surgery or bone/tissue grafts. |
| Systemic Impact | Localized inflammation. Limited direct impact on systemic health. | Chronic inflammation is linked to increased risk for systemic diseases like diabetes, heart disease and respiratory conditions. |
3. What is Gingivitis? The Early Warning Sign
Gingivitis is the most common and mildest form of periodontal disease.
It represents the body’s initial inflammatory response to an accumulation of bacteria on the teeth.
Healthy gums are typically firm, pale pink, and fit snugly around the teeth.
When gingivitis develops, they become irritated, red and swollen.
One of the most telling signs of gingivitis is gums that bleed easily, especially during brushing or flossing.
Many people mistakenly believe that a little blood in the sink is normal, but it’s a clear indicator of active inflammation.
It’s your body’s way of signaling that something is wrong.
The good news about gingivitis is that it does not involve any loss of the bone or tissue that holds teeth in place.
The infection is superficial, limited to the soft gum tissue.
This means that with timely intervention, the condition can be completely reversed, and your gums can return to a state of perfect health without any lasting damage.
4. What Causes Gingivitis? The Role of Dental Biofilm
The primary cause of gingivitis is the buildup of dental plaque, a sticky, colorless film of bacteria that constantly forms on your teeth.
This plaque is not just a random collection of germs, it’s a highly organized community known as a biofilm.
Understanding the Biofilm
A biofilm is a complex microbial community that adheres to a surface—in this case, your teeth.
The bacteria within the biofilm work together, creating a protective slime layer that makes them more resistant to removal and to the body’s immune defenses.
According to research on bacterial biofilms, this organized structure is far more pathogenic than free-floating bacteria.
The Progression from Plaque to Gingivitis
- Plaque Formation: After you eat or drink, bacteria in your mouth feed on sugars and starches, forming the sticky plaque biofilm on your teeth, especially along the gum line. This process starts within hours.
- Plaque Hardens into Tartar: If plaque is not removed daily through brushing and flossing, it can harden into tartar (also called calculus) in as little as 24-48 hours. Tartar forms both above and below the gum line.
- Tartar Irritates the Gums: The surface of tartar is rough and porous, making it an ideal place for even more plaque to accumulate. Tartar acts as a persistent irritant to the gums, and unlike plaque, it cannot be removed with a toothbrush or floss. It requires professional removal by a dentist or hygienist.
- Inflammatory Response (Gingivitis): The toxins produced by the bacteria in the plaque and tartar trigger an inflammatory response from your immune system. This is what causes the redness, swelling, and bleeding characteristic of gingivitis. Your body is trying to fight off the bacterial invasion.
5. What Are the Symptoms of Gingivitis?
Because gingivitis can be mild, many people are unaware they have it. It’s crucial to be vigilant for the early signs.
The most common gingivitis symptoms include:
- Swollen or puffy gums: Gums may look larger than usual and lose their firm, scalloped edge around the teeth.
- Changes in gum color: Gums may change from a healthy pale pink to a dusky red or dark red.
- Bleeding gums: This is a hallmark symptom. Gums that bleed easily when you brush, floss or even eat hard foods.
- Tender or painful gums: Your gums may feel sore to the touch.
- Bad breath (halitosis): Persistent bad breath or a bad taste in the mouth that doesn’t go away after brushing can be a sign of gum infection.
Key Takeaway: Healthy gums do not bleed. If you see blood when you brush or floss, it’s a sign of active gingivitis and a signal to step up your oral hygiene and see a dentist.
6. What is Periodontitis? When Gum Disease Gets Serious
Periodontitis is what happens when gingivitis is left to smolder.
It is a chronic inflammatory disease that destroys the supporting structures of the teeth, including the periodontal ligament (the fibers that attach the tooth to the bone) and the alveolar bone (the bone socket that holds the tooth).
The transition from gingivitis to periodontitis occurs when the immune system’s response to the chronic bacterial infection goes into overdrive.
In an attempt to eliminate the bacteria, the body’s own enzymes and inflammatory cells begin to break down the very bone and connective tissue that anchor the teeth.
This creates deep spaces between the teeth and gums called periodontal pockets.
These pockets become breeding grounds for more aggressive, anaerobic (oxygen-hating) bacteria, which thrive in these deep, dark spaces.
This creates a vicious cycle: deeper pockets harbor more destructive bacteria, which cause more bone loss, leading to even deeper pockets. Unlike gingivitis, the damage caused by periodontitis is permanent.
Symptoms of Periodontitis
Periodontitis includes all the gingivitis symptoms, but with additional, more severe signs:
- Receding gums: Gums pull away from the teeth, making the teeth appear longer.
- Deep periodontal pockets: Formation of spaces between teeth and gums.
- Persistent bad breath or a foul taste: Caused by the infection deep within the pockets.
- Pus between your teeth and gums: A clear sign of a significant infection.
- Loose or shifting teeth: As bone is lost, teeth lose their support and can become mobile.
- Changes in your bite: You may notice a change in the way your teeth fit together when you bite down.
- Pain when chewing: Pressure on loose teeth or inflamed tissues can be painful.
7. The Unchecked Progression: From Healthy Gums to Periodontitis
Understanding the stages of gum disease highlights the importance of early detection and treatment.
The progression is a continuum, but it’s often categorized into distinct stages based on severity.
Stage 0: Periodontal Health
- Gums: Firm, pale pink, no swelling.
- Bleeding: No bleeding on probing by a dentist.
- Pockets: Probing depths are healthy, typically 1-3 mm.
- Bone: No bone loss.
Stage 1: Gingivitis
- Gums: Red, swollen and tender.
- Bleeding: Bleeding on probing is the key sign.
- Pockets: Probing depths may be slightly elevated (up to 4mm) due to swelling (pseudo-pockets), but there is no attachment loss.
- Bone: No bone loss.
- Reversibility: 100% reversible with treatment.
Stage 2: Early Periodontitis (Stage I Periodontitis)
This is the first stage where irreversible damage occurs.
The inflammation has started to destroy the bone.
- Bleeding: Bleeding on probing is present.
- Pockets: Probing depths increase to 4-5 mm.
- Bone Loss: The first signs of bone loss are visible on dental X-rays. The loss of attachment is 1-2 mm.
- Reversibility: The disease can be managed and its progression halted, but the lost bone will not regrow on its own.
Stage 3: Moderate Periodontitis (Stage II Periodontitis)
The destruction of bone and tissue becomes more significant.
- Bleeding: Bleeding on probing is more pronounced.
- Pockets: Probing depths deepen to 5-6 mm.
- Bone Loss: More significant bone loss is evident, potentially affecting the areas where roots of multi-rooted teeth divide (furcations). Attachment loss is 3-4 mm.
- Tooth Stability: Teeth may begin to show slight mobility.
Stage 4: Severe Periodontitis (Stage III & IV Periodontitis)
This is the most advanced stage, with extensive damage and a high risk of tooth loss.
- Pockets: Probing depths are 7 mm or greater.
- Bone Loss: More than 50% of the supporting bone has been destroyed.
- Tooth Stability: Teeth are noticeably loose, may shift position, and can be painful.
- Other Signs: Significant gum recession and pus are common. Tooth loss is highly probable without aggressive treatment.
“Periodontitis is a ‘silent’ disease in its early stages. By the time symptoms like loose teeth appear, significant and irreversible damage has already been done. This is why regular dental check-ups are not just for cleaning teeth—they are for saving them.”
8. Who is at Risk for Gum Disease?
While plaque biofilm is the direct cause of gingivitis, several factors can increase your risk of developing and progressing to periodontitis.
These risk factors can weaken your immune response or create a more favorable environment for harmful bacteria.
- Poor Oral Hygiene: The single most significant risk factor. Inconsistent brushing and flossing allow plaque to thrive.
- Smoking and Tobacco Use: A major risk factor. Smoking impairs your immune system’s ability to fight off gum infection, hinders healing, and masks early symptoms like bleeding. Smokers are several times more likely to develop periodontitis than non-smokers.
- Genetics: Some individuals are genetically more susceptible to gum disease, regardless of their oral hygiene habits.
- Diabetes: The link between diabetes and periodontitis is a two-way street. Uncontrolled blood sugar levels make gum infections more severe, and active gum disease can make it harder to control blood sugar.
- Hormonal Changes: Fluctuations in hormones during puberty, pregnancy, and menopause can make gums more sensitive and prone to gingivitis.
- Stress: Chronic stress can weaken the immune system, making it harder for your body to fight off infection.
- Poor Nutrition: A diet lacking in essential nutrients, especially Vitamin C, can compromise gum health.
- Certain Medications: Some drugs, including certain anti-seizure medications, calcium channel blockers for heart conditions, and immunosuppressants, can cause gum overgrowth, making them harder to clean.
- Crooked Teeth: Misaligned teeth create more areas for plaque to hide and are more difficult to clean effectively.
- Weakened Immune System: Conditions like HIV/AIDS or treatments like chemotherapy compromise the body’s ability to defend against infection.
9. How Do Dentists Diagnose Gum Disease?
A comprehensive periodontal examination is essential for diagnosing gingivitis and periodontitis.
Your dentist or hygienist will perform several checks:
- Medical History Review: Your dentist will ask about your symptoms, habits (like smoking) and any medical conditions or medications that could be risk factors.
- Visual Examination: They will look for visible signs of inflammation, such as redness, swelling and gum recession.
- Periodontal Probing: This is the most critical step. A small dental instrument called a periodontal probe, which is essentially a tiny ruler, is gently inserted into the space between your tooth and gum (the sulcus). This measures the depth of the pocket.
- 1-3 mm: Generally considered healthy.
- 4-5 mm: May indicate early periodontitis.
- 6 mm or more: Indicates moderate to advanced periodontitis.
- Checking for Bleeding: The dentist will note any sites that bleed during probing. Bleeding on probing (BOP) is a key indicator of active inflammation.
- Dental X-rays: X-rays are crucial for diagnosing periodontitis. They allow the dentist to see what’s happening below the gum line and assess the level of the bone that supports the teeth. X-rays can reveal the extent of bone loss that has already occurred.
10. How Are Gingivitis and Periodontitis Treated?
Treatment for gum disease depends entirely on its stage.
The goal for gingivitis is reversal, while the goal for periodontitis is to halt its progression and manage the condition to prevent further damage.
How to Treat Gingivitis
Since gingivitis is a superficial infection with no bone loss, its treatment is straightforward and highly effective.
It focuses on removing the cause—the plaque and tartar.
- Professional Dental Cleaning (Prophylaxis): A dentist or dental hygienist will remove all plaque and tartar from your teeth. This gives your gums a clean slate to heal.
- Improved At-Home Oral Hygiene: This is the most critical part of treating and preventing the recurrence of gingivitis.
- Brushing: Brush your teeth for two minutes, twice a day, with a fluoride toothpaste. Pay special attention to the gum line.
- Flossing: Floss at least once a day to remove plaque from between your teeth and under the gum line, where a toothbrush can’t reach.
- Antiseptic Mouthwash: Your dentist may recommend a therapeutic mouthwash containing ingredients like chlorhexidine for a short period to help control bacteria.
How to Treat Periodontitis
Treating periodontitis is more complex because it involves managing an infection deep below the gum line and dealing with irreversible damage. Treatment is typically phased.
Phase 1: Non-Surgical Treatment
The initial goal is to thoroughly clean the periodontal pockets and remove the bacterial biofilm.
This is often called “deep cleaning”.
- Scaling and Root Planing (SRP): This is the cornerstone of periodontitis treatment.
- Scaling: The process of removing tartar and plaque from the tooth surfaces both above and below the gum line.
- Root Planing: The process of smoothing the tooth roots to help the gums reattach to the teeth and to make it more difficult for plaque to accumulate again.
- Antibiotics: In some cases, antibiotics may be used to help control the infection. These can be administered systemically (oral pills) or placed directly into the periodontal pockets (e.g., antibiotic microspheres or chips) to deliver a high concentration of medication right where it’s needed.
Phase 2: Surgical Treatment
If deep pockets and bone loss persist after non-surgical therapy, surgery may be required to gain access for cleaning, reduce pocket depth and regenerate lost tissue.
- Flap Surgery (Pocket Reduction Surgery): The gums are lifted back to allow for thorough removal of tartar from deep pockets. The underlying bone may be reshaped before the gums are sutured back into a position that fits more snugly around the tooth, reducing pocket depth.
- Bone Grafts: If significant bone has been lost, a graft may be performed to stimulate new bone growth. The grafting material can be from your own body, a donor, or a synthetic material.
- Soft Tissue Grafts: Used to cover exposed roots caused by gum recession. Tissue is typically taken from the roof of your mouth and stitched into place to cover the recession, reducing sensitivity and protecting the root from decay.
- Guided Tissue Regeneration (GTR): A procedure that stimulates bone and gum tissue growth. A small, mesh-like membrane is placed between the bone and gum tissue, preventing the gum tissue from growing into the area where bone should be, allowing the bone and connective tissue to regrow.
Phase 3: Maintenance Therapy
Periodontitis is a chronic disease, much like diabetes. It can be controlled, but not cured.
After active treatment, ongoing maintenance is crucial to prevent recurrence.
- Periodontal Maintenance Cleanings: These are not regular cleanings. They are performed more frequently (typically every 3-4 months) and involve cleaning deep into the pockets to continually disrupt the bacterial biofilm and prevent the disease from reactivating.
11. The Mouth-Body Connection: How Gum Disease Affects Overall Health
The impact of periodontitis extends far beyond the mouth.
The mouth is a gateway to the rest of the body, and the chronic inflammation and bacteria associated with severe gum disease can have serious systemic consequences.
This field of study is known as periodontal medicine.
Research published in journals like the Journal of the American Heart Association has established strong links between periodontitis and several systemic conditions.
How does the connection work?
There are two primary mechanisms:
- Bacterial Spread: The ulcerated lining of deep periodontal pockets provides a direct entry point for harmful oral bacteria to enter the bloodstream. These bacteria can travel to other parts of the body, such as the heart and lungs and contribute to new infections or inflammation.
- Chronic Inflammation: Periodontitis creates a state of chronic, low-grade inflammation. The inflammatory proteins (like C-reactive protein) produced in the gums enter the bloodstream and circulate throughout the body, contributing to systemic inflammation, which is a known risk factor for many chronic diseases.
Key Systemic Links
- Cardiovascular Disease: People with periodontitis have a higher risk of heart attack, stroke, and atherosclerosis (hardening of the arteries). The inflammation and bacteria from gum disease are thought to contribute to the formation of arterial plaques.
- Diabetes: The relationship is bidirectional. Periodontitis makes it harder for diabetic patients to control their blood sugar, and high blood sugar makes gum disease worse. Treating periodontitis can improve glycemic control.
- Respiratory Disease: Bacteria from the mouth can be inhaled into the lungs, potentially causing or worsening conditions like pneumonia and chronic obstructive pulmonary disease (COPD).
- Pregnancy Complications: Pregnant women with periodontitis may have an increased risk of delivering preterm, low-birth-weight babies.
- Rheumatoid Arthritis: Both are chronic inflammatory diseases. Evidence suggests that the bacteria responsible for periodontitis can worsen the severity of rheumatoid arthritis.
- Dementia and Alzheimer’s Disease: Emerging research is exploring a link between the bacteria Porphyromonas gingivalis, a key pathogen in periodontitis, and the development of Alzheimer’s disease.
12. How Can You Prevent Gum Disease?
The best way to deal with gum disease is to prevent it from ever starting.
Prevention is simple, effective, and entirely in your hands.
It revolves around one central theme: controlling dental plaque.
The Cornerstones of Prevention
- Brush Thoroughly and Correctly: Brush for two minutes, twice a day. Use a soft-bristled toothbrush and fluoride toothpaste. Angle the brush at 45 degrees toward the gum line and use gentle, circular motions. Don’t forget to brush the chewing surfaces and the inside surfaces of your teeth.
- Floss Daily—No Excuses: Flossing is not optional. It’s the only way to remove plaque from between your teeth and under the gum line. If you find flossing difficult, consider using floss holders, interdental brushes, or a water flosser as a supplement (but not a replacement) to traditional floss.
- Regular Dental Visits: See your dentist and hygienist for regular check-ups and professional cleanings, typically every 6 to 12 months. Even with perfect home care, some tartar will likely form, and only a professional can remove it. If you have risk factors, you may need more frequent cleanings.
- Eat a Balanced Diet: A diet rich in vitamins and minerals (especially vitamin C) and low in sugar and starches supports gum health. Crunchy fruits and vegetables can also help clean teeth.
- Don’t Smoke: If you smoke, quitting is one of the best things you can do for your gums and your overall health.
- Manage Systemic Health: If you have diabetes or other chronic conditions, work with your physician to keep them well-managed.
Frequently Asked Questions (FAQ)
1. Can gingivitis go away on its own?
No, gingivitis will not go away on its own. It requires the removal of plaque and tartar buildup through diligent brushing, flossing and a professional dental cleaning. Without intervention, it will persist and likely worsen into periodontitis.
2. Is gum disease contagious?
The bacteria that cause gum disease can be passed through saliva. While you can’t “catch” periodontitis like a cold, sharing utensils or kissing can transfer the bacteria. However, disease development depends more on your own oral hygiene and immune response.
3. How long does it take for gingivitis to turn into periodontitis?
There is no set timeline. For some, it can take years for others who are more susceptible due to genetics or risk factors like smoking, the progression can be much faster. This variability is why early treatment of gingivitis is so important.
4. Can you have periodontitis without having gingivitis first?
No, periodontitis is by definition a progression of untreated gingivitis. However, in some individuals, especially smokers whose bleeding is masked, the signs of gingivitis may be subtle and go unnoticed before the more severe damage of periodontitis is diagnosed.
5. Does a water flosser replace regular flossing?
A water flosser is an excellent tool for removing loose debris and reducing inflammation, but it does not effectively remove the sticky plaque biofilm that adheres to teeth. Most dentists recommend using it as a supplement to, not a replacement for, traditional string floss.
6. Can receding gums from periodontitis grow back?
No, gum tissue lost to periodontitis does not grow back on its own. However, procedures like soft tissue grafts can be performed by a periodontist to cover the exposed roots and restore the gum line.
7. What is the main difference between a regular cleaning and a deep cleaning?
A regular cleaning (prophylaxis) cleans plaque and tartar from above the gum line. A deep cleaning (scaling and root planing) is a therapeutic procedure that cleans the tooth surfaces deep below the gum line, in the periodontal pockets, to treat active periodontitis.
8. Why do my gums still bleed after I started flossing?
When you first start flossing regularly, it’s common for inflamed gums to bleed for a few days to a week. This is a sign of active gingivitis. If you are consistent, the bleeding should stop as your gums heal. If it persists for more than two weeks, see your dentist.
Conclusion
The distinction between gingivitis and periodontitis is one of the most critical concepts in oral health.
Gingivitis is a reversible warning sign, a call to action.
Periodontitis is a chronic, destructive disease with irreversible consequences for your mouth and your body.
Your daily habits are your most powerful defense.
By committing to a simple routine of brushing twice a day, flossing daily, and visiting your dentist regularly, you can effectively prevent gingivitis and halt the potential progression to periodontitis.
Never ignore the signs of gum inflammation, especially bleeding gums. They are not normal, they are a signal that your gums need help.
The journey to lifelong oral health begins with understanding.
By recognizing the difference between these two conditions and taking proactive steps, you can protect your smile and contribute positively to your overall well-being.
Your Next Step: If you have noticed any symptoms of gum disease, from bleeding gums to persistent bad breath, schedule an appointment with your dentist today. Early diagnosis and treatment are the keys to preventing irreversible damage and preserving your health.
We hope this guide has been informative. Do you have any questions or personal experiences with gum disease? Share them in the comments below to help others in the community!

