If you’re reading this, chances are you’re tired. Not just “end-of-a-long-day” tired, but a profound, bone-deep exhaustion that follows you from the moment you wake up.
Chronic insomnia, defined as sleep difficulties occurring at least three nights a week for over three months, is a challenging but highly treatable condition.
The key is understanding that effective long-term strategies go far beyond temporary fixes and sleeping pills.
You are far from alone in this struggle. According to a 2024 survey by the American Academy of Sleep Medicine (AASM), about 12% of American adults have been diagnosed with chronic insomnia, highlighting a widespread and often silent battle for restful nights.
This condition is more than just an inconvenience, it’s a serious health issue linked to impaired cognitive function, mood disorders and an increased risk of chronic diseases.
This guide is designed to be your definitive resource for navigating the path to recovery.
We will delve into the gold-standard treatment, Cognitive Behavioral Therapy for Insomnia (CBT-I), explore the latest advancements in long-term medications, and provide a clear framework for creating a sustainable sleep improvement plan.
If you’re ready to move past sleepless nights and reclaim your days, this comprehensive guide is your first step toward lasting change.
In This Article
What Exactly Is Chronic Insomnia?
The term “insomnia” is often used casually to describe a single bad night’s sleep.
However, in a clinical context, chronic insomnia is a specific and persistent sleep disorder with clear diagnostic criteria.
Understanding this distinction is the first step toward seeking the right help.
It’s not about being a “bad sleeper”, it’s about having a recognized medical condition.
According to the International Classification of Sleep Disorders, Third Edition (ICSD-3), the diagnostic standard used by sleep specialists worldwide, chronic insomnia is defined by the following criteria:
- Sleep Disturbance: A consistent complaint of difficulty initiating sleep, difficulty maintaining sleep (frequent awakenings), or waking up too early with an inability to return to sleep.
- Frequency: These sleep difficulties occur at least three nights per week.
- Duration: The problem has persisted for at least three months.
- Opportunity: The sleep difficulty occurs despite having an adequate opportunity and environment for sleep.
- Daytime Impairment: The lack of sleep causes significant distress or impairment in social, occupational, educational, or other important areas of functioning. This can manifest as fatigue, attention problems, mood disturbances or reduced motivation.
Acute vs. Chronic Insomnia
It’s crucial to differentiate between acute and chronic insomnia.
Acute insomnia is short-term, typically lasting from a few days to a few weeks.
It’s often triggered by a specific life event or stressor, such as an upcoming exam, a job loss, or jet lag. In many cases, acute insomnia resolves on its own once the stressor is removed or managed.
Chronic insomnia, on the other hand, is a long-term pattern. It may start as acute insomnia, but it develops a life of its own, persisting long after the initial trigger has passed.
This is because of perpetuating factors—habits and thought patterns that unintentionally maintain the sleep problem, which we will explore in the next section.
Primary vs. Comorbid Insomnia
Another important distinction is whether the insomnia is primary or comorbid.
- Primary Insomnia (or Idiopathic Insomnia) means the insomnia is the main problem and isn’t caused by another medical or psychiatric condition.
- Comorbid Insomnia means the insomnia occurs alongside another condition. This is extremely common. Conditions frequently associated with insomnia include depression, anxiety disorders, chronic pain, gastroesophageal reflux disease (GERD), and other sleep disorders like sleep apnea. In these cases, the relationship is often bidirectional: the medical condition worsens sleep, and poor sleep exacerbates the medical condition. Effective long-term treatment must address both issues simultaneously.
Why Has My Insomnia Become a Long-Term Problem?
One of the most frustrating aspects of chronic insomnia is its persistence. You might have tried everything—warm milk, counting sheep, avoiding screens—yet the problem remains.
The reason for this lies in a well-established psychological framework known as the “3-P Model of Insomnia”.
This model explains how a temporary sleep problem evolves into a chronic, self-perpetuating cycle.
The 3-P Model: Understanding the Vicious Cycle
Developed by Dr. Arthur Spielman, this model breaks down the progression of insomnia into three key factors:
- Predisposing Factors: These are the underlying vulnerabilities that make you more susceptible to developing insomnia. They don’t cause insomnia on their own but set the stage. Examples include a genetic predisposition, a personality type prone to worry or perfectionism, or being a “light sleeper”.
- Precipitating Factors: This is the initial trigger—the event that kicks off the bout of acute insomnia. It could be a major life stressor (divorce, new job), a medical illness, a change in schedule, or a traumatic event.
- Perpetuating Factors: This is the most critical component for understanding chronic insomnia. These are the thoughts and behaviors you adopt to cope with sleeplessness that, paradoxically, end up making it worse and keeping the cycle going long after the initial trigger is gone.
The Key Perpetuating Factors That Fuel Chronic Insomnia
Chronic insomnia is less about the initial cause and more about these maintaining factors.
Recognizing them is the first step to breaking the cycle.
1. Conditioned Arousal
This is a form of classical conditioning. After many nights of tossing and turning, your brain starts to associate your bed and bedroom with anxiety, frustration and wakefulness instead of rest and sleep.
The moment your head hits the pillow, your mind and body may go into “fight or flight” mode, releasing stress hormones that make sleep impossible.
The bed becomes a cue for arousal, not relaxation.
2. Maladaptive Behaviors and Habits
In a desperate attempt to get more sleep, people with insomnia often develop habits that backfire:
- Spending too much time in bed: Going to bed earlier or staying in bed later to “try” to sleep. This leads to more fragmented, light sleep and reinforces the bed-as-a-battleground association.
- Napping during the day: While a short nap can feel necessary, it can reduce your “sleep drive” at night, making it harder to fall asleep.
- Inconsistent sleep schedules: Sleeping in on weekends disrupts your internal body clock (circadian rhythm), leading to a “social jetlag” effect that makes it harder to wake up on Monday and fall asleep the following night.
- Clock-watching: Constantly checking the time increases anxiety and pressure to fall asleep, which is counterproductive.
3. Cognitive Distortions and Worry
The mental side of chronic insomnia is powerful.
Sufferers often develop unhelpful beliefs and thought patterns about sleep:
- Worrying about sleep itself: “What if I can’t fall asleep tonight?” This performance anxiety makes sleep less likely.
- Catastrophizing: Believing that a single bad night’s sleep will ruin the next day entirely (“I won’t be able to function at work tomorrow”).
- Unrealistic sleep expectations: Believing you absolutely *must* get 8 hours of sleep every night to be healthy, leading to anxiety when you fall short.
The State of Hyperarousal
Ultimately, these perpetuating factors combine to create a state of 24-hour hyperarousal.
Research shows that individuals with chronic insomnia have elevated levels of stress hormones like cortisol and increased metabolic rates, not just at night but throughout the day.
Their nervous system is stuck in a state of being “on”, making it incredibly difficult to transition to the “off” state required for sleep.
This is why chronic insomnia is considered a disorder of both night and day.
What Is the Most Effective Long-Term Treatment for Insomnia? (CBT-I Deep Dive)
When it comes to a durable, long-term solution for chronic insomnia, the scientific and medical consensus is clear.
The most effective, first-line treatment is not a pill, but a structured therapy program called Cognitive Behavioral Therapy for Insomnia (CBT-I).
Leading medical bodies, including the American College of Physicians and the AASM, recommend CBT-I as the primary treatment for all adults with chronic insomnia.
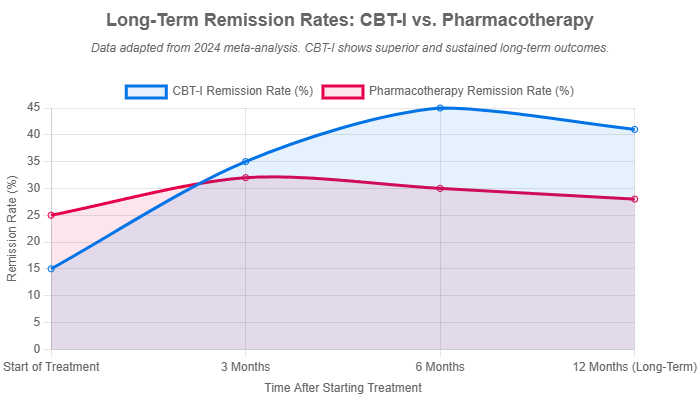
A landmark 2024 network meta-analysis published in *Psychiatry and Clinical Neurosciences* confirmed that starting with CBT-I leads to better long-term remission rates than starting with medication.
The reason is simple: CBT-I addresses the underlying causes—the perpetuating factors—of insomnia, rather than just masking the symptoms.
The Core Components of CBT-I
CBT-I is a multi-component program that systematically targets the behaviors and thoughts that interfere with sleep.
It’s typically delivered over 4-8 sessions with a trained therapist. Here are its powerful core components:
Cognitive Restructuring: Changing Your Thoughts About Sleep
This component focuses on identifying, challenging, and changing the negative thoughts and beliefs that fuel sleep-related anxiety.
A therapist helps you recognize cognitive distortions and replace them with more realistic and adaptive thoughts.
- Identifying the thought: “I only got 5 hours of sleep. Tomorrow will be a disaster. I won’t be able to function”.
- Challenging the thought: “Have I had 5 hours of sleep before? Was the day a complete disaster, or was it just difficult? What can I do to manage my day even if I’m tired?”
- Reframing the thought: “I’d prefer more sleep, but I can handle tomorrow. I will focus on one task at a time and take short breaks. It’s not ideal, but it’s manageable”.
Stimulus Control Therapy (SCT): Reconnecting Your Bed with Sleep
The goal of SCT is to break the conditioned arousal and re-establish the bed as a strong cue for sleep.
The instructions are simple but require strict adherence:
- Go to bed only when you feel sleepy. Not just tired, but sleepy.
- Use the bed only for sleep and intimacy. No reading, watching TV, working, or worrying in bed.
- If you can’t fall asleep within about 20-30 minutes, get out of bed. Go to another room and do a quiet, relaxing activity (like reading a dull book in dim light). Do not do anything stimulating.
- Return to bed only when you feel sleepy again. Repeat this step as many times as necessary throughout the night.
- Wake up at the same time every morning, regardless of how much you slept.
- Do not nap during the day.
Sleep Restriction Therapy (SRT): Consolidating Your Sleep
This may sound counterintuitive, but it’s one of the most powerful techniques. SRT aims to improve your sleep efficiency (the percentage of time in bed that you’re actually asleep).
It temporarily limits your time in bed to the average amount of time you are currently sleeping.
Case Example: If your sleep diary shows you spend 8 hours in bed but only sleep for 5.5 hours, your initial “sleep window” would be set to 5.5 hours. This mild sleep deprivation builds a powerful homeostatic sleep drive, making you fall asleep faster and sleep more deeply. As your sleep efficiency improves (to >85-90%), your time in bed is gradually increased until you reach an optimal sleep duration.
This technique is highly effective at eliminating long periods of wakefulness during the night and consolidating sleep into a single, solid block.
Relaxation Techniques: Calming the Hyperaroused Mind and Body
CBT-I also incorporates techniques to lower the physiological and cognitive arousal that prevents sleep.
These can include diaphragmatic (deep) breathing, progressive muscle relaxation, guided imagery and mindfulness meditation.
These practices help activate the body’s parasympathetic nervous system, the “rest and digest” system that is essential for sleep.
Digital CBT-I (dCBT-I): Making Treatment Accessible
A major barrier to CBT-I has been the shortage of trained therapists. Fortunately, technology has provided a solution.
Digital CBT-I (dCBT-I) delivers the full program through smartphone apps and web-based platforms.
A 2024 meta-analysis mentioned in *Nature* concluded that electronically delivered CBT-I was equally as effective as in-person therapy.
Programs like Sleepio and Somryst are even FDA-cleared, making this gold-standard treatment more accessible than ever.
Are There Long-Term Medications for Chronic Insomnia?
For decades, the prevailing wisdom was that sleeping pills were only for short-term use due to risks of tolerance, dependence and side effects.
While this caution remains valid for older classes of drugs, the landscape of pharmacological insomnia treatment is evolving.
Today, the conversation has shifted toward a more nuanced approach involving shared decision-making between patient and doctor.
A 2023 clinical appraisal highlighted this shift, noting that while older guidelines recommended limiting use to 4-5 weeks, newer medications have been studied and proven safe and effective for much longer durations.
The consensus among experts is that the appropriate duration of therapy should be individualized, especially since chronic insomnia is, by definition, a long-term condition.
Medication is rarely a standalone solution. It is most effective when used as part of a comprehensive plan, often to provide initial relief while a patient learns the long-term skills of CBT-I.
Overview of Medication Classes for Insomnia
Benzodiazepine Receptor Agonists (“Z-drugs”)
This class includes well-known drugs like zolpidem (Ambien), eszopiclone (Lunesta) and zaleplon (Sonata).
They work by enhancing the effect of GABA, a neurotransmitter that reduces brain activity.
While effective for sleep onset and maintenance, their long-term daily use is generally discouraged due to risks of:
- Tolerance: Needing higher doses over time to achieve the same effect.
- Dependence: Experiencing withdrawal symptoms if the medication is stopped abruptly.
- Next-day impairment: Grogginess, cognitive “fogginess” and impaired driving ability.
- Complex sleep behaviors: Rare but serious side effects like sleep-walking, sleep-driving or sleep-eating.
Eszopiclone is one Z-drug that has been approved for longer-term use, but the risks still warrant careful consideration.
Dual Orexin Receptor Antagonists (DORAs)
This is the newest class of insomnia medication and represents a significant advancement for long-term treatment.
Drugs in this class include suvorexant (Belsomra), lemborexant (Dayvigo) and daridorexant (Quviviq).
Unlike Z-drugs that sedate the brain, DORAs work by blocking the activity of orexin, a chemical messenger in the brain that promotes wakefulness.
This more targeted approach offers several advantages for long-term use, which we will detail in the next section.
Low-Dose Antidepressants
Certain antidepressants are prescribed “off-label” for insomnia due to their sedating side effects.
The most common is doxepin, which is FDA-approved at very low doses (3-6 mg) specifically for sleep maintenance.
Others like trazodone and mirtazapine are also used.
They can be a good option for patients who have both depression and insomnia, but their side effect profile (including daytime sleepiness and weight gain) must be managed.
How Do New Insomnia Medications (DORAs) Differ from Older Sleeping Pills?
The arrival of Dual Orexin Receptor Antagonists (DORAs) marked a paradigm shift in the pharmacological management of insomnia.
Their unique mechanism of action directly addresses the hyperarousal state of insomnia, making them a fundamentally different and often safer long-term option compared to traditional sedative-hypnotics like the Z-drugs.
A Tale of Two Mechanisms: Turning Down vs. Turning Off
The core difference lies in how these drugs interact with the brain’s sleep-wake circuitry.
- Older Sedative-Hypnotics (Z-drugs): These drugs act like a dimmer switch for the entire brain. They enhance the activity of the neurotransmitter GABA, which is the brain’s primary “brake”. This broadly reduces neuronal activity, inducing a state of sedation. The goal is to force sleep by slowing the brain down.
- DORAs: These drugs act like a targeted “off” switch for the brain’s wakefulness system. They specifically block orexin, a key neurotransmitter that acts as the brain’s “gas pedal”, promoting alertness and arousal. By preventing orexin from binding to its receptors, DORAs quiet the “wake drive”, allowing the brain’s natural sleep processes to take over.
As one researcher in the *Nature* article aptly put it, this approach is like making someone “narcoleptic for one night”—turning off the wake signal rather than inducing an artificial sedative state.
Comparative Table: Z-Drugs vs. DORAs
This table provides a clear, at-a-glance comparison, making it an ideal resource for understanding your options.
| Feature | Sedative-Hypnotics (e.g., Zolpidem) | DORAs (e.g., Daridorexant) |
|---|---|---|
| Mechanism | Enhances GABA to broadly reduce brain activity (sedation). | Blocks orexin to specifically suppress wakefulness signals. |
| Long-Term Use | Generally not recommended for daily use due to tolerance/dependence risks. | Studied and approved for long-term, daily use. |
| Risk of Dependence | Higher risk of physical and psychological dependence. | Lower risk reported in clinical trials. |
| Next-Day Effects | Can cause significant grogginess, memory issues, and impaired coordination. | Designed to have minimal next-day residual effects due to shorter half-lives. |
| Primary Goal | Induce sedation. | Quiet the “wake drive” and permit natural sleep. |
| Rebound Insomnia | Common upon discontinuation (sleep can become worse than before). | Less common or absent in studies. |
What Role Do Natural Remedies and Sleep Hygiene Play?
In the quest for better sleep, many people first turn to natural remedies and lists of “sleep hygiene” tips.
While these strategies can be beneficial, it’s critical to understand their proper role in managing a complex condition like chronic insomnia.
For long-term sufferers, they are best viewed as supportive components of a comprehensive plan, not standalone cures.
Sleep Hygiene: A Necessary Foundation, Not a Cure
Sleep hygiene refers to a set of habits and environmental factors that are conducive to good sleep. These include:
- Maintaining a consistent sleep-wake schedule, even on weekends.
- Ensuring your bedroom is cool, dark and quiet.
- Avoiding large meals, caffeine, and alcohol close to bedtime.
- Getting regular exercise, but not too close to bedtime.
- Avoiding stimulating activities and screen time before bed.
For someone with mild or acute insomnia, improving sleep hygiene can sometimes be enough.
However, for chronic insomnia, it is almost always insufficient on its own.
The perpetuating factors of conditioned arousal and sleep-related anxiety are too powerful to be overcome by a dark room alone.
Think of sleep hygiene as the foundation of a house: you absolutely need it, but it’s not the whole house.
It’s an essential part of a CBT-I program, but not a substitute for it.
An Evidence-Based Look at Natural Remedies
The market for natural sleep aids is vast, but the scientific evidence is often mixed or weak.
It’s important to approach them with a critical eye.
Melatonin
Melatonin is a hormone your brain produces in response to darkness, helping to regulate your circadian rhythm.
While it’s often marketed as a sleep aid, its role is more about timing than inducing sleep.
The AASM clinical practice guidelines explicitly recommend *against* using melatonin to treat chronic insomnia in adults due to a lack of strong evidence for its effectiveness.
It can be useful for circadian rhythm disorders like jet lag or delayed sleep phase disorder, but it does not typically resolve the core issues of chronic insomnia.
Valerian Root, Chamomile and Lavender
These are among the most popular herbal remedies for sleep.
- Valerian Root: Some studies suggest it may have mild sedative effects and can improve sleep quality for some, but results are inconsistent.
- Chamomile: Often consumed as a tea, it contains an antioxidant called apigenin that may promote sleepiness by binding to certain brain receptors. Research is limited but suggests a modest benefit.
- Lavender: Used in aromatherapy, the scent of lavender has been shown to have calming effects that can help reduce anxiety and promote relaxation before bed.
While these remedies may help you relax, they are not considered reliable treatments for chronic insomnia.
Their effect is generally mild and not comparable to evidence-based therapies like CBT-I.
Important Disclaimer: “Natural” does not always mean “safe”. Supplements are not regulated by the FDA in the same way as medications, and they can have variable purity and potency. They can also interact with other medications. Always consult your doctor before starting any new supplement for your insomnia.
How Can I Manage Insomnia With Other Health Conditions?
Chronic insomnia rarely exists in a vacuum.
It is frequently intertwined with other medical and psychiatric conditions, a phenomenon known as comorbidity.
In fact, research suggests that 40-50% of individuals with insomnia have a comorbid mental health condition.
Successfully managing long-term insomnia requires addressing these co-occurring issues head-on.
The Bidirectional Relationship: A Vicious Cycle
The link between insomnia and other conditions is often a two-way street. Poor sleep can worsen the symptoms of a co-occurring disorder, and that disorder, in turn, can disrupt sleep.
This creates a vicious cycle that can be difficult to break.
- Depression and Anxiety: These are the most common psychiatric comorbidities. Over 90% of patients with depression report sleep problems. Worry and rumination from anxiety make it hard to fall asleep, while the fatigue and hopelessness from insomnia can trigger or worsen depression.
- Chronic Pain: Pain makes it difficult to find a comfortable position and can cause awakenings. Simultaneously, sleep deprivation lowers the pain threshold and amplifies the perception of pain, making it feel more intense.
- Post-Traumatic Stress Disorder (PTSD): Nightmares and hypervigilance, hallmarks of PTSD, are profoundly disruptive to sleep. The resulting sleep deprivation can then impair emotional regulation, making PTSD symptoms harder to manage during the day.
Why Integrated Treatment is the Key to Success
Treating only one side of the equation is often ineffective.
For example, taking an antidepressant might improve mood but may not fully resolve the entrenched habits and anxieties of chronic insomnia.
The most effective approach is an integrated one that treats both conditions simultaneously.
This is another area where CBT-I shines. Studies have consistently shown that CBT-I is not only effective for sleep in patients with comorbid conditions, but it can also lead to significant improvements in the symptoms of the co-occurring disorder itself.
By improving sleep, CBT-I can enhance emotional resilience, reduce pain perception, and improve overall quality of life, creating a positive upward spiral.
Medication Considerations in Comorbid Insomnia
When medication is considered, the presence of a comorbid condition adds a layer of complexity.
A doctor must carefully select a medication that will not worsen the other condition. For instance:
- For a patient with both depression and insomnia, a sedating antidepressant like low-dose doxepin or mirtazapine might be a logical choice to address both issues with a single medication.
- A doctor must be cautious about potential drug interactions. For example, some medications for pain or anxiety can have their own sedative effects, which could lead to excessive daytime sleepiness when combined with a sleep aid.
This highlights the absolute necessity of a thorough medical evaluation and ongoing management by a healthcare professional who understands the complex interplay between sleep and other health conditions.
How Do I Create a Personalized Long-Term Treatment Plan?
Overcoming chronic insomnia is a journey, not a quick fix.
It requires a structured, personalized plan that addresses your unique symptoms, history and lifestyle.
While the specifics will be tailored with your healthcare provider, the following framework outlines the essential steps to building a successful and sustainable long-term treatment plan.
Step 1: Professional Consultation and Diagnosis (The Non-Negotiable Start)
Before attempting any treatment, you must see a doctor or a sleep specialist.
This is the most critical step for several reasons:
- Confirm the Diagnosis: Ensure that your sleep problem is indeed chronic insomnia.
- Rule Out Other Disorders: Your doctor needs to screen for other conditions that can mimic or cause insomnia, most notably Obstructive Sleep Apnea (OSA), Restless Legs Syndrome (RLS) and circadian rhythm disorders. Treating insomnia without addressing an underlying OSA, for example, can be ineffective and even dangerous.
- Assess Comorbidities: A thorough evaluation of your physical and mental health will identify any co-occurring conditions that need to be managed as part of the plan.
Step 2: Start with Cognitive Behavioral Therapy for Insomnia (CBT-I)
As established throughout this guide, CBT-I is the cornerstone of effective long-term treatment.
This should be the starting point for nearly everyone with chronic insomnia. Discuss your options with your provider:
- Finding a Therapist: Ask for a referral to a psychologist or therapist trained in CBT-I.
- Using Digital CBT-I: If access to a therapist is limited, ask about validated and FDA-cleared digital programs (dCBT-I). These are highly effective and can be started immediately.
Step 3: Discussing Medication as an Adjunct, Not a Crutch
Medication can play a valuable role, but its purpose should be strategic.
Discuss with your doctor whether medication is appropriate for you, considering scenarios such as:
- As a Bridge to CBT-I: Using a medication for a short period to provide immediate relief and improve your ability to engage with the demands of CBT-I.
- For Severe Symptoms: If your insomnia is causing extreme distress or functional impairment, medication can help stabilize the situation.
- If CBT-I Alone is Insufficient: For a small subset of individuals, CBT-I may not be fully effective on its own. In these cases, long-term medication (like a DORA) may be considered as a maintenance therapy.
Step 4: Incorporate Lifestyle and Sleep Hygiene as Supportive Structures
While your core treatment will be CBT-I and potentially medication, a healthy lifestyle provides the supportive structure that holds the plan together.
This is where you integrate good sleep hygiene, a balanced diet, regular exercise and stress management techniques like mindfulness or yoga.
These elements reinforce the work you’re doing in therapy and promote overall well-being.
Step 5: Regular Follow-Up and Adjustment
A long-term plan is not static. It’s a dynamic process that requires monitoring and adjustment.
Schedule regular follow-up appointments with your healthcare provider to:
- Track Progress: Use a sleep diary to monitor your sleep patterns and efficiency.
- Adjust the Plan: Your provider can help you fine-tune your CBT-I techniques or medication regimen as your sleep improves.
- Plan for Medication Tapering: If you started on medication, work with your doctor to create a gradual tapering plan as your CBT-I skills become more robust.
By following these steps, you move from passively suffering from insomnia to actively managing your sleep health with a clear, evidence-based strategy.
Frequently Asked Questions (FAQ)
1. Can chronic insomnia ever be cured permanently?
While “cure” can be a tricky word, many people achieve long-term remission where insomnia is no longer a significant problem in their lives. CBT-I provides the skills to manage sleep effectively, so even if you have a bad night, you have the tools to prevent it from spiraling back into a chronic issue.
2. How long does it take for CBT-I to work?
Most people begin to see noticeable improvements within 2 to 4 weeks of starting a CBT-I program. The full course typically lasts 4 to 8 sessions. The benefits are durable and often continue to improve even after therapy ends.
3. Is it safe to take melatonin every night for insomnia?
While generally considered safe for short-term use, the AASM does not recommend melatonin for chronic insomnia due to weak evidence. Long-term safety is not well-established, and supplement quality can vary. It’s best to consult a doctor before using it regularly.
4. Will I have to be on insomnia medication for life?
Not necessarily. The goal for many is to use medication as a temporary tool while learning CBT-I skills. However, for some individuals with severe, persistent insomnia, long-term maintenance medication under a doctor’s supervision may be an appropriate part of their treatment plan.
5. Can exercise help my chronic insomnia?
Yes, regular moderate-intensity exercise has been shown to improve sleep quality and duration. It can reduce anxiety and deepen sleep. However, try to avoid vigorous exercise within 2-3 hours of bedtime, as it can be too stimulating for some.
6. What’s the difference between a sleep specialist and a regular doctor?
A primary care doctor can diagnose and treat uncomplicated insomnia. A board-certified sleep specialist has advanced training in diagnosing and managing all types of sleep disorders, including complex cases, comorbid conditions, and disorders like sleep apnea that require specialized testing (e.g., a sleep study).
7. Does insurance cover CBT-I or new insomnia medications?
Coverage varies widely. CBT-I delivered by a licensed psychologist is often covered under mental health benefits. Some insurers are beginning to cover digital CBT-I programs. Newer medications like DORAs can be expensive and may require prior authorization or trying other medications first.
8. Can I drink alcohol if I have chronic insomnia?
It is strongly advised to avoid alcohol, especially near bedtime. While alcohol is a sedative and may help you fall asleep faster, it severely disrupts sleep architecture in the second half of the night, leading to frequent awakenings and non-restorative sleep.
Conclusion
Navigating the exhausting world of chronic insomnia can feel isolating and hopeless.
However, as this guide has shown, the path to restful nights is well-defined and supported by decades of scientific research.
You are not powerless in this struggle, and lasting improvement is not only possible but probable with the right approach.
The key takeaway is this: chronic insomnia is a treatable disorder, not a life sentence.
The most effective, durable solution is Cognitive Behavioral Therapy for Insomnia (CBT-I), a powerful program that retrains your brain and behaviors for healthy sleep by addressing the root causes of the problem.
For those who need additional support, modern pharmacology has provided newer, safer long-term medication options like DORAs that work in harmony with the body’s natural sleep-wake cycle.
The journey begins with a single, decisive action. Don’t accept sleepless nights as your normal. Don’t resign yourself to a life of fatigue. Take the first and most important step on your path to recovery.
Schedule a conversation with your healthcare provider today. Discuss your symptoms, your struggles, and your desire for a long-term solution. Ask about CBT-I. A personalized, evidence-based treatment plan is within your reach.
Have you found a long-term strategy that works for your insomnia? Share your experience in the comments below to help others on their journey.
Reference
[1] Chronic Insomnia – StatPearls – NCBI Bookshelf
https://www.ncbi.nlm.nih.gov/books/NBK526136
[2] Cognitive-Behavioral Therapy for Insomnia: An Effective …
https://pmc.ncbi.nlm.nih.gov/articles/PMC6796223
[3] https://www.healthline.com/health/insomnia
[4] https://www.sleepfoundation.org/insomnia
[5] https://www.mayoclinic.org/diseases-conditions/insomnia/symptoms-causes/syc-20355167
[6] New treatments to put insomnia to bed
https://www.nature.com/articles/d41586-025-00963-x
[7] What is sleep restriction therapy for insomnia?
https://sleepeducation.org/sleep-restriction-therapy-insomnia
[8] Sleep Restriction and CBTI | Stanford Health Care

