Gastroesophageal reflux disease (GERD) is a chronic digestive condition where stomach acid frequently flows back into the esophagus, the tube connecting your mouth and stomach.
This acid backwash irritates the esophageal lining, causing a range of uncomfortable symptoms.
Affecting an estimated 20% of the U.S. population, GERD is far more than occasional heartburn, it’s a persistent issue that can significantly impact daily life and lead to serious complications if left untreated.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), this condition is one of the most common reasons for visits to a gastroenterologist.
This guide will provide a comprehensive explanation of GERD, moving beyond the basics to explore its nuanced symptoms, underlying causes, and the full spectrum of modern treatment options.
You will learn to distinguish GERD from simple acid reflux, understand the diagnostic process, and discover effective strategies—from lifestyle changes to advanced medical procedures—to manage your symptoms and protect your long-term health.
Read on to gain the knowledge you need to take control of GERD.
In This Article
What Exactly is GERD?
At its core, Gastroesophageal Reflux Disease (GERD) is the chronic, more severe form of acid reflux.
While nearly everyone experiences occasional acid reflux, a diagnosis of GERD means the reflux is happening regularly—typically at least twice a week—and is causing problematic symptoms or damage to the esophagus.
It’s a formal medical diagnosis that signifies a breakdown in the body’s natural anti-reflux barrier.
Heartburn vs. Acid Reflux vs. GERD: Clearing the Confusion
These terms are often used interchangeably, but they represent different concepts.
Understanding the distinction is the first step toward proper management.
Many patients are confused by this, but the relationship is quite simple: one is a symptom, one is an event, and one is a chronic disease.
| Term | What It Is | Description | Example |
|---|---|---|---|
| Heartburn | A Symptom | The burning pain or discomfort felt in the chest, caused by stomach acid irritating the esophagus. It’s a feeling, not a condition itself. | “I ate a spicy pizza and now I have terrible heartburn.” |
| Acid Reflux | A Mechanical Event | The physical event of stomach contents (acid and food) flowing backward into the esophagus. This event may or may not cause symptoms. | “;My doctor said my acid reflux is happening even when I don’t feel heartburn.” |
| GERD | A Chronic Disease | The diagnosis given when acid reflux occurs frequently and causes significant symptoms (like heartburn) or leads to complications like esophageal inflammation. | “;Because I have acid reflux more than twice a week, my doctor diagnosed me with GERD.” |
As experts at the Cleveland Clinic explain, heartburn is a symptom of acid reflux, and GERD is the disease caused by chronic acid reflux.
The Mechanics: What Happens in Your Body During Reflux?
Your digestive system has a clever gatekeeper between the esophagus and the stomach called the lower esophageal sphincter (LES).
The LES is a ring of muscle that opens to allow food to pass into your stomach and then closes tightly to keep stomach contents from coming back up.
In individuals with GERD, the LES is often weakened or relaxes inappropriately.
This malfunction allows harsh stomach acid and digestive enzymes to splash back into the esophagus.
Unlike the stomach, the esophageal lining is not designed to withstand this acidity, leading to irritation, inflammation, and the classic symptoms of GERD.
Recognizing the Signs: What Are the Symptoms of GERD?
The experience of GERD can vary widely from person to person.
While some symptoms are classic and easily recognizable, others are more subtle and can be mistaken for other conditions.
Recognizing the full spectrum of GERD symptoms is crucial for a timely diagnosis.
Typical (Esophageal) Symptoms
These are the most common symptoms directly related to esophageal irritation:
- Heartburn: A burning sensation in the chest that can move up toward the throat. It often occurs after eating, when lying down, or when bending over.
- Regurgitation: The sensation of stomach acid or food coming back into the throat or mouth, often leaving a sour or bitter taste.
- Chest Pain: Non-cardiac chest pain can be a primary symptom of GERD. It can be sharp or burning and is often difficult to distinguish from heart-related pain. Any new or severe chest pain requires immediate medical evaluation to rule out a heart attack.
- Dysphagia: Difficulty swallowing or the feeling of food being stuck in your throat. This can be a sign of esophageal narrowing due to chronic inflammation.
Atypical (Extra-Esophageal) Symptoms and “Silent Reflux”
Sometimes, GERD manifests in ways that don’t seem related to the esophagus at all.
This is often called laryngopharyngeal reflux (LPR) or “silent reflux” because it may not cause classic heartburn.
The acid travels further up, affecting the throat, airways, and even the mouth.
Many patients visit ear, nose, and throat (ENT) specialists or pulmonologists for these symptoms, not realizing the root cause is in their stomach.
Atypical symptoms include:
- Chronic Cough: A persistent, dry cough, especially after meals or when lying down.
- Hoarseness or Laryngitis: Stomach acid can irritate the vocal cords, leading to a raspy or weak voice.
- Sore Throat or Throat Clearing: A constant need to clear the throat or a feeling of a lump in the throat (known as globus sensation).
- Worsening Asthma: Acid droplets can be inhaled into the lungs, triggering bronchospasm and making asthma symptoms worse.
- Dental Erosion: Stomach acid can wear away tooth enamel over time, leading to cavities and sensitivity.
When Should You See a Doctor?
While occasional heartburn can be managed with over-the-counter remedies, you should consult a healthcare professional if:
- You experience heartburn or other GERD symptoms two or more times per week.
- Your symptoms are severe or wake you up at night.
- Over-the-counter medications are no longer effective or you need them frequently.
- You experience any “alarm” symptoms, such as:
- Unexplained weight loss
- Difficulty or pain with swallowing (dysphagia)
- Vomiting, especially with blood
- Black, tarry stools (a sign of bleeding)
- A persistent feeling of fullness after eating small amounts of food
Uncovering the Roots: What Causes GERD?
GERD is not caused by a single factor but rather a combination of physical and lifestyle elements that compromise the anti-reflux barrier.
Understanding these causes is key to effective management.
The Role of the Lower Esophageal Sphincter (LES)
As mentioned, the primary cause of GERD is a malfunctioning LES. This can happen for several reasons:
- Weak LES Pressure: The muscle itself may be inherently weak and unable to stay tightly closed against the pressure from the stomach.
- Transient LES Relaxations (TLESRs): The LES relaxes temporarily for reasons other than swallowing (like belching), allowing reflux to occur. In people with GERD, these relaxations happen more frequently.
- Hiatal Hernia: This condition occurs when the upper part of the stomach bulges up through the diaphragm (the muscle separating the abdomen and chest). This can weaken the LES and disrupt the normal pressure barrier, making reflux much more likely.
Key Risk Factors for Developing GERD
Certain conditions and lifestyle choices significantly increase your risk of developing GERD. The Mayo Clinic identifies several key risk factors:
- Obesity: Excess weight increases pressure on the abdomen, pushing stomach contents upward and overwhelming the LES.
- Pregnancy: Hormonal changes can relax the LES, and the growing uterus puts physical pressure on the stomach.
- Smoking: Nicotine is known to relax the LES muscle and can also reduce saliva production, which helps neutralize acid.
- Delayed Stomach Emptying (Gastroparesis): When food sits in the stomach for too long, it increases the chance of reflux.
- Connective Tissue Disorders: Conditions like scleroderma can affect the smooth muscle of the esophagus, impairing its function.
Can Certain Foods and Medications Make GERD Worse?
Yes, certain substances can either relax the LES or increase stomach acid, triggering GERD symptoms.
While triggers are highly individual, common culprits include:
- Foods: Fatty or fried foods, tomato-based sauces, chocolate, mint, garlic, onions, and citrus fruits.
- Beverages: Alcohol, coffee, carbonated drinks, and tea.
- Medications: Certain asthma medications, calcium channel blockers (for high blood pressure), antihistamines, painkillers, sedatives, and antidepressants can affect the LES.
The Path to Diagnosis: How is GERD Officially Diagnosed?
Diagnosing GERD often starts with a simple conversation, but confirming the diagnosis and ruling out other conditions may require more advanced testing.
The goal is to find objective evidence of reflux-related damage or excessive acid exposure.
The Initial Approach: Symptom Review and PPI Trial
For patients with classic GERD symptoms (heartburn and regurgitation) and no alarm features, doctors often recommend a diagnostic trial of a Proton Pump Inhibitor (PPI).
These medications strongly reduce stomach acid production.
If your symptoms significantly improve after an 8-week course of PPIs, a presumptive diagnosis of GERD is often made.
However, this method isn’t foolproof, as other conditions can also respond to PPIs, and not all GERD responds well to them.
When More Tests Are Needed: Upper Endoscopy
If symptoms are severe, don’t respond to treatment, or if alarm symptoms are present, your doctor will likely recommend an upper endoscopy (EGD).
During this procedure, a thin, flexible tube with a camera is passed down your throat to directly visualize the lining of your esophagus, stomach, and the first part of your small intestine.
An endoscopy can reveal:
- Esophagitis: Inflammation and visible damage to the esophagus, graded by severity.
- Esophageal Strictures: Narrowing of the esophagus from scar tissue.
- Barrett’s Esophagus: Precancerous changes in the esophageal lining.
- Hiatal Hernia: The physical protrusion of the stomach through the diaphragm.
The Gold Standard: Ambulatory Reflux Monitoring
When endoscopy is normal but GERD is still suspected, the definitive test is ambulatory reflux monitoring.
This test measures the actual amount of acid refluxing into your esophagus over a 24- to 96-hour period.
According to the latest international guidelines, known as the Lyon Consensus 2.0, conclusive evidence of GERD is an Acid Exposure Time (AET) greater than 6%. This means stomach acid is present in the esophagus for more than 6% of the monitoring period.
This test is typically done in one of two ways:
- Catheter-based Test: A thin tube is passed through the nose into the esophagus for 24 hours.
- Wireless Capsule Test (Bravo™): A small capsule is temporarily attached to the esophageal wall during an endoscopy and transmits pH data wirelessly for 48-96 hours before detaching and passing naturally.
Comprehensive Treatment: How Can You Manage GERD?
GERD treatment is a stepwise process that begins with lifestyle changes and can progress to medications and even surgery.
The goal is to control symptoms, heal the esophagus, and prevent complications.
Foundational Changes: Diet and Lifestyle Modifications
For many, these changes are enough to control mild GERD symptoms and are a crucial component of any treatment plan.
- Weight Loss: If you are overweight, losing even a small amount of weight can dramatically reduce abdominal pressure and reflux.
- Dietary Adjustments: Avoid your personal trigger foods. Eating smaller, more frequent meals is better than three large ones.
- Meal Timing: Stop eating at least 2-3 hours before lying down to give your stomach time to empty.
- Elevate the Head of Your Bed: Use blocks to raise the head of your bed by 6-8 inches or use a wedge pillow. This lets gravity help keep stomach acid down.
- Sleep Position: Sleeping on your left side can reduce reflux episodes.
- Avoid Tight Clothing: Tight belts or waistbands can constrict the abdomen and worsen reflux.
- Quit Smoking and Limit Alcohol: Both are known to worsen GERD.
Over-the-Counter (OTC) Medications
For occasional symptoms, several OTC options are available:
- Antacids (Tums, Rolaids): Neutralize stomach acid for quick, short-term relief.
- H2-Receptor Blockers (Pepcid AC, Tagamet HB): Reduce acid production. They work more slowly than antacids but provide longer relief.
Prescription Medications: PPIs and Beyond
For frequent and severe GERD, stronger medications are needed.
- Proton Pump Inhibitors (PPIs): These are the most effective drugs for reducing stomach acid and healing the esophagus. Examples include omeprazole, esomeprazole, and lansoprazole. They are available in both OTC and prescription strengths.
- Potassium-Competitive Acid Blockers (PCABs): A newer class of drugs that offer faster and more sustained acid control than PPIs. Recent studies from 2025 show high efficacy for drugs like Tegoprazan, which may become a first-line treatment for severe GERD.
When Medication Isn’t Enough: Surgical and Endoscopic Options
Surgery is considered for patients who don’t respond to medication, wish to avoid long-term drug use, or have a large hiatal hernia.
- Laparoscopic Nissen Fundoplication: The gold-standard surgical procedure where the top of the stomach is wrapped around the lower esophagus to reinforce the LES.
- Transoral Incisionless Fundoplication (TIF): A less invasive procedure performed through the mouth with an endoscope to create a partial wrap.
- Magnetic Sphincter Augmentation (LINX): A ring of magnetic beads is placed around the outside of the lower esophagus. The magnetic attraction keeps the sphincter closed but is weak enough to allow food to pass through.
Long-Term Outlook: What Are the Complications of Untreated GERD?
Ignoring chronic GERD can lead to serious and sometimes life-threatening health problems.
The constant exposure to stomach acid damages the delicate tissues of the esophagus.
Esophagitis and Esophageal Strictures
Esophagitis is the inflammation of the esophagus, which can cause pain, bleeding, and ulcers.
If this inflammation persists, it can lead to the formation of scar tissue.
This scarring can cause the esophagus to narrow, a condition known as an esophageal stricture, which makes swallowing difficult.
Barrett’s Esophagus: The Precancerous Risk
Over time, in some individuals, the cells lining the lower esophagus can change to become more like the cells lining the intestine.
This condition is called Barrett’s Esophagus.
It is the most significant risk factor for developing esophageal adenocarcinoma, a type of cancer.
While the overall risk is low, patients with Barrett’s Esophagus require regular endoscopic surveillance to monitor for precancerous changes (dysplasia).
According to Cleveland Clinic, while the cancer risk is low, early detection is key to successful treatment.
The Link to Esophageal Cancer
While the vast majority of people with GERD will never develop cancer, chronic, untreated GERD is a primary risk factor for esophageal adenocarcinoma.
The risk is highest in those who develop Barrett’;s Esophagus.
This underscores the importance of seeking treatment for persistent GERD symptoms to heal the esophagus and reduce long-term risk.
Global Prevalence of GERD
GERD is a global health issue, but its prevalence varies significantly by region, often correlating with Western diets and lifestyles.
The chart below illustrates the estimated prevalence of GERD symptoms in different parts of the world, highlighting its high incidence in North America.
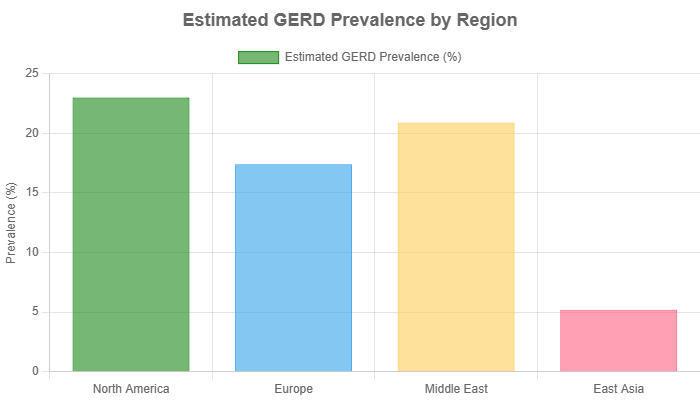
Data sourced from a systematic review published in the Journal of Neurogastroenterology and Motility. Chart displays mid-point estimates for clarity.
Frequently Asked Questions (FAQ)
1. Can GERD be cured permanently?
GERD is a chronic condition that can be managed, but not typically “cured.” Lifestyle changes and medications can control symptoms effectively, and surgery can provide long-term relief for many, but the underlying tendency for reflux may remain.
2. What is the best position to sleep in with GERD?
Sleeping on your left side with your head elevated is best. This position uses gravity and the stomach’s anatomy to make reflux less likely. Sleeping on your back or right side can worsen symptoms.
3. Can stress and anxiety cause GERD?
While stress doesn’t directly cause GERD, it can worsen symptoms. Anxiety can increase acid production and make you more sensitive to the pain of reflux, creating a vicious cycle. Managing stress is an important part of managing GERD.
4. Is it safe to take PPIs long-term?
For patients with proven GERD and complications, the benefits of long-term PPI use generally outweigh the risks. However, you should use the lowest effective dose and discuss potential side effects and risks with your doctor. The American College of Gastroenterology guidelines support this approach.
5. Can GERD cause shortness of breath?
Yes, GERD can cause shortness of breath. This can happen if stomach acid irritates the airways (triggering bronchospasm) or if severe chest pain from reflux makes it feel difficult to take a deep breath.
6. Is a GERD diet very restrictive?
Not necessarily. A GERD diet focuses on identifying and avoiding your personal trigger foods. Common triggers include acidic, spicy, and fatty foods, but what affects one person may not affect another. It’s more about personalization than restriction.
7. How is “silent reflux” (LPR) different from classic GERD?
Silent reflux primarily causes throat and respiratory symptoms (hoarseness, chronic cough, throat clearing) without the classic symptom of heartburn. The refluxed material is often less acidic but still contains damaging enzymes like pepsin.
8. Can children get GERD?
Yes, GERD can affect people of all ages, including infants and children. In children, symptoms might include frequent vomiting, coughing, refusal to eat, and breathing problems. It requires evaluation by a pediatrician or pediatric gastroenterologist.
Conclusion
Gastroesophageal Reflux Disease (GERD) is more than just an occasional nuisance, it’s a complex, chronic condition that requires careful management.
From understanding the crucial difference between heartburn and GERD to recognizing its wide array of symptoms, knowledge is your most powerful tool.
We’ve explored how a faulty lower esophageal sphincter, influenced by factors like diet, weight, and lifestyle, lies at the heart of the problem.
Effective management is a partnership between you and your healthcare provider.
It starts with foundational lifestyle and dietary changes and may progress to highly effective medications like PPIs or even advanced surgical procedures for long-term relief.
Remember, leaving GERD untreated can lead to serious complications, including Barrett’s Esophagus and an increased risk of cancer.
If you are experiencing persistent symptoms of reflux, don’t ignore them.
Schedule an appointment with your doctor or a gastroenterologist to get an accurate diagnosis and create a personalized treatment plan.
By taking proactive steps, you can control your GERD, heal your esophagus, and significantly improve your quality of life.
We encourage you to share your experiences or questions in the comments below. Your journey could help someone else on theirs.
Reference
[1] Acid Reflux/GERD | ACG – American College of Gastroenterology
https://gi.org/topics/acid-reflux/
[2] Heartburn, Acid Reflux and GERD Differences
https://health.clevelandclinic.org/whats-the-difference-between-heartburn-acid-reflux-and-gerd
[3] Differences between heartburn and GERD – United Healthcare
https://www.uhc.com/news-articles/healthy-living/differences-between-heartburn-and-gerd
[4] Understanding Barrett’s Esophagus Diagnosis and Cancer Risk
https://castlebiosciences.com/patient-information/gastroenterology/barretts-esophagus/overview
[5] Heartburn, acid reflux or GERD? Here’s how to tell the difference.
[6] GERD Symptoms You Shouldn’t Ignore – Northwestern Medicine
https://www.nm.org/healthbeat/healthy-tips/gerd-symptoms-you-shouldnt-ignore
[7] My experience 1.5 years with GERD – Reddit
https://www.reddit.com/r/GERD/comments/13s162t/my_experience_15_years_with_gerd/
[8] Silent Reflux (Laryngopharyngeal Reflux) | Condition
https://utswmed.org/conditions-treatments/silent-reflux
[9] Heartburn & Acid Reflux | Causes, Symptoms and Treatment – Guts UK
https://gutscharity.org.uk/advice-and-information/symptoms/heartburn-and-reflux/
[10] GERD, Barrett’s Esophagus, and the Link to Esophageal Cancer
[11] Acid Reflux & GERD: Symptoms, What It Is, Causes, Treatment
https://my.clevelandclinic.org/health/diseases/17019-acid-reflux-gerd

