For a non-diabetic adult, a normal fasting blood sugar level is generally below 100 mg/dL (5.6 mmol/L), and a level less than 140 mg/dL (7.8 mmol/L) two hours after eating is considered normal. These numbers are more than just clinical data, they are vital indicators of your metabolic health.
Consider this: according to the Centers for Disease Control and Prevention (CDC), over 96 million American adults—more than 1 in 3—have prediabetes, and more than 80% of them don’t even know it.
This silent epidemic underscores the critical importance of understanding your blood sugar levels before they lead to irreversible health complications.
This guide will provide a comprehensive exploration of blood sugar management. We will demystify the numbers, explaining the crucial differences between normal, prediabetic, and diabetic ranges.
You will learn to recognize the subtle and overt symptoms of both high and low blood sugar, understand the various methods for testing your levels, and discover how factors like age, pregnancy and lifestyle can influence these vital metrics.
Understanding your personal numbers is the first, most powerful step you can take toward safeguarding your long-term health and well-being.
In This Article
What Is Blood Sugar (Glucose) and Why Is It Important?
At its core, blood sugar, or more technically glucose, is the primary fuel that powers every cell in your body.
From the complex firing of neurons in your brain to the contraction of your heart muscle, nearly every physiological process depends on a steady supply of this simple sugar. It is the fundamental currency of energy in our biological economy.
When you consume foods containing carbohydrates—like bread, fruits and vegetables—your digestive system breaks them down into glucose. This glucose is then absorbed into your bloodstream, causing your blood sugar levels to rise. This is a normal and necessary process.
However, for glucose to be used by your cells, it needs help. This is where insulin comes in. Insulin is a hormone produced by the beta cells in your pancreas, an organ located behind your stomach. Think of insulin as a key.
When glucose is circulating in your blood, the pancreas releases insulin, which travels to your cells and “unlocks” them, allowing glucose to enter and be converted into energy. Any excess glucose is stored in the liver and muscles as glycogen for later use.
This intricate system is designed to maintain a state of balance, or homeostasis. When this balance is disrupted—either because the pancreas doesn’t produce enough insulin (as in Type 1 diabetes) or because the cells become resistant to insulin’s effects (as in Type 2 diabetes)—the entire system falters.
Maintaining stable blood sugar levels is therefore not just a concern for people with diabetes, it is a cornerstone of overall health, affecting everything from your energy and mood to your risk of chronic disease.
What Is a “Normal” Blood Sugar Level? The Official Ranges
Understanding the specific numbers that define normal, prediabetic, and diabetic states is crucial for interpreting your health status. These ranges, established by leading health organizations like the American Diabetes Association (ADA), are the gold standard for diagnosis and management.
They are typically measured in milligrams per deciliter (mg/dL) in the United States, or millimoles per liter (mmol/L) in many other parts of the world.
The Definitive Blood Sugar Levels Chart (mg/dL and mmol/L)
The following table provides a clear, at-a-glance reference for diagnosing and categorizing blood sugar levels based on three key tests: the Fasting Plasma Glucose (FPG) test, the Oral Glucose Tolerance Test (OGTT) and the Hemoglobin A1C test.
| Category | Fasting (8+ hours, no food) | 2 Hours After Meal (Postprandial) | Hemoglobin A1C (%) |
|---|---|---|---|
| Normal | Less than 100 mg/dL (5.6 mmol/L) | Less than 140 mg/dL (7.8 mmol/L) | Less than 5.7% |
| Prediabetes | 100 to 125 mg/dL (5.6 to 6.9 mmol/L) | 140 to 199 mg/dL (7.8 to 11.0 mmol/L) | 5.7% to 6.4% |
| Diabetes | 126 mg/dL (7.0 mmol/L) or higher | 200 mg/dL (11.1 mmol/L) or higher | 6.5% or higher |
Source: American Diabetes Association (ADA) Standards of Medical Care in Diabetes. A diagnosis of diabetes or prediabetes typically requires two abnormal test results from the same sample or in two separate test samples.
Interpreting Your Results: Normal vs. Prediabetes vs. Diabetes
- Normal: If your numbers fall into this range, your body is effectively managing glucose. This is the target for optimal metabolic health.
- Prediabetes: This category serves as a critical warning sign. Your blood sugar levels are higher than normal but not yet high enough to be classified as Type 2 diabetes. Prediabetes significantly increases your risk for developing Type 2 diabetes, heart disease and stroke. However, with lifestyle interventions like diet and exercise, progression to diabetes can often be prevented or delayed.
- Diabetes: A result in this range indicates that your body can no longer regulate blood sugar effectively. A fasting glucose of 126 mg/dL or higher or an A1C of 6.5% or higher on two separate occasions is a standard diagnostic criterion. This condition requires medical management to prevent serious long-term complications.
What Is High Blood Sugar (Hyperglycemia)?
Hyperglycemia is the medical term for high blood sugar. It occurs when the body has too little insulin or when the body can’t use insulin properly.
While occasional, minor spikes after a carb-heavy meal can happen, persistent hyperglycemia is a hallmark of unmanaged diabetes and can be damaging over time.
The Telltale Symptoms of Hyperglycemia
Early symptoms of hyperglycemia can be subtle and easy to dismiss. However, as blood sugar levels remain high, the signs become more pronounced. Recognizing them is the first step toward taking action.
- Increased Thirst (Polydipsia): As excess sugar builds up in your bloodstream, your kidneys go into overdrive to filter and absorb it. When they can’t keep up, the excess sugar is excreted into your urine, dragging fluids from your tissues along with it, leading to dehydration and intense thirst.
- Frequent Urination (Polyuria): This is a direct consequence of the kidneys flushing out excess glucose, leading to more frequent trips to the bathroom, especially at night.
- Blurred Vision: High blood sugar can cause the lens of your eye to swell, changing its shape and affecting your ability to focus. This is often temporary and resolves once blood sugar levels are stabilized.
- Fatigue and Weakness: When glucose can’t enter your cells to be used for energy, your body is literally starved of its main fuel source, leading to persistent tiredness and a feeling of weakness.
- Headaches: Dehydration and the effects of high blood sugar on blood vessels in the brain can trigger headaches.
- Slow-healing Sores or Infections: Hyperglycemia impairs the function of white blood cells, which are crucial for fighting infection, and can also lead to poor circulation, making it harder for the body to heal.
What Causes Blood Sugar to Spike?
Several factors can contribute to hyperglycemia, particularly in individuals with diabetes. According to experts at the Mayo Clinic, common triggers include:
- Diet: Consuming more carbohydrates than your body can handle with its available insulin is the most common cause. Sugary drinks, processed foods, and large portion sizes are frequent culprits.
- Lack of Physical Activity: Exercise helps your body use glucose for energy and makes your cells more sensitive to insulin. A sedentary lifestyle does the opposite.
- Illness or Infection: When you’re sick, your body releases stress hormones (like cortisol) to fight the illness. These hormones can raise blood sugar levels.
- Stress: Both emotional and physical stress can trigger the release of hormones that elevate blood sugar.
- Medication Issues: For people with diabetes, skipping doses of insulin or oral diabetes medication, or not taking enough, will directly lead to hyperglycemia. Certain other medications, like steroids, can also raise blood sugar.
The Long-Term Dangers of Uncontrolled High Blood Sugar
If left untreated, chronic hyperglycemia can lead to severe and life-altering complications. The excess sugar in the blood acts like a slow-acting poison, damaging blood vessels and nerves throughout the body.
“The key aim of diabetes management is to prevent complications, which are a major cause of morbidity and mortality”, states a 2024 review in PubMed. Keeping blood sugar levels in a healthy range is the best way to prevent these long-term problems.
Major complications, as detailed by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), include:
- Cardiovascular Disease: Diabetes dramatically increases the risk of heart attack, stroke and high blood pressure.
- Nerve Damage (Neuropathy): High blood sugar can injure the walls of the tiny capillaries that nourish your nerves, especially in your legs and feet. This can cause tingling, numbness, burning, or pain and can eventually lead to a complete loss of feeling.
- Kidney Disease (Nephropathy): The kidneys contain millions of tiny blood vessel clusters (glomeruli) that filter waste from your blood. Diabetes can damage this delicate filtering system, leading to kidney failure.
- Eye Damage (Retinopathy): Diabetes can damage the blood vessels of the retina, potentially leading to blindness. It also increases the risk of cataracts and glaucoma.
- Diabetic Ketoacidosis (DKA): A life-threatening emergency that occurs when the body, lacking insulin, starts breaking down fat for fuel at a dangerous rate, producing toxic acids called ketones.
What Is Low Blood Sugar (Hypoglycemia)?
Hypoglycemia, or low blood sugar, occurs when the level of glucose in your blood drops below the normal range (typically below 70 mg/dL or 3.9 mmol/L).
While less common in the general population, it is a significant and immediate risk for people with diabetes, especially those who use insulin.
Recognizing the Signs of a Blood Sugar Crash
The body’s response to low blood sugar is swift, as the brain is highly dependent on glucose to function. Symptoms can appear quickly and should be treated immediately.
- Mild to Moderate Symptoms:
- Shakiness or trembling
- Sweating, chills and clamminess
- Anxiety or nervousness
- Irritability or impatience
- Rapid heartbeat (palpitations)
- Dizziness or lightheadedness
- Hunger and nausea
- Severe Symptoms (require immediate medical attention):
- Confusion or difficulty concentrating
- Blurred or impaired vision
- Slurred speech
- Loss of coordination
- Seizures
- Loss of consciousness
Common Causes of Hypoglycemia
In people with diabetes, hypoglycemia is often a result of a mismatch in the timing or amount of medication, food and activity.
- Too much insulin or diabetes medication: This is the most frequent cause.
- Skipping or delaying a meal: Not providing the glucose needed to balance the medication in your system.
- Increased physical activity: Exercising more than usual without adjusting food intake or medication can rapidly deplete glucose stores.
- Drinking alcohol: The liver prioritizes metabolizing alcohol over releasing glucose, which can lead to a drop in blood sugar, especially if drinking on an empty stomach.
In people without diabetes, a condition known as reactive hypoglycemia can occur a few hours after a meal, though this is less common. Other rare causes include certain tumors or critical illnesses.
How to Treat Low Blood Sugar Fast: The “15-15 Rule”
For conscious individuals experiencing mild to moderate hypoglycemia, the American Diabetes Association recommends the simple and effective “15-15 Rule”. This is a critical piece of information that can be life-saving.
The 15-15 Rule for Treating Hypoglycemia
- Consume 15 grams of a fast-acting carbohydrate. This is a source of sugar that can be quickly absorbed by the body. Examples include:
- 4 glucose tablets
- 4 ounces (1/2 cup) of juice or regular soda (not diet)
- 1 tablespoon of sugar, honey or corn syrup
- Hard candies, jellybeans, or gumdrops (check the label for 15g of carbs)
- Wait 15 minutes. Avoid the temptation to eat more, as this can cause your blood sugar to rebound too high. Let the sugar work.
- Re-check your blood sugar. If it is still below 70 mg/dL, repeat the process.
- Follow up with a snack. Once your blood sugar is back in the normal range, eat a small snack containing both carbohydrates and protein (like crackers with cheese or peanut butter) if your next meal is more than an hour away. This helps prevent another drop.
How Do You Check Your Blood Sugar Levels?
Monitoring blood sugar is the cornerstone of effective diabetes management and a valuable tool for anyone looking to understand their metabolic health.
There are several methods available, each providing a different piece of the puzzle.
At-Home Testing: The Blood Glucose Meter (BGM)
The blood glucose meter (BGM) is the traditional method of self-monitoring. It provides a snapshot of your blood sugar level at a specific moment in time using a small drop of blood.
How to Perform a Finger-Prick Test:
- Wash your hands: Use soap and warm water to clean your hands thoroughly and dry them completely. Food residue or dirt can affect the reading.
- Prepare the device: Insert a fresh test strip into your glucose meter.
- Lance your finger: Use the lancing device to prick the side of your fingertip. The sides have fewer nerve endings than the pad, making it less painful.
- Apply blood to the strip: Gently squeeze your finger to get a small drop of blood and touch it to the edge of the test strip.
- Read the result: The meter will analyze the blood and display your glucose reading within a few seconds.
Your doctor will advise you on how often to test, but common times include upon waking (fasting), before meals, 1-2 hours after meals, and at bedtime.
Modern Monitoring: Continuous Glucose Monitors (CGM)
A Continuous Glucose Monitor (CGM) is a wearable device that tracks your glucose levels automatically, 24/7. It consists of a tiny sensor inserted just under the skin (usually on the arm or abdomen) that measures glucose in the interstitial fluid—the fluid between your cells. This is a close proxy for blood glucose.
The sensor sends readings to a receiver or smartphone every few minutes, providing a dynamic view of your glucose trends. Key benefits include:
- Real-time data: See your glucose level at any moment without a finger prick.
- Trend arrows: Know whether your glucose is rising, falling, or stable, allowing for proactive decisions.
- Alarms: Set customizable alerts for high and low glucose levels, which can be life-saving, especially overnight.
- Comprehensive data: See the full picture of how diet, exercise, and stress affect your glucose levels throughout the day and night.
The Big Picture: Understanding the Hemoglobin A1C Test
The Hemoglobin A1C (or HbA1c) test is different from daily glucose monitoring. It doesn’t measure your current blood sugar but instead provides an average of your blood sugar levels over the past 2-3 months.
As explained by the Cleveland Clinic, the test works by measuring the percentage of hemoglobin (a protein in red blood cells that carries oxygen) that has become “glycated” or coated with sugar.
Think of A1C as a baseball player’s batting average for the season, while a BGM reading is the result of a single at-bat. The batting average gives a much better sense of the player’s overall performance.
Similarly, the A1C gives you and your doctor a reliable overview of your long-term glucose control, making it the gold standard for diagnosing diabetes and assessing management effectiveness.
BGM vs. CGM vs. A1C: Which Test is Right for You?
Each testing method offers unique insights. The best approach often involves a combination, tailored to an individual’s needs and medical advice.
| Feature | Blood Glucose Meter (BGM) | Continuous Glucose Monitor (CGM) | Hemoglobin A1C Test |
|---|---|---|---|
| What it Measures | Glucose in the blood at a single point in time. | Glucose in the interstitial fluid, continuously (every 1-5 mins). | Average blood glucose over the past 2-3 months. |
| Type of Data | A single number (snapshot). | A continuous stream of data, trends and patterns. | A single percentage (long-term average). |
| Primary Use | Making immediate treatment decisions (e.g., insulin dose). | Understanding trends, preventing highs/lows, lifestyle adjustments. | Diagnosing diabetes, assessing long-term management success. |
| Convenience | Requires multiple finger pricks per day. | Sensor worn for 7-14 days, minimal finger pricks (for calibration). | A simple blood draw done every 3-6 months. |
| Accuracy | Considered highly accurate for real-time decisions. Lab tests are the benchmark. | Highly accurate, but with a 5-15 minute lag behind blood glucose. | Very accurate for long-term average but misses daily fluctuations. |
Do Normal Blood Sugar Targets Change with Age?
While the fundamental principles of glucose metabolism remain the same throughout life, the recommended target ranges and management strategies can be adjusted based on age and overall health status.
A one-size-fits-all approach is not always optimal.
Pediatric Blood Sugar Levels (Children & Teens)
Managing blood sugar in children and adolescents with diabetes presents unique challenges. Growth spurts, hormonal changes during puberty, unpredictable eating habits and variable activity levels can all cause significant glucose fluctuations.
The primary goal is to maintain levels as close to normal as possible to support healthy growth and development while minimizing the risk of both acute and long-term complications.
According to guidelines from organizations like the Dartmouth Health Children’s Hospital, target ranges are often slightly wider than for adults to provide a safety buffer against hypoglycemia:
- Children under 5 years: Target range often 80-200 mg/dL.
- Children 5 to 11 years: Target range often 70-180 mg/dL.
- Teens 12 years and up: Target range often 70-150 mg/dL, moving closer to adult targets.
These are general guidelines, and individual goals must be set with a pediatric endocrinologist.
Blood Sugar Goals for Older Adults (65+)
For older adults, particularly those over 65, the focus of diabetes management often shifts. While controlling hyperglycemia is still important, preventing hypoglycemia becomes a paramount concern.
Falls, confusion, and dizziness caused by low blood sugar can have devastating consequences in this population.
The ADA’s “Standards of Care in Diabetes—2024” recommends individualizing glycemic goals.
For healthy older adults with a long life expectancy, standard adult goals (e.g., A1C <7%) may be appropriate. However, for those with multiple chronic illnesses, cognitive impairment, or functional limitations, less stringent goals are often safer:
- Fasting Glucose Target: May be relaxed to 90–150 mg/dL.
- Bedtime Glucose Target: May be relaxed to 100–180 mg/dL.
- A1C Target: May be relaxed to <8.0% or even <8.5% to prioritize safety and quality of life.
The mantra becomes “start low, go slow” with medications, and the treatment plan must be regularly reassessed.
What Are the Target Blood Sugar Levels During Pregnancy?
Pregnancy brings about significant hormonal changes that can affect insulin sensitivity, sometimes leading to Gestational Diabetes Mellitus (GDM), a type of diabetes that develops during pregnancy in women who did not previously have diabetes.
Maintaining tight glycemic control is vital for the health of both the mother and the developing baby.
Uncontrolled high blood sugar during pregnancy can lead to complications such as a large-for-gestational-age baby (macrosomia), which increases the risk of birth injuries and C-section delivery, as well as preeclampsia and an increased risk of the child developing obesity and Type 2 diabetes later in life.
Consequently, blood sugar targets during pregnancy are stricter than for the general population. The American College of Obstetricians and Gynecologists (ACOG) and the ADA recommend the following targets for GDM:
- Fasting (before breakfast): Less than 95 mg/dL (5.3 mmol/L)
- One hour after a meal: Less than 140 mg/dL (7.8 mmol/L)
- Two hours after a meal: Less than 120 mg/dL (6.7 mmol/L)
These tight targets often require intensive management through diet, exercise and sometimes medication like insulin.
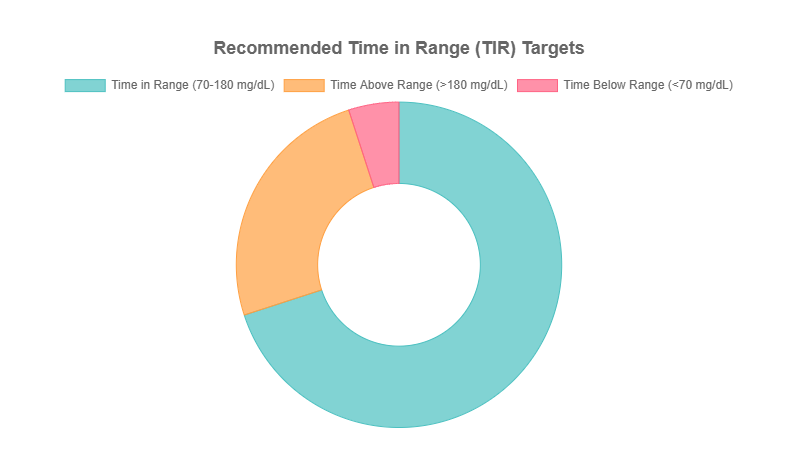
What Is “Time in Range” (TIR) and Why Does It Matter?
With the rise of Continuous Glucose Monitoring (CGM), a powerful new metric has emerged that is revolutionizing diabetes management: Time in Range (TIR).
While A1C provides a long-term average, it can’t capture the daily rollercoaster of highs and lows. TIR fills this critical gap.
TIR is defined as the percentage of time a person’s blood sugar levels stay within their target range. For most adults with Type 1 or Type 2 diabetes, the internationally agreed-upon target range is 70 to 180 mg/dL (3.9 to 10.0 mmol/L).
A 2025 study highlighted in Nature refers to TIR as a potential “new gold standard” because it provides a more nuanced view of glycemic control than A1C alone.
For example, two people could have the same A1C of 7.0%, but one might have stable glucose levels while the other experiences dangerous swings between severe highs and lows. TIR reveals this crucial difference.
International Consensus on TIR Targets
The general targets recommended for most adults with Type 1 or Type 2 diabetes are:
- Time in Range (70-180 mg/dL): >70% of the day (about 17 hours)
- Time Above Range (>180 mg/dL): <25% of the day (less than 6 hours)
- Time Below Range (<70 mg/dL): <4% of the day (less than 1 hour)
- Time in Severe Lows (<54 mg/dL): <1% of the day (less than 15 minutes)
Increasing TIR by even 5% (just 72 minutes a day) has been shown to have clinically significant benefits in reducing the risk of complications.
Frequently Asked Questions (FAQ)
What is considered a dangerously high blood sugar level?
A blood sugar level of 180 mg/dL or higher is considered high (hyperglycemia). Levels consistently above 250 mg/dL can be dangerous and may lead to diabetic ketoacidosis (DKA) if ketones are present, requiring urgent medical attention.
Can you have high blood sugar without having diabetes?
Yes, temporary high blood sugar can be caused by severe illness, stress, infection, or certain medications like steroids. This is known as stress hyperglycemia. However, persistent high blood sugar is a primary indicator of prediabetes or diabetes.
What should my blood sugar be at bedtime?
For most adults with diabetes, a common bedtime blood sugar target is between 100 and 140 mg/dL (5.6 to 7.8 mmol/L). This helps prevent both overnight hypoglycemia and high morning blood sugar levels. Your specific target should be set by your doctor.
How quickly does food affect blood sugar levels?
Simple carbohydrates (like sugar and white flour) can start raising blood sugar within 15-30 minutes. Complex carbohydrates and meals containing fat, fiber and protein will have a slower, more gradual impact, typically peaking 1-2 hours after eating.
Does drinking water help lower blood sugar?
Yes, staying hydrated helps your kidneys flush out excess glucose through urine. While it’s not a treatment for high blood sugar, drinking plenty of water is an important part of overall diabetes management and can help lower blood sugar levels modestly.
What is the main difference between A1C and a daily glucose reading?
A daily glucose reading (from a BGM or CGM) is a snapshot of your blood sugar at that exact moment. An A1C test is a lab value that reflects your average blood sugar control over the past 2-3 months, providing a long-term overview.
Is an A1C of 5.7% good or bad?
An A1C of 5.7% is the threshold for prediabetes. It is not “bad” in the sense of a diabetes diagnosis, but it is a critical warning sign that your blood sugar levels are higher than normal, increasing your risk for developing Type 2 diabetes.
What are the first signs of diabetes to watch for?
The classic early signs are increased thirst, frequent urination, unexplained weight loss and persistent fatigue. However, in Type 2 diabetes, these symptoms can develop slowly over years, or may not be noticeable at all in the prediabetes stage.
How often should I check my blood sugar?
The frequency depends on your condition and treatment. People on insulin may test 4-10 times a day. Those with well-controlled Type 2 diabetes on oral medication might test less often. Always follow the specific recommendations of your healthcare provider.
Conclusion
Understanding and managing your blood sugar levels is one of the most powerful actions you can take for your long-term health. It is a journey of awareness, vigilance, and proactive partnership with your healthcare team.
Key Takeaways from This Guide
- Know Your Numbers: A normal fasting blood sugar is under 100 mg/dL, while a level of 126 mg/dL or higher indicates diabetes. An A1C between 5.7% and 6.4% is a critical prediabetes warning.
- Recognize the Symptoms: Be aware of the signs of high blood sugar (thirst, frequent urination) and low blood sugar (shakiness, sweating), and know how to respond, especially with the “15-15 Rule” for lows.
- Management is Key: Blood sugar management is a pillar of overall health, not just a concern for those with diabetes. Modern tools like CGMs and metrics like Time in Range (TIR) are transforming our ability to maintain control.
- It’s Personal: Optimal blood sugar targets can vary based on age, pregnancy, and overall health. A personalized plan is essential.
The information in this guide is a map, but it is not the journey itself. Your next, most important step is to use this knowledge to have an informed conversation with your healthcare provider.
They can help you understand your personal risk factors, order the appropriate tests, and establish blood sugar goals that are right for you.
Take control of your metabolic health today. Schedule an appointment, ask questions, and become an active participant in your own well-being. Your future self will thank you.
We invite you to share your experiences or ask further questions in the comments section below. Your story could help someone else on their health journey.
Disclaimer: The information provided in this article is for informational and educational purposes only. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.

