Benign Prostatic Hyperplasia (BPH), or an enlarged prostate, is a common, non-cancerous condition where the prostate gland grows, often causing urinary issues.
It is highly treatable, and this guide will walk you through every option available in modern medicine.
The prostate’s growth is a nearly universal aspect of male aging.
According to extensive research, including data highlighted by Yale Medicine, by age 60, about half of all men experience symptoms of BPH.
By age 85, that number dramatically jumps to 90%.
This isn’t a rare affliction, it’s a predictable biological process that can significantly impact quality of life if left unmanaged.
This guide is designed to be your definitive resource.
We will demystify BPH by helping you identify its specific symptoms, understand the crucial differences between BPH and prostate cancer, and get a clear overview of the diagnostic process.
Most importantly, we will explore a comprehensive comparison of all modern treatment options—from simple lifestyle changes and medications to the latest minimally invasive procedures and gold-standard surgeries.
Continue reading to arm yourself with knowledge and find the path to relief that’s right for you.
In This Article
Part 1: What is BPH and What Does It Feel Like?
Understanding the fundamentals of BPH is the first step toward managing it.
This section establishes a clear definition of the condition, details the specific symptoms it causes, and provides crucial guidance on when it’s time to seek professional medical advice.
What is an Enlarged Prostate (BPH)?
Benign Prostatic Hyperplasia (BPH) is the medical term for a non-cancerous enlargement of the prostate gland.
The prostate is a small, walnut-sized gland in men, located just below the bladder and in front of the rectum.
Its primary function is to produce seminal fluid, which nourishes and transports sperm.
A helpful analogy is to think of the prostate as a donut.
The tube that carries urine from the bladder out of the body, the *urethra*, passes directly through the hole of this “donut”.
As a man ages, hormonal changes, primarily related to dihydrotestosterone (DHT), can cause the prostate cells to multiply, making the gland grow larger.
This growth squeezes the urethra, narrowing the passageway for urine—much like a swelling donut would shrink its hole.
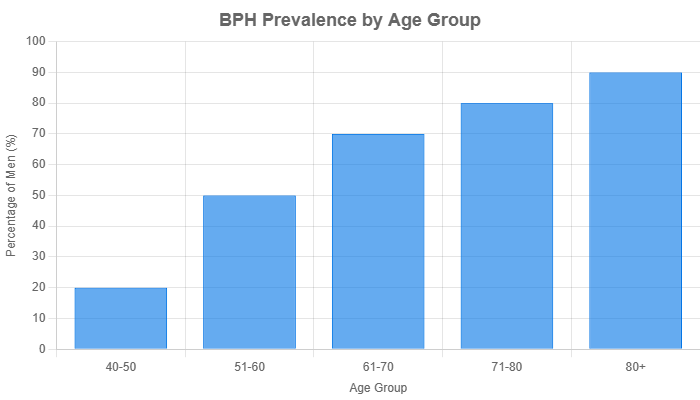
Figure 1: Estimated prevalence of symptomatic BPH increases significantly with age. Data synthesized from multiple epidemiological studies.
Crucial Distinction: BPH is NOT Prostate Cancer. One of the most common fears men have when they experience urinary symptoms is cancer. It is vital to understand that BPH is a benign condition. Having BPH does not increase your risk of developing prostate cancer. However, both conditions can exist simultaneously and may present with similar symptoms, which is why a proper medical diagnosis is essential.
The growth of the prostate is a slow, progressive process.
The size of the prostate doesn’t always correlate with the severity of the symptoms.
Some men with very large prostates have few symptoms, while others with only a slightly enlarged prostate can experience significant discomfort and disruption to their daily lives.
What Are the Common Symptoms of an Enlarged Prostate?
BPH symptoms are broadly categorized into two groups: storage symptoms (related to the bladder’s ability to hold urine) and voiding symptoms (related to the process of emptying the bladder).
Recognizing which type of symptoms you’re experiencing can help you have a more productive conversation with your doctor.
This structure is often used by urologists and is ideal for identifying issues.
Storage Symptoms (Problems Holding Urine)
These symptoms arise because the obstructed urethra causes the bladder to work harder, leading to irritation and changes in the bladder muscle itself.
- Frequency: The need to urinate more often than usual, sometimes as frequently as every one to two hours.
- Nocturia: Waking up frequently during the night to urinate. This is one of the most bothersome symptoms of BPH as it directly impacts sleep quality and overall well-being. The term for this is nocturia.
- Urgency: A sudden, compelling need to urinate that is difficult to postpone. This can lead to anxiety about being far from a restroom.
- Urge Incontinence: An involuntary leakage of urine that occurs immediately after feeling a strong urge to urinate.
Voiding Symptoms (Problems Emptying the Bladder)
These symptoms are a direct result of the physical blockage of the urethra by the enlarged prostate tissue.
- Hesitancy: Difficulty or delay in starting the urine stream, even when you feel ready to go.
- Weak or Interrupted Stream: The flow of urine is noticeably weaker than it used to be, or it stops and starts multiple times during urination.
- Straining: The need to push or bear down to begin and maintain urination.
- Dribbling: A loss of a few drops of urine at the end of urination, often after you’ve left the restroom.
- Incomplete Emptying: A persistent sensation that the bladder has not fully emptied after urinating.
When Should You See a Doctor About BPH Symptoms?
Many men delay seeking medical advice, assuming their symptoms are just a normal, unavoidable part of aging.
While BPH is common, the symptoms are treatable, and living with them is not a necessity.
Furthermore, it’s crucial to get a proper diagnosis to rule out more serious conditions.
You should schedule an appointment with your primary care provider or a urologist if your symptoms are bothersome, affect your quality of life or if you are concerned.
Even mild symptoms warrant a discussion to establish a baseline and monitor for progression over time.
“Red Flag” Symptoms: Seek Immediate Medical Attention
While most BPH symptoms develop gradually, certain signs require urgent medical evaluation. If you experience any of the following, contact a doctor right away or go to an emergency room:
- Complete Inability to Urinate (Acute Urinary Retention): This is a medical emergency. It is often accompanied by significant pain and discomfort in the lower abdomen.
- Blood in the Urine (Hematuria): While it can be caused by BPH, it can also be a sign of infection, bladder stones, or cancer and must be investigated promptly.
- Signs of a Urinary Tract Infection (UTI) or Kidney Infection: This includes fever, chills, nausea, vomiting, or burning pain during urination.
- New Onset of Bladder Pain or Discomfort.
Part 2: Getting a Definitive BPH Diagnosis
A trip to the urologist can be intimidating, especially when you don’t know what to expect.
This section demystifies the diagnostic process, explaining each step from the initial conversation to advanced testing.
Understanding this process can reduce anxiety and help you prepare for your appointment.
How Will a Doctor Diagnose BPH?
Diagnosing BPH is a systematic process designed to confirm the presence of an enlarged prostate, assess the severity of your symptoms, and, crucially, rule out other conditions with similar presentations.
The Initial Consultation: What to Expect
Your first visit will primarily involve a detailed conversation and a physical examination.
- Symptom Assessment: Your doctor will ask you to describe your urinary problems in detail. To standardize this, they will likely use the American Urological Association (AUA) Symptom Index, also known as the International Prostate Symptom Score (IPSS). This is a simple questionnaire that scores your symptoms from mild to severe, providing an objective measure of how much BPH is affecting you.
- Medical History Review: Be prepared to discuss your overall health, any other medical conditions you have (like diabetes or heart disease) and a list of all medications and supplements you take. Some medications, like certain decongestants and antidepressants, can worsen urinary symptoms.
- Physical Examination: This will include a general check-up and an examination of your abdomen. It will also almost certainly include a Digital Rectal Exam (DRE). During a DRE, the doctor inserts a gloved, lubricated finger into the rectum to feel the size, shape, and consistency of the prostate. While it may sound uncomfortable, it is a very quick (less than 30 seconds) and incredibly informative procedure that provides a direct assessment of the prostate gland.
Key Diagnostic Tests Explained
Based on your initial consultation, your doctor will likely order a few basic tests to get a clearer picture.
- Urinalysis (Urine Test): A sample of your urine is analyzed to check for signs of infection (like white blood cells) or blood (hematuria), which could indicate other problems like a UTI or bladder stones.
- PSA (Prostate-Specific Antigen) Blood Test: This is a common point of confusion and anxiety. PSA is a protein produced by prostate cells. An elevated PSA level can be a sign of prostate cancer, but it is also frequently elevated due to BPH, prostate inflammation (*prostatitis*), or even recent sexual activity or a DRE. A high PSA level is an indicator that warrants further discussion, not a diagnosis of cancer. Your doctor will interpret the result in the context of your age, prostate size, and other risk factors.
Advanced Tests for a Clearer Picture
If the diagnosis is uncertain or if your symptoms are severe, your urologist may recommend more specialized tests to gather precise data about your urinary function.
- Uroflowmetry (Urine Flow Test): You will be asked to urinate into a special funnel that measures the speed and volume of your urine stream. A slow flow rate is a strong indicator of obstruction caused by BPH.
- Post-void Residual (PVR) Test: This test measures how much urine is left in your bladder immediately after you urinate. It is usually done with a quick, non-invasive bladder ultrasound. A high PVR volume indicates that you are not emptying your bladder effectively, which can increase the risk of complications like UTIs and bladder stones.
- Transrectal Ultrasound: Similar to a DRE, a small ultrasound probe is inserted into the rectum. It uses sound waves to create a detailed image of the prostate, allowing for a very accurate measurement of its size and shape.
- Cystoscopy: In this procedure, a urologist inserts a thin, flexible tube with a camera on the end (a cystoscope) through the urethra into the bladder. This allows for a direct visual inspection of the urethra, prostate, and bladder lining, helping to identify the location and degree of blockage, as well as check for stones or tumors.
Part 3: The Complete Guide to BPH Treatment Options
This is the heart of our guide. Once a diagnosis of BPH is confirmed, the conversation shifts to treatment.
The good news is that there is a wide spectrum of effective options, ranging from simple monitoring to advanced surgery.
The best choice depends on your symptom severity, prostate size, overall health, and personal preferences.
What Are My BPH Treatment Options? A Comparative Overview
Modern BPH management follows a tiered approach.
Think of it as a ladder, where you start on the lowest rung that provides adequate relief and only move up if necessary.
- Watchful Waiting & Lifestyle Modifications: For men with mild, non-bothersome symptoms.
- Medications: The most common first-line treatment for mild to moderate symptoms.
- Minimally Invasive Surgical Therapies (MISTs): A modern middle-ground for men who don’t get enough relief from pills but want to avoid major surgery and preserve sexual function.
- Traditional & Advanced Surgery: The most definitive treatment for moderate to severe symptoms or when complications arise.
When is “Watchful Waiting” and Lifestyle Change the Best First Step?
If your IPSS score is low (typically less than 8) and your symptoms don’t significantly impact your daily life, your doctor may recommend “watchful waiting” or “active surveillance”.
This isn’t doing nothing, it’s a proactive strategy of monitoring your symptoms with regular check-ups while implementing lifestyle changes that can provide relief.
As recommended by institutions like the Mayo Clinic, these actionable changes can make a real difference:
- Fluid Management: Reduce your fluid intake in the evening, especially for 1-2 hours before bedtime, to minimize nocturia. Limit diuretics like caffeine and alcohol, which can irritate the bladder and increase urine production.
- Dietary Adjustments: Research suggests a diet rich in fruits, vegetables, and healthy fats, and low in red meat and saturated fats, may support prostate health.
- Bladder Training: Practice “timed voiding” by urinating on a set schedule (e.g., every 2-3 hours) rather than waiting for the urge. Also, try “double voiding”—after you finish urinating, wait 30-60 seconds and then try to urinate again to ensure the bladder is as empty as possible.
- Maintain a Healthy Weight: Obesity is a known risk factor for BPH and can worsen symptoms. Regular exercise can help manage weight and has been shown to reduce urinary problems.
- Avoid Certain Medications: Be mindful of over-the-counter cold and allergy medicines containing decongestants (like pseudoephedrine) or certain antihistamines, as they can tighten muscles around the urethra and make urination more difficult.
Which Medications Are Prescribed for BPH?
For men with moderate symptoms, medication is the most common starting point.
There are two primary classes of drugs used to treat BPH.
Alpha-Blockers (e.g., Tamsulosin/Flomax, Alfuzosin, Silodosin)
- How They Work: These drugs do not shrink the prostate. Instead, they work by relaxing the smooth muscle cells in the prostate gland and at the bladder neck. This relaxation widens the urethral channel, making it easier for urine to flow.
- Effectiveness: They work relatively quickly, often providing symptom relief within days to a week. They are most effective for men with small to moderately sized prostates.
- Common Side Effects: The most common side effects include dizziness or lightheadedness (especially when standing up), headache, and a stuffy nose. A notable side effect for many men is retrograde ejaculation, where semen travels backward into the bladder during orgasm instead of out the penis. This is harmless but can be a concern for men who wish to father children.
5-Alpha Reductase Inhibitors (e.g., Finasteride/Proscar, Dutasteride/Avodart)
- How They Work: These medications work by blocking the conversion of testosterone to dihydrotestosterone (DHT), the primary hormone responsible for prostate growth. By reducing DHT levels, they can actually shrink the size of the prostate gland over time.
- Effectiveness: These drugs are slow-acting. It can take up to six months or even a year to see the full benefit. They are most effective for men with significantly enlarged prostates (typically > 40 grams). They have also been shown to reduce the long-term risk of acute urinary retention and the need for future surgery.
- Common Side Effects: Because they alter hormone levels, potential side effects can include decreased libido (sex drive), erectile dysfunction (ED), and a reduction in the volume of ejaculate. These side effects are not universal but should be discussed with your doctor.
Combination Drug Therapy
For men with large prostates and significant symptoms, urologists often prescribe an alpha-blocker and a 5-alpha reductase inhibitor together.
The alpha-blocker provides rapid symptom relief while the 5-ARI works in the background to shrink the prostate for long-term control.
A common combination is Jalyn (dutasteride and tamsulosin).
What Are the Latest Minimally Invasive BPH Treatments?
The last decade has seen a revolution in BPH treatment with the rise of Minimally Invasive Surgical Therapies (MISTs).
These office-based or outpatient procedures offer a compelling middle ground, providing more significant and durable relief than medication without the recovery time and side effect profile of traditional surgery.
A key advantage for many of these procedures is the high likelihood of preserving normal ejaculatory function.
Prostatic Urethral Lift (UroLift®)
Think of this as a “tie-back” procedure for the prostate.
The urologist inserts a delivery device through the urethra and places tiny, permanent implants that pull the encroaching prostate lobes apart, like holding open a curtain.
This mechanically opens the urethra.
It’s a quick procedure with a rapid recovery and has a very low risk of causing new, sustained erectile or ejaculatory dysfunction.
It is best suited for men with prostates of a certain size (30-80g) and shape (without a large obstructive middle lobe).
Water Vapor Thermal Therapy (Rezūm™)
This procedure uses the natural energy stored in sterile water vapor (steam) to treat the excess prostate tissue.
A device is inserted into the urethra, and a small needle deploys into the prostate tissue, delivering targeted nine-second bursts of steam.
The steam condenses into water, releasing thermal energy that gently and precisely kills the targeted cells.
The body’s natural healing process then absorbs the dead tissue over several weeks, causing the prostate to shrink.
It is effective for a range of prostate sizes and also has a low risk of sexual side effects.
Robotic Waterjet Treatment (Aquablation®)
This is a more advanced, robotically-assisted procedure.
It combines real-time ultrasound imaging with a cystoscope, allowing the surgeon to map out the exact portion of the prostate to be removed.
A robotically controlled, heat-free waterjet then precisely removes the targeted tissue.
The robotic precision aims to remove obstructive tissue while avoiding structures critical for sexual function and continence.
It can be used for a wide range of prostate sizes and offers results comparable to TURP with a potentially better safety profile regarding sexual function.
Prostate Artery Embolization (PAE)
Performed by an interventional radiologist, not a urologist, PAE is a unique approach.
The radiologist threads a tiny catheter through an artery in the wrist or groin to the arteries that supply blood to the prostate.
Tiny microscopic beads are then injected to block these arteries.
Starved of its blood supply, the prostate tissue begins to shrink over weeks and months, relieving the pressure on the urethra.
It is a good option for men who are poor candidates for surgery or who have very large prostates.
What Surgical Options Exist for Severe BPH?
For men with severe symptoms, complications like urinary retention, or very large prostates, surgery remains the most effective and durable solution.
Transurethral Resection of the Prostate (TURP)
For decades, TURP has been considered the “gold standard” for BPH treatment.
The surgeon inserts an instrument called a resectoscope through the urethra.
A small, electrified wire loop at the end of the scope is used to cut away and remove the inner core of the prostate piece by piece, creating a wide-open channel.
TURP provides excellent and long-lasting symptom relief.
However, it requires anesthesia and a hospital stay, and has a very high rate of causing permanent retrograde ejaculation.
The risk of significant incontinence or erectile dysfunction is low but present.
Laser Enucleation (HoLEP/ThuLEP)
Holmium Laser Enucleation of the Prostate (HoLEP) and Thulium Laser Enucleation of the Prostate (ThuLEP) are modern, advanced alternatives to TURP.
The surgeon uses a high-powered laser to precisely separate the entire inner portion of the prostate from its outer capsule, much like peeling an orange from the inside.
The tissue is then pushed into the bladder and removed with a special device.
Laser enucleation is highly effective for any prostate size, results in very little bleeding, and often allows for a shorter hospital stay than TURP.
Like TURP, it provides excellent long-term results but also has a high rate of retrograde ejaculation.
How Do BPH Treatments Compare?
Choosing a treatment is a shared decision between you and your doctor.
This table provides a high-level comparison to help you understand the trade-offs between the most common options.
This is a critical, high-value element designed to be a reference for your medical discussions.
| Treatment | How it Works | Best For (Symptoms/Prostate Size) | Recovery Time | Impact on Ejaculation/ED | Long-Term Retreatment Rate |
|---|---|---|---|---|---|
| Watchful Waiting | Monitoring symptoms and making lifestyle changes. | Mild, non-bothersome symptoms. Any prostate size. | N/A | None. | N/A (May progress to need treatment later). |
| Alpha-Blockers (Flomax) | Relaxes prostate/bladder muscles to improve flow. Does not shrink prostate. | Mild to moderate symptoms. Best for smaller prostates. | Immediate effect, no recovery time. | High rate of retrograde ejaculation. Low risk of ED. | High. Often a bridge to a procedure. |
| 5-ARIs (Proscar) | Shrinks the prostate by blocking hormones. | Moderate to severe symptoms with a large prostate (>40g). | Takes 6+ months for full effect. | Moderate risk of decreased libido and ED. | Moderate. Reduces need for future surgery. |
| UroLift® | Implants hold prostate lobes apart, opening the urethra. | Moderate symptoms. Prostate 30-80g without obstructive middle lobe. | Minimal. Back to most activities in days. | Very low risk. Preserves ejaculatory function. | Low to moderate (~13% at 5 years). |
| Rezūm™ | Steam (water vapor) ablates excess prostate tissue. | Moderate symptoms. Prostate 30-80g. | May need catheter for a few days. Full results in 1-3 months. | Low risk. High rate of preserving ejaculatory function. | Very low (~4% at 5 years). |
| Aquablation® | Robotic, heat-free waterjet removes tissue with high precision. | Moderate to severe symptoms. Prostate 30-150g. | Overnight hospital stay. Catheter for 1-2 days. | Low risk of ED. Low rate of retrograde ejaculation (~10%). | Very low. Data is still emerging. |
| TURP | “Gold Standard”. Electrically charged loop removes tissue piece by piece. | Moderate to severe symptoms. Best for prostates < 80-100g. | Hospital stay 1-2 days. Catheter needed. 2-4 weeks recovery. | Very high rate of retrograde ejaculation (>70%). Low risk of ED. | Very low. Highly durable. |
| HoLEP/ThuLEP | Laser enucleates the entire inner prostate gland. | Moderate to severe symptoms. Effective for any prostate size, especially very large ones. | Hospital stay 1 day. Catheter needed. 1-2 weeks recovery. | Very high rate of retrograde ejaculation (>75%). Very low risk of ED. | Lowest of all procedures. Most durable. |
Part 4: Natural Remedies for BPH: What Does the Science Say?
A search for BPH treatments online will inevitably lead to a plethora of “natural” remedies, supplements, and herbs promising relief.
It’s crucial to approach these claims with a scientific and evidence-based perspective to protect both your health and your wallet.
Can Supplements or Herbs Help My BPH Symptoms?
This is a question many men ask, hoping for a solution without the side effects of prescription drugs or the invasiveness of a procedure. However, the medical consensus is clear.
In its official guidelines, the American Urological Association (AUA) states that it does not currently recommend any herbal therapies for the management of BPH. This conclusion is based on a thorough review of scientific literature, which has found a lack of strong, consistent, and high-quality evidence supporting their effectiveness.
The Truth About Saw Palmetto
Saw palmetto is by far the most popular and widely marketed supplement for prostate health.
It is an extract from the fruit of a palm tree.
For years, small studies suggested it might help with BPH symptoms.
However, more recent, larger, and better-designed clinical trials have failed to support these early findings.
A landmark study funded by the National Institutes of Health (NIH) and published in the New England Journal of Medicine concluded that saw palmetto was no more effective than a placebo (a sugar pill) in relieving BPH symptoms, even at high doses.
Other Common Supplements (Beta-sitosterol, Pygeum, Rye Grass Pollen)
Other supplements are also commonly promoted for BPH:
- Beta-sitosterol: A substance found in many plants. Some small studies have suggested it can improve urinary flow. However, as noted by Healthline’s review, the long-term safety and effectiveness are unknown.
- Pygeum: An extract from the bark of the African plum tree. Again, some older, smaller studies showed potential benefits, but the evidence is considered weak and inconsistent by modern standards.
- Rye Grass Pollen Extract: Some studies have shown it may help with nocturia, but overall evidence remains insufficient for a medical recommendation.
The Bottom Line: Talk to Your Doctor First
The supplement industry is largely unregulated.
This means you cannot be certain that the product in the bottle contains the ingredients or dosages listed on the label. Furthermore, “natural” does not mean “safe”.
Some herbal products can cause side effects or, more dangerously, interact with prescription medications you are taking (such as blood thinners).
Always tell your doctor about any supplements you are considering or currently taking.
Part 5: Life After BPH Treatment
Deciding on a treatment is a major step, but it’s equally important to understand what comes next.
This section manages expectations about the recovery process and long-term outcomes, addressing the real-world “experience” of living with the results of BPH treatment.
What is Recovery Like After a BPH Procedure?
Recovery varies significantly depending on the procedure performed.
While medications have no physical recovery period, all invasive treatments do.
The First Few Weeks
For minimally invasive procedures like UroLift or Rezūm, recovery is typically fast.
You might experience some temporary urinary symptoms like frequency, urgency, or mild burning for a week or two as the area heals.
Many men can return to non-strenuous activities within a few days.
For more extensive surgeries like TURP or HoLEP, the initial recovery is more involved.
It’s common to have a temporary urinary catheter in place for a day or two after the procedure to allow the urethra to heal.
After the catheter is removed, you can expect:
- Irritative Symptoms: It is very common to experience urinary frequency, urgency, and some burning for several weeks as the internal surgical site heals.
- Blood in the Urine: You may see some blood or small clots in your urine intermittently for a few weeks. This is normal, and your doctor will advise you to drink plenty of water to keep your urine clear.
- Activity Restrictions: You will be advised to avoid heavy lifting, straining, and strenuous exercise for several weeks to prevent bleeding.
Long-Term Adjustments and Sexual Function
The primary long-term adjustment for many men after TURP or HoLEP is retrograde ejaculation.
Because the internal sphincter of the bladder is altered during these procedures, semen takes the path of least resistance and flows backward into the bladder during orgasm.
It is then harmlessly flushed out with the next urination.
This results in a “dry” or low-volume orgasm.
It does not affect the sensation of orgasm or the ability to get an erection, but it does impact fertility.
The risk of new, long-term, significant erectile dysfunction or urinary incontinence is low with modern techniques performed by experienced surgeons.
MISTs like UroLift and Rezūm were specifically designed to minimize these risks and have a very high rate of preserving normal ejaculation.
What Are the Risks of Leaving BPH Untreated?
Ignoring moderate to severe BPH symptoms can lead to serious and sometimes irreversible complications.
The constant strain on the urinary system takes a toll.
As detailed by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), potential complications include:
- Acute Urinary Retention (AUR): A sudden and complete inability to urinate. This is a painful medical emergency requiring immediate catheterization.
- Bladder Stones: Minerals in the residual urine can crystallize and form painful stones within the bladder.
- Bladder Damage: Over time, the bladder muscle can stretch and weaken from constantly pushing against an obstruction, losing its ability to contract effectively.
- Kidney Damage: In severe, long-standing cases, the back-pressure from a full bladder can travel up to the kidneys, leading to damage and even kidney failure.
These risks underscore why BPH is more than just an inconvenience, it’s a medical condition that requires proper management.
Frequently Asked Questions (FAQ) about BPH
Here are quick, direct answers to some of the most common questions men have about BPH.
- Can BPH turn into prostate cancer?
No. BPH is a benign (non-cancerous) condition and is not a precursor to prostate cancer. Having BPH does not increase your risk of developing cancer, though both conditions can exist at the same time. - Can an enlarged prostate shrink on its own?
Generally, no. BPH is a progressive condition, and the prostate tends to continue growing slowly with age. While symptoms can sometimes fluctuate or temporarily improve with lifestyle changes, the underlying physical enlargement does not typically reverse itself without medical or surgical treatment. - What is the fastest way to shrink an enlarged prostate?
Medications like finasteride (Proscar) can shrink the prostate, but it takes 6+ months. Procedures like Rezūm, TURP, or HoLEP cause the prostate to shrink or remove tissue, with results becoming apparent over weeks to months. There is no “instant” way to shrink the gland. - Does Flomax (tamsulosin) actually shrink the prostate?
No. Flomax is an alpha-blocker. It does not change the size of the prostate. It works by relaxing the muscles around the urethra, which opens the channel and improves urine flow. The relief it provides is symptomatic, not structural. - Is BPH surgery a major operation?
It depends on the type. Minimally invasive procedures like UroLift and Rezūm are minor, often done in a doctor’s office. Traditional surgeries like TURP and HoLEP are more significant, requiring anesthesia and a hospital stay, but are still performed through the urethra without external incisions. - Can I still have a normal sex life with BPH?
Yes. BPH itself does not typically cause erectile dysfunction. Some treatments can affect sexual function (e.g., retrograde ejaculation after TURP), but many modern options are specifically designed to preserve it. Discussing this priority with your doctor is key to choosing the right treatment. - What foods should I avoid if I have an enlarged prostate?
While no food causes BPH, some can irritate the bladder and worsen symptoms. It’s often helpful to limit caffeine, alcohol, spicy foods, and artificial sweeteners. A diet high in red meat and dairy has also been linked to a higher risk of BPH progression. - How do I know if my prostate is too big?
You can’t know based on symptoms alone. A doctor determines the size through a Digital Rectal Exam (DRE) or, more accurately, with an ultrasound. Prostate size does not always correlate with symptom severity, a proper diagnosis is essential. - Is it normal to urinate 10 times a day with BPH?
For someone with symptomatic BPH, urinating 8-10 times or more during the day can be typical. This increased frequency is a hallmark symptom. “Normal” for a healthy adult is usually 4-7 times per day, depending on fluid intake. - Can exercise help BPH?
Yes. Regular, moderate exercise like brisk walking can help reduce BPH symptoms. Maintaining a healthy weight through diet and exercise is one of the most effective lifestyle strategies for managing the condition and reducing its severity.
Conclusion
Benign Prostatic Hyperplasia is a journey that a majority of men will navigate as they age.
The key takeaway from this comprehensive guide should be one of empowerment, not fear.
BPH is a highly manageable condition, and its symptoms are not something you simply have to “live with”.
We’ve established that BPH is not cancer and does not lead to it.
We’ve detailed the spectrum of symptoms, from mild annoyances to urgent red flags, and demystified the diagnostic process.
Most importantly, we’ve explored the vast landscape of modern treatments, which offers a solution for nearly every man, regardless of his symptoms, priorities, or health status.
From lifestyle adjustments and effective medications to revolutionary minimally invasive procedures that preserve sexual function and definitive gold-standard surgeries, relief is attainable.
Urinary symptoms are not a mandatory sentence of aging.
Use this guide to have an informed, confident conversation with your doctor or a urologist.
By understanding your options, you can collaboratively choose the best treatment path for your specific needs, preferences, and lifestyle, and reclaim your quality of life.
References
- American Urological Association (AUA) Guideline: Management of Benign Prostatic Hyperplasia/Lower Urinary Tract Symptoms (2021, Amended 2023).
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). “Enlarged Prostate (Benign Prostatic Hyperplasia).”
- Mayo Clinic. “Benign prostatic hyperplasia (BPH) – Symptoms and causes.”
- Yale Medicine. “Enlarged Prostate (Benign Prostatic Hyperplasia).”
- Cleveland Clinic. “Benign Prostatic Hyperplasia (BPH).”
- Harvard Health Publishing. “The growing problem of an enlarged prostate gland.”

