The primary signs you might have a cavity are tooth sensitivity to temperatures or sweets, visible discoloration or holes, pain when biting down, a persistent toothache, and chronic bad breath or a bad taste in your mouth.
Recognizing these symptoms early is crucial for preventing more serious dental problems.
According to the World Health Organization (WHO), untreated dental caries (the disease that causes a cavity) in permanent teeth is the single most common health condition worldwide, affecting an estimated 3.7 billion people.
Despite its prevalence, many people don’t know how to spot a cavity in its early stages, when it’s most treatable.
This comprehensive guide will walk you through the five most common signs, explain what a cavity looks and feels like, and detail the causes, prevention strategies, and modern treatment options available.
Read on to empower yourself with the knowledge to protect your oral health.
In This Article
What Is a Cavity and Why Should You Care?
Before diving into the signs, it’s essential to understand what a cavity is.
A cavity is not just a minor inconvenience, it’s a sign of a progressive disease that can lead to significant pain, infection, and even tooth loss if left untreated.
Defining the Terms: Cavity, Tooth Decay, and Caries
You’ll often hear these three terms used interchangeably, but they have distinct meanings:
- Dental Caries: This is the scientific name for the disease process itself. As defined by the National Center for Biotechnology Information (NCBI), it’s an infectious disease caused by bacteria in your mouth that metabolize sugars and produce acid.
- Tooth Decay: This is a common term for the effects of the caries process—the gradual destruction of tooth structure.
- Cavity: This is the physical result of untreated tooth decay. It’s a hole or permanently damaged area that forms in the hard surface of your tooth.
In short, caries is the disease, tooth decay is the process, and a cavity is the lesion that results.
The Global Impact: A Common but Serious Problem
The statistics surrounding tooth decay are staggering. It is the most common chronic disease in both children and adults in the United States, according to Healthy People 2030.
The Centers for Disease Control and Prevention (CDC) reports that over 90% of U.S. adults have had at least one cavity, and about 1 in 4 adults currently have untreated decay.
This isn’t just a cosmetic issue, a severe cavity can lead to complications like a painful tooth abscess, infection spreading to other parts of the body, and problems with chewing and nutrition.
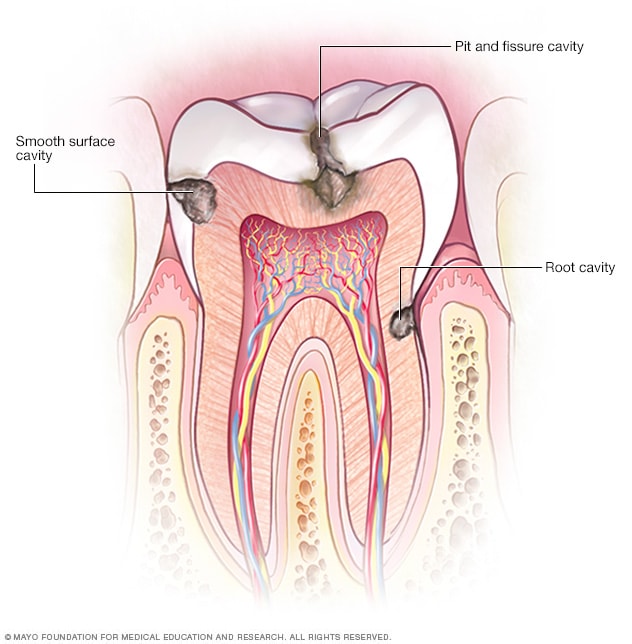
There are three main types of cavities: smooth surface, root, and pit and fissure cavities.
The Process of Tooth Decay: A Tug-of-War in Your Mouth
The National Institute of Dental and Craniofacial Research (NIDCR) describes tooth decay as a dynamic “tug-of-war” happening inside your mouth. On one side, you have harmful factors, and on the other, protective ones.
- Plaque Forms and Attacks: A sticky film of bacteria called dental plaque constantly forms on your teeth. When you consume sugary or starchy foods and drinks, these bacteria feed on the sugars and produce acids.
- Demineralization: These acids attack the tooth’s hard outer layer, the enamel, leaching out essential minerals like calcium and phosphate. This process is called demineralization.
- Remineralization: Your body fights back. Saliva contains minerals that help repair the enamel, and fluoride from toothpaste and water also helps replenish lost minerals. This is remineralization.
- A Cavity Forms: A cavity develops when the demineralization process happens faster than the remineralization process. The repeated acid attacks weaken and eventually destroy the enamel, creating a hole.
Sign #1: Tooth Sensitivity – The Early Warning System
One of the earliest and most common cavity symptoms is new or worsening tooth sensitivity.
This isn’t the same as the generalized sensitivity many people experience, it’s often more specific and pointed.
What Does Cavity Sensitivity Feel Like?
Sensitivity from a cavity often manifests as a short, sharp pain or a tingling sensation when the affected tooth is exposed to certain triggers. Common triggers include:
- Hot or Cold: A sudden twinge of pain when drinking hot coffee or eating ice cream.
- Sweet or Sugary: A sharp ache after eating a piece of candy, a cookie, or drinking soda.
- Acidic: Discomfort from foods and drinks like citrus fruits, tomatoes, or juice.
The pain is typically temporary and subsides once the trigger is removed. However, as the cavity deepens, the sensitivity can become more intense and linger longer.
Why Does a Cavity Cause Sensitivity?
Your tooth’s enamel is the hardest substance in your body and has no nerves. However, beneath the enamel lies a softer layer called dentin.
Dentin is porous and contains thousands of microscopic tubules that lead directly to the tooth’s nerve center, the pulp. When tooth decay erodes the protective enamel, it exposes the dentin.
The triggers (hot, cold, sweet) can then travel through these tubules and stimulate the nerve, causing that sharp jolt of pain.
Is It a Cavity or Just General Sensitivity?
It can be tricky to tell the difference. However, there are some clues. The table below compares sensitivity from a cavity versus more generalized sensitivity, which might be caused by gum recession or enamel wear.
| Feature | Sensitivity from a Cavity | Generalized Tooth Sensitivity |
|---|---|---|
| Location | Often localized to a single tooth or a specific spot. | Can affect multiple teeth or an entire area of the mouth. |
| Sensation | Typically a sharp, intense, and sudden pain. | Often a duller, more diffuse ache. |
| Onset | May appear suddenly and worsen over time. | Often develops gradually and can fluctuate. |
| Primary Triggers | Sweets are a very common and specific trigger. Hot and cold also cause pain. | Primarily triggered by hot and cold temperatures or cold air. |
| Associated Signs | May be accompanied by visible discoloration or a hole. | Often associated with receding gums or worn-down teeth. |
If you experience new or localized sensitivity, especially to sweets, it’s a strong indicator that you should see a dentist to rule out a cavity.
Sign #2: Visible Changes – What Does a Cavity Look Like?
While some cavities are hidden between teeth and only visible on an X-ray, many present visual cues. Knowing what to look for can help you catch tooth decay early.
The Earliest Visual Cue: White Spot Lesions
The very first visible sign of a cavity is often a “white spot lesion”. This appears as a chalky, dull white patch on the tooth’s surface.
This spot indicates an area of demineralization where the enamel has lost minerals but has not yet broken down.
At this stage, the decay process is often reversible with improved oral hygiene and fluoride treatments.
Progression to Brown and Black Spots
If the decay process continues, the lesion can become stained by foods and drinks, turning a light brown, dark brown, or even black color.
It’s important to note that not all dark spots are a cavity. Stains can also accumulate in the natural pits and fissures of your teeth.
However, a discolored spot, especially if it feels soft or “sticky” to a dental instrument, is a strong sign of an active cavity.
Pits and Holes You Can See or Feel
This is the classic sign of a cavity. As the enamel and dentin continue to decay, a noticeable pit or hole will form.
You might be able to see it in the mirror or feel it with your tongue.
These holes can trap food particles, making them difficult to clean and accelerating the decay process.
A Visual Guide: The 6 Stages of Tooth Decay
Understanding the progression of a cavity can help you appreciate the importance of early detection. The decay process is typically broken down into six stages:
- Stage 1: Demineralization (White Spots): The initial stage where enamel loses minerals. It appears as a white spot. This stage is reversible.
- Stage 2: Enamel Decay: The decay breaks through the surface of the enamel, forming a small cavity. The damage is now permanent and requires a filling.
- Stage 3: Dentin Decay: The decay reaches the softer dentin layer. At this point, the cavity grows much faster and sensitivity or pain may begin.
- Stage 4: Pulp Involvement: The decay penetrates to the pulp, the tooth’s nerve and blood vessel center. This often causes significant pain and inflammation (pulpitis). A root canal is typically necessary.
- Stage 5: Abscess Formation: The infection spreads from the pulp to the tip of the tooth’s root, forming a pocket of pus called an abscess. This can cause severe, throbbing pain, swelling, and can be a serious health risk.
- Stage 6: Tooth Loss: If the tooth structure is too compromised by decay and infection, it may need to be extracted.
Sign #3: Pain – From Mild Discomfort to Severe Aches
While sensitivity is a type of pain, a cavity can also cause other kinds of pain, especially as it progresses. This pain is a clear signal from your body that something is wrong.
Pain When Biting Down
Do you feel a sharp pain when you chew or apply pressure to a specific tooth? This can be a sign that decay has weakened the tooth’s internal structure.
The pressure of biting down can irritate the inflamed pulp or stress the weakened tooth, causing pain.
This symptom should never be ignored, as it can also indicate a cracked tooth or a damaged filling.
Spontaneous or Persistent Toothache
In the early stages, cavity pain is usually triggered. But as the decay reaches the pulp, the pain can become spontaneous, meaning it occurs without any obvious cause.
You might experience a dull, constant ache or throbbing pain that comes and goes. This type of toothache can be distracting and may even wake you up at night.
It’s a sign that the nerve is infected or severely inflamed and requires immediate dental attention.
Sign #4: Bad Breath or a Bad Taste That Won’t Go Away
If you notice persistent bad breath (halitosis) or a foul taste in your mouth that doesn’t improve with brushing and flossing, a cavity could be the culprit.
The bacteria that cause tooth decay release smelly waste products as they break down food particles. A hole in your tooth provides a perfect, hard-to-clean shelter for these bacteria and trapped food debris to fester.
This can create a persistent unpleasant odor or taste that originates from the site of the cavity.
Sign #5: Food Constantly Getting Stuck in a Tooth
Do you find that one particular spot in your mouth always seems to trap food? Whether it’s a piece of meat or a popcorn kernel, if food consistently gets lodged in the same tooth, it could be because a cavity has created a hole or a rough edge.
This can also happen if a cavity between two teeth has damaged their contact point, creating a gap where food can become impacted. This not only is annoying but also provides more fuel for the decay-causing bacteria, making the cavity worse.
What Causes a Cavity? Understanding the Risk Factors
Anyone with teeth can get a cavity, but certain factors increase your risk. According to the Mayo Clinic, these include:
- Poor Oral Hygiene: Not brushing and flossing effectively allows plaque to build up.
- Frequent Snacking and Sipping: Constantly exposing your teeth to sugars and starches fuels acid-producing bacteria.
- High-Sugar Diet: Foods and drinks like soda, candy, dried fruit, and even chips cling to teeth and promote decay.
- Dry Mouth: Saliva helps wash away food and neutralize acids. A lack of saliva, often caused by medications or medical conditions, increases cavity risk.
- Tooth Location: Back teeth (molars and premolars) have more grooves and are harder to clean, making them more susceptible to a cavity.
- Worn Fillings or Dental Devices: Old fillings can break down, creating rough edges where plaque can accumulate.
- Heartburn (GERD): Stomach acid flowing back into the mouth can severely erode tooth enamel.
How Do Dentists Diagnose a Cavity?
You can’t always see or feel a cavity, which is why regular dental checkups are essential.
Dentists use several methods to detect tooth decay, even in its earliest stages.
- Visual-Tactile Examination: Your dentist will visually inspect each tooth for signs of decay, such as discoloration or pits. They will use a dental explorer (a sharp, pointed instrument) to gently feel the tooth surfaces for soft or sticky spots, which indicate a cavity.
- Dental X-rays (Radiographs): X-rays are crucial for finding decay that isn’t visible to the naked eye, such as a cavity between teeth, under an existing filling, or in the early stages within the enamel. On an X-ray, decay appears as a darker spot on the tooth.
- Laser Fluorescence Detection: Some dentists use a special laser device that can detect early-stage cavities. It measures the fluorescence within the tooth structure, healthy tooth structure has little to no fluorescence, while decayed areas will fluoresce.
How to Get Rid of a Cavity: Modern Treatment Options
The treatment for a cavity depends on its stage and severity. The goal is always to preserve as much of the natural tooth as possible.
| Stage of Decay | Common Treatment | Description |
|---|---|---|
| Stage 1: White Spots | Fluoride Treatments | In the earliest stage, a professional fluoride treatment (gel, varnish, or foam) can help the enamel remineralize and reverse the decay process. No drilling is needed. |
| Stages 2 & 3: Enamel/Dentin Decay | Dental Filling (Restoration) | This is the most common treatment for a cavity. The dentist removes the decayed portion of the tooth and “fills” the area with a material like composite resin (tooth-colored), amalgam (silver), or porcelain. |
| Stage 4: Pulp Involvement | Root Canal Therapy | When the decay reaches the pulp, the infected or inflamed pulp must be removed. The inside of the tooth is cleaned and sealed. The tooth is then typically covered with a crown. |
| Advanced Decay | Dental Crown | For a large cavity or a tooth weakened by decay, a crown (or “cap”) is placed over the entire tooth to restore its shape, size, strength, and appearance. |
| Stage 6: Severe Damage | Tooth Extraction | If the tooth is too damaged to be saved, it will need to be removed. The missing tooth can then be replaced with a dental implant, bridge, or partial denture. |
Prevention Is Key: How to Stop a Cavity Before It Starts
The best way to deal with a cavity is to prevent it from ever forming. Good oral hygiene and lifestyle choices are your best defense.
- Brush Thoroughly: Brush your teeth at least twice a day for two minutes with a fluoride toothpaste.
- Floss Daily: Flossing removes plaque and food from between your teeth and under the gumline, where your toothbrush can’t reach.
- Use Fluoride: Fluoride is a mineral that strengthens enamel and can reverse early decay. Ensure your toothpaste contains it and drink fluoridated tap water.
- Limit Sugary Foods and Drinks: Reduce your intake of soda, juice, candy, and other sweets. If you do indulge, do so with a meal rather than snacking throughout the day.
- Visit Your Dentist Regularly: Professional cleanings and exams (typically every six months) are essential for removing tartar and catching any problems early.
- Consider Dental Sealants: For children and teenagers, sealants—a thin, protective coating applied to the chewing surfaces of back teeth—can be highly effective at preventing a cavity.
Frequently Asked Questions (FAQ)
1. Can a cavity go away on its own?
No, once a physical hole (a cavity) has formed, it cannot heal on its own. However, the earliest stage of decay (a white spot lesion) can be reversed with fluoride and good oral hygiene before it becomes a true cavity.
2. Does a cavity always hurt?
No. In the early stages, a cavity is often painless. Pain and sensitivity typically only begin once the decay has progressed to the deeper layers of the tooth. This is why regular dental checkups are so important for early detection.
3. How long does it take for a cavity to form?
It varies greatly depending on diet, oral hygiene, and other risk factors. A cavity can take months or even years to develop. In high-risk individuals with very sugary diets, however, decay can progress much more rapidly.
4. Can you get a cavity under a crown or filling?
Yes. This is called recurrent decay. It occurs when plaque accumulates at the margin (the edge) of a filling or crown, causing a new cavity to form in the adjacent tooth structure. Good hygiene is crucial for protecting dental work.
5. Are baby teeth cavities a big deal?
Yes. According to the NIDCR, decay in baby teeth can cause pain, infection, and problems with eating and speaking. If a baby tooth is lost too early due to a cavity, it can also cause spacing issues for the permanent teeth that follow.
6. What does a cavity filling procedure involve?
The dentist will numb the area, remove the decayed tooth structure with a drill, clean the space, and then place the filling material. The procedure is typically quick and painless thanks to local anesthesia.
7. Is it possible to have a cavity between teeth?
Yes, these are called interproximal cavities. They are common because these areas are difficult to clean. Daily flossing is the best way to prevent this type of cavity. They are usually detected with dental X-rays.
8. What’s the difference between a cavity and a stain?
A stain is a surface discoloration that can often be polished off. A cavity is structural damage to the tooth. While a cavity can be discolored, it also involves a softening or breakdown of the tooth that a dentist can detect.
Conclusion
A cavity is far more than a small hole in your tooth, it’s a sign of a preventable disease.
By learning to recognize the five telltale signs—sensitivity, visible changes, pain, bad breath, and food trapping—you can seek timely care and prevent minor issues from becoming major problems.
Remember that the earliest stages of decay are often silent, making your partnership with your dental team more important than ever.
Adopt a proactive approach to your oral health. Practice diligent brushing and flossing, make smart dietary choices, and never skip your regular dental checkups.
By doing so, you can win the “tug-of-war” against tooth decay and keep your smile healthy and strong for a lifetime.
If you are experiencing any of the symptoms described in this article, don’t wait. Schedule an appointment with your dentist today.
Early detection and treatment are the keys to preserving your teeth and your overall well-being.
Medical Disclaimer: The information in this article is intended for general informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your dentist or other qualified health provider with any questions you may have regarding a medical condition.

