If you’re one of the millions of people worldwide living with Irritable Bowel Syndrome (IBS), you know the frustration of unpredictable symptoms like bloating, gas, abdominal pain, and erratic bowel habits.
The low-FODMAP diet is a scientifically-backed, three-phase dietary approach designed to help you identify specific food triggers and regain control over your digestive health.
It’s not a forever diet, but rather a powerful diagnostic tool to personalize your eating plan for long-term relief.
Research has shown this approach can be remarkably effective.
Studies published in leading medical journals indicate that between 50% and 86% of IBS patients experience a significant reduction in their symptoms after following the diet correctly.
This guide will walk you through everything you need to know—from the science behind FODMAPs to practical food lists and a step-by-step plan—to determine if this diet is the right path for you.
In This Article
What is a FODMAP, Exactly?
Before diving into the diet, it’s crucial to understand what FODMAPs are.
The term might sound complex, but the concept is straightforward.
FODMAPs are a group of short-chain carbohydrates (sugars) that are poorly absorbed in the small intestine of some people.
Breaking Down the Acronym: FODMAP
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. Let’s break that down:
- Fermentable: This means that when these carbohydrates reach your large intestine, the bacteria that live there rapidly consume (ferment) them, producing gas as a byproduct.
- Oligosaccharides: These include Fructans (found in wheat, onions, garlic) and Galacto-oligosaccharides or GOS (found in beans, lentils, and legumes).
- Disaccharides: The main culprit here is Lactose, the sugar found in milk and other dairy products.
- Monosaccharides: This refers to excess Fructose (fruit sugar), especially when it’s present in higher amounts than glucose in foods like honey, apples, and high-fructose corn syrup.
- And Polyols: These are sugar alcohols like sorbitol, mannitol, and xylitol, found naturally in some fruits and vegetables (like avocados and mushrooms) and often used as artificial sweeteners in “sugar-free” products.
How Do FODMAPs Trigger IBS Symptoms?
For individuals with a sensitive gut, FODMAPs cause a two-part problem as they travel through the digestive system:
- They Draw Water into the Intestine: Because they are poorly absorbed, FODMAPs are “osmotically active”, meaning they pull excess water into the small intestine. This can lead to feelings of pressure, cramping, and can cause diarrhea.
- They are Fermented by Gut Bacteria: When these undigested carbs reach the large intestine, the trillions of bacteria residing there have a feast. This rapid fermentation produces hydrogen and/or methane gas, leading to the painful bloating, distension, and flatulence characteristic of IBS.
In essence, for people with IBS, FODMAPs act as fast food for gut bacteria, leading to a rapid production of gas and fluid that stretches the intestinal wall and triggers pain signals.
Is the Low-FODMAP Diet Right for You?
While highly effective, the low-FODMAP diet is a specific medical intervention and isn’t necessary for everyone.
It’s designed for individuals with certain digestive conditions who haven’t found relief through simpler dietary changes.
Who Benefits Most? (IBS, SIBO, and Beyond)
The primary candidates for a low-FODMAP diet are individuals diagnosed with:
- Irritable Bowel Syndrome (IBS): This is the most common and well-researched application of the diet. It’s effective for all subtypes of IBS, including diarrhea-predominant (IBS-D), constipation-predominant (IBS-C), and mixed type (IBS-M).
- Small Intestinal Bacterial Overgrowth (SIBO): In SIBO, there is an excessive amount of bacteria in the small intestine. The low-FODMAP diet helps by “starving” these overgrown bacteria of their fuel source, reducing fermentation where it shouldn’t be happening.
- Inflammatory Bowel Disease (IBD): Some people with Crohn’s disease or ulcerative colitis in remission may experience functional gut symptoms similar to IBS. For them, a low-FODMAP diet can help manage these persistent symptoms, though it does not treat the underlying inflammation of IBD.
Key Signs a Low-FODMAP Approach Could Help
If you consistently experience the following symptoms, especially after eating, the diet might be worth discussing with your doctor:
- Chronic and painful bloating or visible abdominal distension.
- Excessive and uncomfortable gas.
- Recurrent abdominal pain or cramping that is often relieved by a bowel movement.
- Unexplained diarrhea, constipation, or an alternating pattern of both.
The Importance of a Professional Diagnosis First
This cannot be overstated: Before starting a low-FODMAP diet, it is essential to consult a doctor or gastroenterologist.
These symptoms can overlap with more serious conditions like celiac disease, IBD, or even certain cancers.
A proper medical evaluation is necessary to rule out other causes and confirm an IBS diagnosis.
Attempting the diet without a diagnosis can mask symptoms of another condition and delay proper treatment.
The 3 Phases of the Low-FODMAP Diet: A Step-by-Step Plan
The low-FODMAP diet is not a lifelong restriction.
It’s a structured, three-part learning process designed to identify your personal triggers.
As Cleveland Clinic explains, the ultimate goal is to widen your dietary options as much as possible while maintaining symptom control.
Phase 1: Elimination (2-6 Weeks)
The Goal: To calm your gut and achieve a baseline of symptom relief.
During this initial phase, you will strictly avoid all high-FODMAP foods.
This gives your digestive system a rest from fermentation and water retention, allowing inflammation and sensitivity to decrease.
It’s crucial to be diligent during this period, as “cheating” can prevent you from getting a clear result.
Most people notice a significant improvement in their symptoms within the first one to two weeks.
This phase should not last longer than six weeks, as prolonged restriction can negatively affect your gut microbiome.
Phase 2: Reintroduction (8-12 Weeks)
The Goal: To systematically identify which FODMAP groups trigger your symptoms and at what dose.
Once your symptoms have improved, you’ll begin reintroducing FODMAPs one group at a time.
This is the most critical phase for long-term success.
The process, as outlined by experts at Monash University, generally looks like this:
- Choose one FODMAP group to test (e.g., Fructose).
- Select a test food for that group (e.g., a teaspoon of honey).
- Day 1: Eat a small amount of the test food while otherwise maintaining your strict low-FODMAP diet. Monitor for symptoms.
- Day 2: If no symptoms, eat a moderate amount of the same food.
- Day 3: If still no symptoms, eat a larger, standard serving size.
- Washout Period: After testing a food (whether it caused symptoms or not), return to the strict low-FODMAP diet for 2-3 days to clear your system before testing the next FODMAP group.
This methodical process allows you to pinpoint your personal triggers.
You might discover you can tolerate lactose perfectly fine but react strongly to fructans in garlic.
Phase 3: Personalization (Long-Term)
The Goal: To create a sustainable, varied, and nutritious long-term diet based on your reintroduction findings.
This is your “modified low-FODMAP diet”.
Armed with the knowledge from Phase 2, you can now reincorporate all the foods that you tolerated well.
For foods that triggered symptoms, you’ll know to either avoid them or consume them only in small, tolerable amounts.
The aim is to have the most diverse and enjoyable diet possible without triggering debilitating symptoms.
This personalized IBS diet plan becomes your new normal.
The Ultimate Low-FODMAP Foods List (and What to Avoid)
Navigating food choices is the biggest challenge of the elimination phase.
This table provides a general guide.
For a comprehensive and continuously updated list, the Monash University FODMAP Diet App is considered the gold standard.
| Food Category | High-FODMAP (Avoid in Phase 1) | Low-FODMAP (Enjoy in Phase 1) |
|---|---|---|
| Fruits | Apples, Pears, Mangoes, Cherries, Watermelon, Peaches, Plums, High-Fructose Corn Syrup | Strawberries, Blueberries (limited), Oranges, Grapes, Kiwi, Unripe Bananas, Pineapple |
| Vegetables | Onions, Garlic, Artichokes, Asparagus, Cauliflower, Mushrooms, Leeks, Sugar Snap Peas | Carrots, Cucumbers, Bell Peppers, Eggplant, Zucchini, Potatoes, Spinach, Kale, Tomatoes |
| Grains & Cereals | Wheat, Rye, Barley (in large amounts), Breads, Pastas, Crackers made with these grains | Oats, Rice, Quinoa, Corn, Gluten-Free Bread/Pasta, Sourdough Spelt Bread (traditional) |
| Proteins | Most Legumes (beans, lentils, chickpeas), Sausages with garlic/onion, Marinated Meats | Plain Cooked Meats (beef, chicken, pork), Fish, Eggs, Tofu (firm), Tempeh |
| Dairy & Alternatives | Cow’s Milk, Soft Cheeses (ricotta, cottage cheese), Yogurt, Ice Cream | Lactose-Free Milk, Almond Milk, Hard Cheeses (cheddar, parmesan), Lactose-Free Yogurt |
| Nuts & Seeds | Cashews, Pistachios | Peanuts, Walnuts, Macadamia Nuts, Pumpkin Seeds, Sesame Seeds (in moderation) |
| Sweeteners | Honey, Agave Nectar, Sorbitol, Mannitol, Xylitol | Maple Syrup, Stevia, Table Sugar (Sucrose) |
How Effective is the Low-FODMAP Diet for IBS? The Science Speaks
The low-FODMAP diet isn’t a fad, it’s an evidence-based therapeutic approach.
A large body of scientific literature supports its use.
A systematic review and meta-analysis published in 2021 found that the diet led to a moderate-to-large reduction in overall IBS symptom severity compared to control diets.
Recent research from 2024 continues to confirm these benefits, with some studies showing that a low-FODMAP diet can also significantly reduce anxiety and depression linked to chronic digestive distress.
The data consistently shows that the diet is most effective at reducing bloating, abdominal pain, and gas.
While it can also help regulate bowel habits, the most dramatic improvements are often seen in these key areas of discomfort.
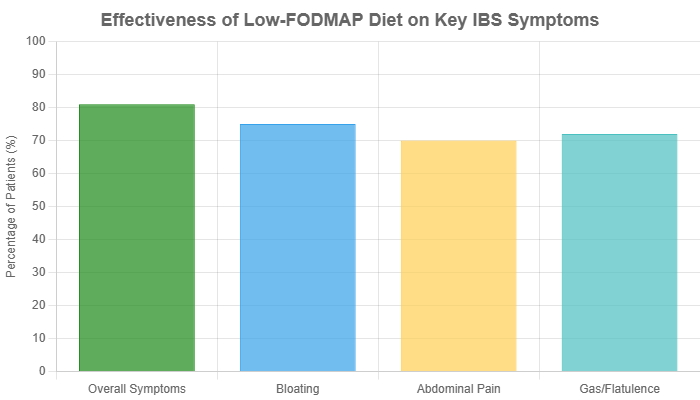
This chart illustrates the high success rate of the diet in alleviating the most burdensome symptoms of IBS, based on aggregated data from multiple clinical trials.
As a 2024 review in the journal *Nutrients* notes, success rates in the IBS population typically range from 50% to 75%, making it one of the most effective dietary strategies available.
Practical Tips for Starting and Succeeding
Embarking on the low-FODMAP diet can feel daunting.
These practical tips can make the process smoother and more successful.
Planning and Preparation is Key
Success starts before you eat your first low-FODMAP meal.
Take a weekend to plan your first week’s meals and snacks.
Go grocery shopping with your “safe” foods list in hand.
Clear your pantry and fridge of high-FODMAP temptations to make sticking to the plan easier.
Batch cooking simple meals like grilled chicken, steamed rice, and roasted carrots can save you time and stress during busy weekdays.
Reading Food Labels Like a Pro
FODMAPs hide in many processed foods.
Become a detective and scan ingredient lists for common high-FODMAP culprits. Look out for:
- High-fructose corn syrup, honey, agave
- Onion powder, garlic powder
- “Natural flavors” (can sometimes contain garlic/onion)
- Chicory root or inulin (a fructan)
- Sorbitol, mannitol, xylitol, maltitol
When in doubt, stick to whole, unprocessed foods where you control the ingredients.
Working with a Dietitian
Navigating this diet alone can be challenging and increases the risk of nutritional deficiencies.
A registered dietitian trained in the low-FODMAP diet is an invaluable resource.
They can provide personalized food lists, help you plan balanced meals, guide you through the reintroduction phase safely, and ensure you’re meeting all your nutritional needs.
Their expertise can be the difference between success and failure.
Frequently Asked Questions (FAQ)
1. How long does it take for the low-FODMAP diet to work?
Many people experience significant symptom relief within the first 1-2 weeks of the elimination phase. However, it can sometimes take up to 4 weeks to see the full benefits.
2. Can I stay on the elimination phase forever?
No, this is strongly discouraged. The elimination phase is nutritionally restrictive and can negatively impact the diversity of your beneficial gut bacteria over time. The goal is always to progress to phases 2 and 3 to liberalize your diet.
3. Is the low-FODMAP diet a weight-loss diet?
No. It is a therapeutic diet designed to manage digestive symptoms, not for weight loss. While some people may lose weight due to cutting out processed foods, it is not the intended purpose.
4. What happens if I accidentally eat a high-FODMAP food?
Don’t panic. You may experience a temporary return of your symptoms. Simply acknowledge it, let the symptoms pass, and return to the strict diet. It does not mean you have to start the entire phase over.
5. Do I need to avoid gluten on a low-FODMAP diet?
Not necessarily. Gluten is a protein, not a FODMAP. However, many gluten-containing grains like wheat, barley, and rye are also high in fructans (a FODMAP). Many people feel better on a low-FODMAP diet because they are reducing fructans, not gluten.
6. Can I drink coffee or alcohol on this diet?
Coffee (black) is generally low-FODMAP. However, caffeine can be a gut irritant for some people with IBS, independent of FODMAPs. Certain alcoholic drinks like beer and rum are high-FODMAP, while others like gin, vodka, and wine are generally low-FODMAP in small quantities.
7. Are there apps to help me follow the diet?
Yes. The Monash University FODMAP Diet app is the most reliable and comprehensive resource. It provides up-to-date food ratings, serving sizes, and other essential information directly from the researchers who developed the diet.
8. What are the risks of a low-FODMAP diet?
The main risks, if done incorrectly or for too long, are potential nutrient deficiencies (especially fiber and calcium) and a negative impact on the gut microbiome. This is why working with a dietitian and moving beyond the elimination phase is so important.
Conclusion
The low-FODMAP diet is a powerful and scientifically-validated tool for managing the often-debilitating symptoms of IBS.
It offers a structured path not just to relief, but to understanding your own body.
By methodically moving through the phases of elimination, reintroduction, and personalization, you can move away from a one-size-fits-all approach and build an IBS diet plan that is uniquely yours.
Remember, this is a journey of discovery, not deprivation.
The ultimate goal is to eat the widest variety of foods you can enjoy without fear or discomfort.
If you’re struggling with IBS, we strongly encourage you to discuss the low-FODMAP diet with your doctor or a registered dietitian to see if it’s the right next step on your path to a happier, calmer gut.

