Age-Related Macular Degeneration (AMD) is a leading cause of significant, irreversible vision loss among people aged 50 and older.
It damages the macula, the small central portion of the retina responsible for sharp, detailed, straight-ahead vision.
This condition makes it difficult to read, drive, and recognize faces.
According to a landmark study published in JAMA Ophthalmology and highlighted by the Centers for Disease Control and Prevention (CDC), nearly 20 million Americans are living with some form of AMD.
This number underscores the vast public health impact of this progressive disease.
In this comprehensive guide, we will explore the critical differences between dry and wet AMD, its symptoms and stages, key risk factors, the latest evidence-based treatments, and the exciting new research that offers hope for the future.
Understanding this condition is the first step toward protecting your sight. Read on to learn everything you need to know about macular degeneration.
In This Article
What Exactly is Age-Related Macular Degeneration (AMD)?
To truly understand macular degeneration, we must first look at the intricate anatomy of the human eye.
The eye functions much like a camera, capturing light and converting it into electrical signals that the brain interprets as images.
At the very back of the eye lies a thin layer of light-sensitive tissue called the retina.
Think of the retina as the camera’s digital sensor or film.
Nestled in the center of this vital tissue is a tiny, specialized area called the macula.
Though it’s only about 5 millimeters in diameter, the macula is responsible for our sharpest, most detailed central vision.
It’s the “high-definition” center of the retina, packed with photoreceptor cells called cones.
These cells allow us to see fine details, read small print, perceive colors vividly, and recognize the faces of our loved ones.
The Crucial Distinction: Central vs. Peripheral Vision
A key characteristic of Age-Related Macular Degeneration is that it specifically targets the macula.
Consequently, it erodes central vision while leaving peripheral (side) vision largely intact.
This is a critical point: macular degeneration does not cause total blindness.
A person with advanced AMD might not be able to see the face of a person standing directly in front of them, but they would still be able to see the person’s outline and the room around them using their side vision.
This selective loss of vision creates a unique and challenging experience. Imagine looking at a clock and being able to see the numbers around the edge, but not the hands in the middle.
Or trying to read a book where the words in the center of your focus disappear into a blurry or dark spot. This is the daily reality for millions living with advanced AMD.
The Profound Impact on Daily Life
The loss of central vision has a profound and often devastating impact on a person’s independence and quality of life.
The tasks we take for granted become monumental challenges. Here are some examples of how AMD affects daily activities:
- Reading: Words may appear blurry, distorted, or have letters missing, making it difficult to read books, newspapers, medication labels, or recipes.
- Driving: Recognizing road signs, seeing traffic lights clearly, and judging distances become hazardous, often leading to the cessation of driving.
- Recognizing Faces: The inability to see the fine details of a person’s face can be socially isolating, making it hard to connect with friends and family.
- Cooking and Hobbies: Tasks requiring fine detail, such as threading a needle, measuring ingredients, or working on crafts, become frustrating or impossible.
- Navigating New Environments: While peripheral vision helps with general navigation, the inability to read signs or see details can make unfamiliar places daunting.
This erosion of functional vision underscores why understanding, diagnosing, and managing macular degeneration is a critical health priority.
It’s not just about saving sight, it’s about preserving a person’s connection to the world around them.
What is the Difference Between Dry and Wet Macular Degeneration?
While both forms of AMD affect the macula, they are distinct in their cause, prevalence, and progression.
Understanding this difference is fundamental to grasping the nature of the disease and its treatment pathways.
The vast majority of people with Age-Related Macular Degeneration have the “dry” form, but the “wet” form is responsible for the most severe and rapid vision loss.
Dry AMD (Atrophic)
Dry macular degeneration is by far the more common type, accounting for approximately 85-90% of all cases, as noted by the American Academy of Ophthalmology (AAO).
Its name, “atrophic”, refers to the slow thinning and wasting away of the macular tissue over time.
The hallmark of dry AMD is the accumulation of tiny yellow deposits called drusen under the retina.
Drusen are metabolic waste products from the retinal cells. In a young, healthy eye, these waste products are efficiently cleared away.
With age and other risk factors, this clearing mechanism becomes less effective, leading to the buildup of these deposits.
While small, hard drusen are a common part of aging, large, soft drusen are a key indicator of Age-Related Macular Degeneration.
As these drusen accumulate, they disrupt the function of the retinal pigment epithelium (RPE), a crucial layer of cells that nourishes the photoreceptors.
Over years, this disruption leads to the gradual breakdown and death of light-sensing cells in the macula, causing a slow, progressive blurring or dimming of central vision.
The Three Stages of Dry AMD
Dry AMD progresses through three distinct stages, which an eye care professional can identify during a dilated eye exam:
- Early-Stage Dry AMD: In this stage, there are several small drusen or a few medium-sized drusen present. Most people have no symptoms and are unaware they have the condition. Vision is typically unaffected.
- Intermediate-Stage Dry AMD: This stage is characterized by many medium-sized drusen or one or more large drusen. Some people may begin to notice mild symptoms, such as a slight blurriness in their central vision or difficulty seeing in low light. This is the critical stage where nutritional intervention with the AREDS 2 formula is often recommended to slow progression.
- Late-Stage Dry AMD (Geographic Atrophy): In this advanced stage, the thinning of the macula has progressed to cause the death of RPE cells and photoreceptors, creating a well-defined area of atrophy. This results in a significant blind spot, or scotoma, in the central vision. This stage is known as Geographic Atrophy (GA) because the atrophied areas can look like a map to an ophthalmologist.
Wet AMD (Neovascular / Exudative)
Wet macular degeneration is less common, affecting only about 10-15% of people with Age-Related Macular Degeneration – AMD, but it is far more aggressive and is responsible for approximately 90% of all cases of severe vision loss from the disease.
The terms “neovascular” (new vessels) and “exudative” (leaking) perfectly describe its underlying mechanism.
Wet AMD occurs when the body, in a misguided attempt to supply more oxygen and nutrients to the distressed macular tissue, grows new, abnormal blood vessels.
This process is called choroidal neovascularization (CNV). These new vessels originate from the choroid, the layer of blood vessels beneath the retina, and break through the barrier into the space under the macula.
Unlike healthy blood vessels, these new vessels are fragile and leaky.
They ooze blood and fluid into the macula, causing it to swell and lift.
This leakage rapidly damages the photoreceptor cells, leading to a sudden and often dramatic loss of central vision.
Patients may notice a rapid onset of symptoms like severe distortion of straight lines or a large, dark spot in their vision.
A critical point to remember is that wet AMD is always considered late-stage AMD. While dry AMD can progress slowly through its stages, it can also convert to the wet form at any time, particularly in the intermediate stage. This is why regular monitoring is so crucial.
Featured Snippet: Dry AMD vs. Wet AMD at a Glance
To summarize the key differences, here is a comparative table designed for quick understanding.
| Feature | Dry AMD (Atrophic) | Wet AMD (Neovascular) |
|---|---|---|
| Prevalence | ~90% of all AMD cases | ~10% of all AMD cases |
| Primary Cause | Buildup of drusen, leading to thinning (atrophy) of the macula. | Growth of abnormal, leaky blood vessels under the macula (neovascularization). |
| Onset of Vision Loss | Slow and gradual, progressing over many years. | Rapid and sudden, can occur over days or weeks. |
| Key Clinical Sign | Yellow deposits (drusen) visible during an eye exam. | Fluid and blood leakage in the macula, visible on an OCT scan. |
| Common Symptoms | Gradual blurring, need for brighter light, dimming of central vision. | Severe distortion of straight lines (wavy vision), large central blind spots. |
| Progression | Progresses through early, intermediate, and late stages. Can convert to wet AMD. | Is always considered a late-stage, advanced form of AMD. |
What are the Symptoms and Signs of Macular Degeneration?
The symptoms of macular degeneration can be subtle at first, often going unnoticed until the disease has progressed.
Since AMD typically affects older adults, many people mistakenly attribute early signs to normal aging or the need for new glasses.
Awareness of the specific symptoms is key to seeking timely diagnosis and treatment.
Early Warning Signs of AMD
In the early and intermediate stages of dry Age-Related Macular Degeneration – AMD, symptoms may be mild or non-existent, especially if only one eye is affected.
The brain is remarkably good at compensating for vision loss in one eye by relying on the healthier eye.
However, as the disease progresses, the following signs may appear:
- Distortion of Straight Lines (Metamorphopsia): This is one of the most classic and specific symptoms of AMD. Straight lines, such as a door frame, window blinds, or lines on a page, may appear wavy, bent, or crooked. This is caused by fluid or drusen distorting the macula’s smooth surface.
- Increased Need for Bright Light: You may find that you need more and more light for reading or other close-up tasks that you used to perform easily.
- Difficulty Adapting to Low Light: Moving from a bright environment to a dim one (like entering a dimly lit restaurant) may seem to take much longer for your eyes to adjust.
- Blurriness of Printed Words: Text in books, on screens, or on labels may appear smudged or less clear, even with reading glasses.
- Slight Dimming of Central Vision: Your central field of view might seem less bright or intense compared to your peripheral vision.
Late-Stage Symptoms (Advanced Dry or Wet AMD)
As Age-Related Macular Degeneration progresses to its advanced stages (Geographic Atrophy or Wet AMD), the symptoms become much more pronounced and disruptive:
- A Well-Defined Blurry or Blind Spot (Scotoma): A persistent, dark, or empty spot appears in the center of your vision. This is a direct result of damaged or dead photoreceptor cells in the macula. It may start as a small smudge and grow larger over time.
- Decreased Intensity or Brightness of Colors: Colors may appear faded, washed out, or less vivid than they used to.
- Difficulty Recognizing Faces: The central blind spot can make it impossible to see the features of a person’s face, a symptom with significant social and emotional consequences.
The Amsler Grid: A Simple Home Monitoring Tool
The Amsler Grid is a simple but effective tool that can help detect the early signs of AMD, particularly the distortions associated with wet AMD.
It is a grid of horizontal and vertical straight lines with a dot in the center.
People with or at risk for Age-Related Macular Degeneration are often advised to use it daily to monitor their vision.
How to Use the Amsler Grid:
- Wear the glasses you normally use for reading.
- Hold the grid at a comfortable reading distance (about 12-15 inches).
- Cover one eye.
- Look directly at the center dot with your uncovered eye.
- While looking at the dot, pay attention to the lines of the grid. Ask yourself:
- Do any of the lines appear wavy, blurry, or distorted?
- Are there any missing areas or dark spots in the grid?
- Can you see all four corners and all sides of the grid?
- Repeat the test with your other eye.
If you notice any changes, such as new wavy lines or dark spots, you should contact your eye doctor immediately.
This could be a sign of wet AMD, which requires urgent treatment.
Disclaimer: The Amsler Grid is a monitoring tool, not a substitute for a comprehensive eye exam. It can help detect problems, but only an eye care professional can diagnose macular degeneration.
How Do Eye Doctors Diagnose Macular Degeneration?
Diagnosing Age-Related Macular Degeneration – AMD requires a thorough examination by an ophthalmologist or optometrist.
A diagnosis is not made based on symptoms alone but through a series of specific tests that allow the doctor to look directly at the retina and macula and assess their health.
Early and accurate diagnosis is critical for initiating treatment to slow the disease’s progression.
The diagnostic process typically involves the following steps:
- Comprehensive Dilated Eye ExamThis is the cornerstone of any eye health evaluation. The doctor will administer eye drops to dilate (widen) your pupils. This allows a much wider and clearer view of the back of the eye, including the retina, macula, and optic nerve. During this exam, the doctor will look for:
- Drusen: The size, number, and type of drusen are key indicators of the presence and stage of dry AMD.
- Pigmentary Changes: The doctor will look for changes in the retinal pigment epithelium (RPE), such as clumping or loss of pigment, which are signs of macular stress and atrophy.
- Optical Coherence Tomography (OCT)OCT is a revolutionary, non-invasive imaging technology that has become the standard of care for diagnosing and managing AMD. It works like an “ultrasound for the eye”, using light waves to take high-resolution, cross-sectional pictures of the retina. The patient simply rests their chin on a machine and looks at a target for a few seconds. The resulting image provides a detailed, layered view of the macula, allowing the doctor to:
- Detect Wet AMD: OCT is exceptionally sensitive at detecting the fluid and blood that leaks from abnormal vessels in wet AMD, even in microscopic amounts. It can show swelling and separation of retinal layers.
- Monitor Geographic Atrophy (GA): In advanced dry AMD, OCT can precisely measure the thickness of the retina and map the areas of thinning and cell loss (atrophy).
- Track Treatment Response: For patients receiving treatment for wet AMD, regular OCT scans are used to see if the fluid is resolving and the macular swelling is decreasing.
- Fluorescein AngiographyIf wet AMD is suspected based on the dilated exam or OCT scan, the doctor may perform a fluorescein angiogram to confirm the diagnosis and locate the exact source of the leakage. This test involves:
- A special vegetable-based dye (fluorescein) is injected into a vein in the patient’s arm.
- The dye travels through the bloodstream to the blood vessels in the retina.
- A special camera takes a rapid series of photographs as the dye circulates.
Who is Most at Risk for Developing AMD?
While the primary cause of Age-Related Macular Degeneration is related to the aging process, certain factors can significantly increase an individual’s likelihood of developing the disease.
Understanding these risk factors is crucial for both prevention and early detection.
They can be broadly divided into two categories: unmodifiable and modifiable.
Unmodifiable Risk Factors (Things You Cannot Change)
- Age: This is the single greatest risk factor. The disease is rare in people under 50. The risk increases dramatically with each decade of life. According to the National Eye Institute (NEI), about 2% of people in their 50s have AMD, but this rises to nearly 30% for those over age 75.
- Family History and Genetics: AMD has a strong genetic component. If you have a close relative (parent or sibling) with AMD, your risk is significantly higher. Researchers have identified several genes associated with an increased risk of developing the disease.
- Race: Caucasians (people of European descent) have a much higher risk of developing AMD compared to people of African, Hispanic, or Asian descent.
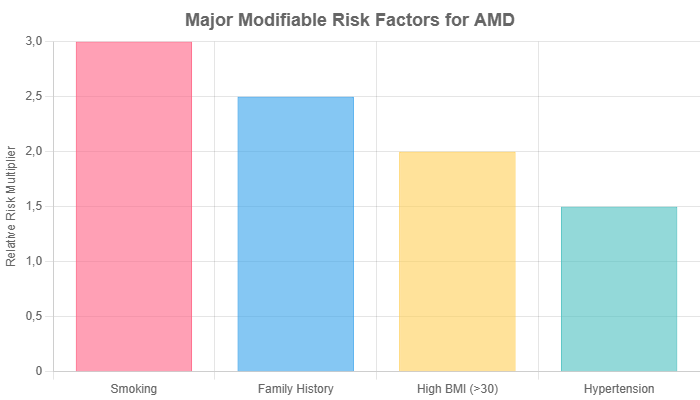
Modifiable Risk Factors (Things You Can Control)
This is where individuals can take proactive steps to lower their risk or slow the progression of the disease.
The connection between lifestyle and eye health is powerful.
- Smoking: This is the most significant and controllable risk factor for macular degeneration. Smokers are two to four times more likely to develop AMD than non-smokers. Smoking generates oxidative stress, damages blood vessels, and reduces the flow of oxygen to the retina. Quitting smoking is the single most important thing you can do to protect your eyes.
- Diet and Nutrition: A diet high in saturated fats, processed foods, and refined carbohydrates is associated with a higher risk of AMD. Conversely, a diet rich in leafy green vegetables (like spinach and kale), colorful fruits, and fish high in omega-3 fatty acids (like salmon) can be protective. These foods contain antioxidants like lutein and zeaxanthin, which are concentrated in the macula.
- Obesity and Cardiovascular Health: High blood pressure (hypertension), high cholesterol, and obesity are all linked to an increased risk of AMD. The health of the tiny blood vessels in the eye is directly related to the health of your entire circulatory system. Maintaining a healthy weight, controlling blood pressure, and managing cholesterol through diet and exercise are beneficial for both your heart and your eyes.
- Sun Exposure: While the link is not as strong as with smoking, some studies suggest that a lifetime of unprotected exposure to the sun’s ultraviolet (UV) and blue light may contribute to the development of Age-Related Macular Degeneration. Wearing sunglasses that block 100% of UV rays and a wide-brimmed hat when outdoors is a sensible precaution.
What is the Current Treatment for Macular Degeneration?
It is essential to begin with a clear statement: currently, there is no cure for age-related macular degeneration.
However, this does not mean nothing can be done.
Over the past two decades, significant advancements have led to highly effective treatments that can slow the progression of the disease, preserve existing vision, and in some cases of wet AMD, even recover some lost sight.
The treatment strategy depends entirely on the type and stage of Age-Related Macular Degeneration.
Treatment for Dry AMD
For early-stage dry AMD, there is no specific medical treatment.
The focus is on risk factor modification (quitting smoking, healthy diet, etc.) and regular monitoring.
However, for intermediate-stage dry AMD, a major breakthrough came from a series of large-scale clinical trials sponsored by the National Eye Institute.
The AREDS/AREDS 2 Formula: A Pillar of Dry AMD Management
The Age-Related Eye Disease Studies (AREDS and AREDS2) were landmark clinical trials that investigated the effect of high-dose antioxidant vitamins and minerals on the progression of AMD and cataracts.
The AREDS2 study found that a specific combination of supplements could reduce the risk of progression from intermediate to advanced Age-Related Macular Degeneration by about 25% over five years.
The recommended AREDS 2 formula contains:
- 500 milligrams (mg) of Vitamin C
- 400 International Units (IU) of Vitamin E
- 10 mg of Lutein
- 2 mg of Zeaxanthin
- 80 mg of Zinc (as zinc oxide)
- 2 mg of Copper (as cupric oxide, to prevent copper deficiency anemia associated with high zinc intake)
Who should take AREDS 2 supplements? It is crucial to understand that these supplements are not a preventative measure for the general public or for people with early-stage AMD. They are specifically recommended for individuals who have:
- Intermediate-stage dry AMD in one or both eyes.
- Late-stage dry AMD (Geographic Atrophy) or wet AMD in one eye, but not the other.
Before starting any supplement regimen, it is vital to consult with an eye doctor to confirm your diagnosis and determine if the AREDS 2 formula is appropriate for you.
These are high-dose supplements and may interact with other medications or conditions.
Treatment for Wet AMD
The treatment landscape for wet AMD has been revolutionized over the past 15 years.
The goal of treatment is to stop the leakage from the abnormal blood vessels, thereby preventing further damage to the macula.
Anti-VEGF Injections: The Standard of Care
The primary treatment for wet AMD is a class of drugs called anti-VEGF agents. VEGF stands for Vascular Endothelial Growth Factor, a protein that the body produces which stimulates the growth of new blood vessels.
In wet Age-Related Macular Degeneration, there is an overproduction of VEGF in the eye, driving the choroidal neovascularization process.
Anti-VEGF drugs work by blocking this protein.
By inhibiting VEGF, these medications cause the abnormal, leaky blood vessels to regress and the fluid in the macula to dry up.
This can stop the progression of vision loss and, in many patients, lead to an improvement in vision.
The drugs are administered directly into the eye via an injection into the vitreous (the gel-like substance that fills the eye).
While the thought of an eye injection can be frightening, the procedure is quick and relatively painless.
The eye is completely numbed with anesthetic drops, and patients typically feel only a slight pressure.
The injections are usually given in a doctor’s office and need to be repeated on a regular basis—initially every month, with the interval potentially extending as the condition stabilizes.
Commonly used anti-VEGF drugs include:
- Avastin (bevacizumab): Originally a cancer drug, it is used “off-label” for Age-Related Macular Degeneration but is highly effective and widely used due to its lower cost.
- Lucentis (ranibizumab): The first drug specifically FDA-approved to treat wet AMD.
- Eylea (aflibercept): A newer agent that may require less frequent injections for some patients.
- Vabysmo (faricimab-svoa): The newest drug in this class, which targets both VEGF and another pathway (Ang-2), potentially offering even longer duration between treatments.
Photodynamic Therapy (PDT)
Before the advent of anti-VEGF drugs, PDT was a primary treatment. It is now used much less frequently, sometimes in combination with anti-VEGF injections for specific types of wet AMD.
PDT involves injecting a light-sensitive drug (verteporfin) into the bloodstream.
When the drug reaches the abnormal vessels in the eye, a special low-power “cold” laser is aimed at the macula to activate the drug, which then closes off the leaky vessels.
What New Research Offers Hope for Future AMD Treatment?
The field of retinal disease is one of the most active areas of medical research.
Scientists and clinicians are relentlessly pursuing new ways to treat AMD more effectively, less invasively, and with longer-lasting results.
This section highlights some of the most promising frontiers in macular degeneration treatment.
New Treatments for Geographic Atrophy (Advanced Dry AMD)
For decades, there was no treatment for the advanced form of dry Age-Related Macular Degeneration, Geographic Atrophy (GA).
This changed dramatically in 2023 with the FDA approval of the first-ever treatments for GA. This represents a monumental step forward.
- Syfovre (pegcetacoplan) and Izervay (avacincaptad pegol): These two new drugs are administered as injections into the eye. They work by targeting a different biological pathway than anti-VEGF drugs. They inhibit the “complement cascade”, a part of the immune system that, when overactive, is believed to contribute to the inflammation and cell death that leads to GA. Clinical trials showed that these drugs can slow the rate of GA lesion growth, though they do not reverse existing damage or restore lost vision. Their approval provides the first tool to slow the progression of this devastating condition.
Gene Therapy: A “One-and-Done” Approach?
One of the biggest challenges for patients with wet AMD is the burden of frequent eye injections.
Gene therapy offers the tantalizing possibility of a one-time treatment that could provide a long-lasting effect.
The concept is to use a harmless, modified virus (typically an adeno-associated virus or AAV) to deliver a gene into the retinal cells.
This gene then instructs the cells to produce their own anti-VEGF medicine continuously.
Several gene therapies are in late-stage clinical trials.
The goal is to create a “bio-factory” inside the eye that produces the therapeutic protein for years, potentially eliminating the need for repeated injections.
As reported by organizations like the BrightFocus Foundation, this is one of the most exciting areas of current research.
Longer-Lasting Treatments and Drug Delivery
Beyond gene therapy, researchers are also developing other ways to reduce the treatment burden. These include:
- Drug-Delivery Implants: A tiny, refillable reservoir can be surgically implanted in the eye. This device, about the size of a grain of rice, slowly releases an anti-VEGF drug over many months, replacing the need for frequent injections with an in-office refill procedure.
- Longer-Acting Drugs: The development of drugs like Vabysmo, which can extend the treatment interval to every three or four months for many patients, is a major step forward. Future research aims to create molecules that are even more durable.
Stem Cell Research: The Frontier of Regeneration
The ultimate goal in Age-Related Macular Degeneration treatment is not just to slow the disease but to reverse the damage by replacing the dead or damaged retinal cells. This is the domain of stem cell research.
Scientists are exploring ways to use stem cells to grow new retinal pigment epithelium (RPE) cells and even photoreceptors in the lab.
These new cells could then be transplanted into the patient’s eye to repopulate the atrophied areas of the macula.
This research is still in its early stages and faces significant challenges, such as ensuring the new cells integrate properly and function correctly.
However, it holds the long-term promise of one day restoring vision that has already been lost to AMD.
How Can You Live a Full Life with AMD-Related Vision Loss?
A diagnosis of Age-Related Macular Degeneration, especially in its advanced stages, can be frightening and emotionally challenging.
The loss of central vision requires significant adjustments, but it does not mean the end of a full and independent life.
A combination of low-vision rehabilitation, adaptive technology, and emotional support can empower individuals to continue pursuing their hobbies and daily activities.
Low Vision Aids and Technology
Low vision rehabilitation specialists can help individuals learn to use their remaining peripheral vision more effectively and introduce them to a wide array of helpful tools.
The principle behind most low-vision aids is magnification and enhanced contrast.
- Magnifiers: These come in many forms, from simple handheld and stand magnifiers to powerful electronic video magnifiers (CCTVs) that display a highly magnified image on a screen.
- Telescopic Lenses: These can be mounted on glasses to help with distance viewing, such as watching television or seeing faces.
- High-Contrast and Large-Print Items: Books, newspapers, keyboards, and playing cards are available in large-print formats. Using black felt-tip pens on white paper can also improve contrast and readability.
- Digital Technology: Modern smartphones, tablets, and computers have powerful built-in accessibility features. These include screen magnification, high-contrast modes, and screen reader software (like VoiceOver on Apple devices) that reads text aloud. Voice commands (like Siri or Google Assistant) can also help with tasks like making calls or sending messages.
Home and Lifestyle Modifications
Simple changes around the home can make a huge difference in safety and independence:
- Lighting: Increasing the amount of task lighting is one of the most effective and simple modifications. Use bright, focused, glare-free lights for reading and other close-up activities.
- Contrast and Organization: Use high-contrast colors to make things stand out. For example, use a dark-colored cutting board for light-colored foods like onions, and a light-colored board for dark foods. Place brightly colored tape on the edges of steps. Keep items organized and in consistent places to make them easier to find.
Support and Mental Health
Adjusting to vision loss is a process that affects not only the individual but also their family.
It is normal to feel anger, frustration, and grief. Seeking support is a sign of strength.
- Low-Vision Specialists: These professionals are trained to help people adapt to vision loss and can provide invaluable training and resources.
- Support Groups: Connecting with others who are going through a similar experience can be incredibly helpful. It provides a space to share frustrations, exchange tips, and realize you are not alone. Organizations like the American Macular Degeneration Foundation (AMDF) and local chapters of the Lighthouse Guild offer support groups and resources.
- Mental Health Professionals: If feelings of depression or anxiety become overwhelming, talking to a counselor or therapist can provide coping strategies and support.
Frequently Asked Questions About AMD
1. Can macular degeneration be cured?
No, there is currently no cure for Age-Related Macular Degeneration. However, treatments for both wet and dry AMD can significantly slow the disease’s progression, preserve existing vision, and help manage symptoms to maintain a high quality of life.
2. Will I go completely blind from AMD?
No. AMD affects central vision but does not cause total blindness because it does not damage your peripheral (side) vision. Even in the most advanced cases, individuals retain their side vision, which is crucial for navigation and general awareness.
3. How fast does macular degeneration progress?
The progression rate varies greatly. Dry AMD typically progresses very slowly over many years. Wet AMD, however, can cause rapid and severe vision loss in a matter of weeks or months if left untreated, which is why prompt diagnosis is critical.
4. Can I prevent macular degeneration?
You cannot completely prevent AMD, especially if you have strong genetic risk factors. However, you can significantly lower your risk by not smoking, eating a healthy diet rich in leafy greens and fish, maintaining a healthy weight, and protecting your eyes from UV light.
5. Are the eye injections for wet AMD painful?
The procedure is designed to be as comfortable as possible. The eye is thoroughly numbed with powerful anesthetic drops before the injection. Most patients report feeling only a brief moment of pressure, not sharp pain. The fear is often worse than the actual experience.
6. Should I take AREDS 2 vitamins?
AREDS 2 vitamins are only recommended for people with intermediate-stage AMD or late-stage AMD in one eye. They are not for prevention in the general public or for those with early-stage disease. Always consult your eye doctor before starting these high-dose supplements.
7. Can you have both wet and dry AMD at the same time?
Yes. Wet AMD always arises from pre-existing dry AMD. A person can have late-stage wet AMD in one eye and intermediate-stage dry AMD in the other. An eye being treated for wet AMD still has the underlying characteristics of dry AMD.
8. Does cataract surgery make Age-Related Macular Degeneration worse?
This is a complex and debated topic. Most large-scale studies have not found a definitive link showing that modern cataract surgery worsens Age-Related Macular Degeneration. For patients with significant cataracts and AMD, the visual benefit of removing the cloudy lens often outweighs the potential risks.
9. What is the difference between macular degeneration and glaucoma?
They are two different diseases. Macular degeneration damages the macula, causing loss of central vision. Glaucoma damages the optic nerve, typically causing a gradual loss of peripheral (side) vision first. Both can lead to significant vision loss if not managed.
Conclusion
Age-related macular degeneration is a complex and common condition that poses a significant threat to the vision and independence of millions of older adults.
However, our understanding and ability to manage the disease have grown exponentially. The most critical takeaways are:
- AMD damages the macula, leading to the loss of sharp, central vision needed for reading and driving.
- There are two forms: the common, slow-progressing dry AMD and the less common but more aggressive wet AMD.
- Early detection is paramount. Regular comprehensive eye exams are the best defense, especially for those over 50 or with known risk factors like a family history or a history of smoking.
- Effective treatments exist. AREDS 2 supplements can slow intermediate dry AMD, and anti-VEGF injections are highly effective at controlling wet Age-Related Macular Degeneration and preserving sight.
- New research, including treatments for Geographic Atrophy and gene therapy, offers incredible hope for even better outcomes in the future.
Your Next Step
The single most important action you can take for your eye health is to be proactive. If you are over the age of 50, have risk factors for AMD, or have noticed any changes in your central vision—no matter how subtle—do not wait.
Schedule a comprehensive dilated eye exam with an ophthalmologist or optometrist. It is a simple, painless step that could save your sight.
Do you have experience with Age-Related Macular Degeneration or a question we didn’t cover? Share your thoughts below to help others in the community.
References
- Prevalence of Age-Related Macular Degeneration in the United States. Centers for Disease Control and Prevention (CDC).
- Age-Related Macular Degeneration (AMD). National Eye Institute (NEI).
- What Is Macular Degeneration? American Academy of Ophthalmology (AAO).
- Age-Related Eye Disease Studies (AREDS/AREDS2). National Eye Institute (NEI).
- Macular Degeneration: Facts & Figures. BrightFocus Foundation.
- American Macular Degeneration Foundation (AMDF).

